Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.8 no.4 Joinville Out./Dez. 2011
CASE REPORT ARTICLE
Eosinophilic ulcer of the lateral tongue: case report
Marcelo Gadelha VasconcelosI; Lélia Batista de SouzaI; Éricka Janine Dantas da SilveiraI; Ana Myriam Costa de MedeirosI; Marianne de Vasconcelos CarvalhoII; Lélia Maria Guedes QueirozI
I Post-Graduate Program, Oral Pathology, Dentistry Department, Federal University of Rio Grande do Norte – Natal – RN – Brazil
II Post-Graduate Program, Department of Oral Diagnosis, Piracicaba Dental School, University of Campinas – Piracicaba – SP – Brazil
ABSTRACT
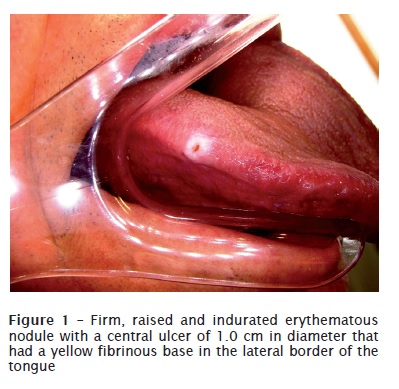
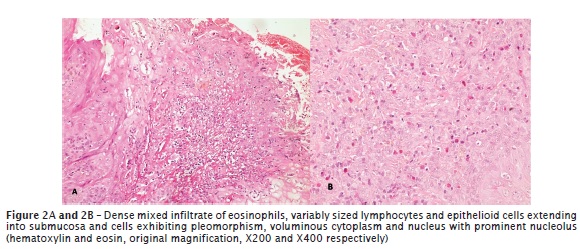
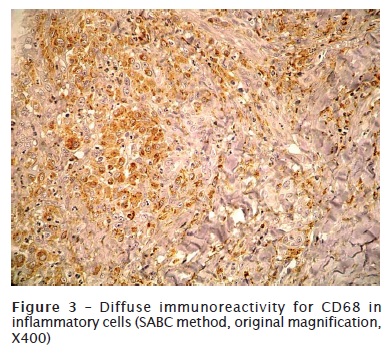
Introduction: Eosinophilic ulcer of the oral mucosa (EUOM) is a lesion manifesting as ulcer with elevated margins. The lesion is self-limiting and develops rapidly usually disappearing after several weeks. The exact pathogenetic mechanisms implicated in its development are poorly understood, however, the possibility that trauma may play a role has been often postulated. Case report: A 63 year-old male patient had presented whit a chief complaint of painful ulcerated nodule on the tongue. Oral examination revealed a firm, raised and indurated erythematous nodule with a central ulcer that had a yellow fibrinous base. Clinical diagnosis hypothesis was either traumatic ulcer or oral squamous cell carcinoma. Histopathologic analysis revealed an ulcerated lesion with a dense mixed infiltrate of eosinophils, variably sized lymphocytes and epithelioid cells extending into submucosa. These cells exhibited pleomorphism, voluminous cytoplasm and nucleus with prominent nucleolus and were identified by immunohistochemical method as CD68+ cells. The histological diagnosis was EUOM. At 1-year follow-up there was no recurrence. Conclusion: Our case provides useful information on clinical and pathological features, diagnosis, treatment, and prognosis of EUOM, as suggesting the possible etiology of this uncommon lesion because it is poorly described in the literature.
Keywords: ulcer; mucous membrane; tongue.
Introduction
Eosinophilic ulcer of the oral mucosa (EUOM) is considered to be a reactive lesion with a benign clinical course. EUOM has been known by different terms, including, eosinophilic ulcer, eosinophilic granuloma of tissue, traumatic granuloma, atypical histiocytic granuloma and traumatic ulcerative granuloma with stromal eosinophilia. In infants it has been called as Riga-Fed disease 4,7,13.
The etiology of EUOM remains obscure, although injury has been considered to play a major role 1,5,10.
EUOM is most frequently diagnosed in patients aged 30-50 years, but also occurs in infants as well as elderly people. Sex distribution is equal or slightly more elevated in females and more than half of the lesions occur on the tongue. Others locations are the lips, buccal mucosa, palate, gingival and floor of the mouth 10,11. The lesion usually manifests as a rapidly developing solitary ulcer, from few millimeters to several centimeters in diameter, with elevated and indurated borders arising in the oral cavity 7,10. The lesion may show a peripheral erythema, a white or yellowish base and fibrinous membrane on the surface. Lesions may be asymptomatic or extremely painful and can mimic oral cancer clinically 6,13.
Microscopically, there is a polymorphic inflammatory infiltrate extending deep into the submucosa, underlying muscle and salivary glands. Numerous eosinophils and large histiocytic cells with pale nuclei and frequent mitoses, in some instances showing a pseudolymphomatous aspect, are characteristic 8. Others components of the infiltrated include lymphocytes, plasma cells, granulocytes and mast cells and occasionally it is misdiagnosed as lymphoma on microscopic examination 4,7,12.
EUOM is generally a self-limiting disorder that tends to resolve spontaneously in a few weeks 6,11. Many different therapeutic approaches for EUOM have been reported in literature. The most frequently performed therapy is surgical excision 1,5. This approach seems to be especially indicated in cases with persistent lesions. No further local recurrences are usually noted after excision. Topical steroids or mouthwashes can be also prescribed. Other therapeutic modalities include intralesional or oral corticosteroids, topical antibiotics, curettage and cryotherapy 5,8.
We report a rare case of eosinophilic ulcer of the oral mucosa, emphasizing the clinic and histopathological aspects that are relevant for the diagnosis and treatment of this pathology. Additionally, we demonstrate the importance of the disease's knowledge and its course.
Case report
A 63 year-old male patient had presented whit a chief complaint of painful ulcerated nodule on the right side of the tongue that had developed within 1 month. Patient had severe pain that disturbed his eating and. stated that his tongue had been quite traumatized for amalgam restoration. There was no palpable cervical lymphadenopathy, patient was in good health and his past medical history was unremarkable. Full blood count and VDRL results were normal and negative, respectively. Oral examination revealed a firm, raised and indurated erythematous nodule with a central ulcer of 1.0 cm in diameter that had a yellow fibrinous base (figure 1). Clinical diagnosis hypothesis was either traumatic ulcer or oral squamous cell carcinoma. A section from an excisional biopsy of the lesion was stained with hematoxylin and eosin. Histopathological analysis revealed an ulcerated lesion with dense mixed infiltrate of eosinophils, variably sized lymphocytes and epithelioid cells extending into submucosa (figure 2A and 2B). These cells exhibited pleomorphism, voluminous cytoplasm and nucleus with prominent nucleolus. These cells were identified by immunohistochemical method as CD68+ cells (figure 3). The histological diagnosis was eosinophilic ulcer of the tongue. At 1 year follow up there was no recurrence.
Discussion
Eosinophilic ulcer of the oral mucosa was first described in adults by Popoff in 1956 4. First reports in the 1960s included this process within the spectrum of granuloma faciale and some authors proposed the term ulcerated granuloma eosinophilicum diutinum of the tongue 4,11. In 1970, this lesion was proposed as a distinct entity by Shapiro and Juhlin 12. Since then, different names have been used to define this process 7,11.
According to Segura and Pujo 11 the aetiology of EUOM remains obscure, although most authors suggest that the lesions are of traumatic origin, caused by accidental bites or by repeated thrusting against sharp, misplaced or fractured teeth. Vélez et al. 13 have suggested that trauma is only a contributing factor in the development of EUOM and could lead to viral or toxic agents entering the underlying tissue to cause an inflammatory response. The increased incidence of this lesion on the tongue, which is easily exposed to trauma through mastication, and the definitive history of traumatic injury in one-third to one-half of reported cases agree with this hypothesis 1,4,13. In our case, the course of ulcer was a defective amalgam restoration.
Clinically, EUOM usually manifests as a rapidly developing solitary ulcer, from few millimeters to several centimeters in diameter, with elevated and hard borders arising in the oral cavity mainly in tongue (lateral and dorsal surfaces), as related in this present case 1,8,11. Pain was reported by our patient and according to Vélez et al. 13 and Alobeid et al. 2 it can be associated in a variable proportion of cases (17% to 100%).
It is reported that EUOM exhibits a slight female predominance in most of the cases with a peak incidence between the sixth and seventh decades of life 5,11. In our case, EUOM occurred in this decade of life, however, in a male patient.
Mezei et al. 6 reported that multiple EUOMs may be observed. Also, this lesion shows a bimodal age distribution, with the first peak occurring at early childhood and the second during the fiftieth decade of life. Our patient showed a single lesion in tongue's lateral border without associated internal disease as reported by Mezei et al. 6.On the other hand, El-Mofty et al. 3 related that in extremely rare cases, association with enlarged regional lymph nodes may occur.
Microscopically, under an ulcerated mucosa, a poorly formed granulation tissue showing an increased number of capillaries with prominent endothelial cells is usually observed. A dense diffuse submucosal polymorphous inflammatory infiltrate involving occasionally the overlying epithelium is usually noted. This infiltrate tends to extend to the deeper underlying soft tissue, muscle fibers and salivary glands 2,10,11. The inflammatory infiltrate is composed of small round lymphocytes, abundant polymorphonuclear eosinophils and other inflammatory cells (neutrophils, plasma cells and histiocytes). Large mononuclear cells with round to ovoid pale nuclei, showing occasional nuclear atypia, intermingled in the inflammatory infiltrate are also frequently observed 2,4. In this present case, we observed some of these aspects. Nevertheless, we also performed the immunohistochemical method and observed that epithelioid cells were positive for anti-CD68, defining these cells as macrophages and not as neoplasic cells.
As most traumatic oral ulcers are devoid of eosinophils, several hypotheses have been proposed to explain the prominent eosinophilic infiltrates observed in this lesion. A possible direct pathogenic role of cytokine and chemotactic factors released by eosinophils in the development of EUOM has been hypothesized. A possible interaction among mast cells, release of eosinophil chemotactic factors and tissue eosinophilia has also been postulated 11. Infiltrate containing T lymphocytes suggests that cell-mediated immunity may play an important role in the lesion pathogenesis 3. However, if eosinophils and mast cells would either play a major pathogenic role or be present as a result of T lymphocyte recruitment is not yet clear. The histogenesis of eosinophilic ulcer of the oral mucosa remains controversial. Immunophenotypic studies have shown that the infiltrate containing large atypical cells have a myofibroblastic or histiocytic origin 9.
Regezi et al. 9 studied eight cases of EUOM and demonstrated that the large mononuclear cells were positive for macrophage marker CD68, as showed in this present case, or dendrocyte marker factor XIII, with a few submucosal S100-positive cells. El-Mofty et al. 3, in a report of 38 cases of EUOM, studied nine representative cases immunohistochemically and demonstrated that the atypical large cells were positive only for vimentin and lacked expression of all lymphoid and histiocytic markers, suggesting that they may represent myofibroblasts. Ficarra et al. 4 described the first case where a proliferation of CD30+ atypical large mononuclear cells was identified, leading to the conclusion that EUOM could be included within the spectrum of CD30+ lymphoproliferative disorders. More recently, Alobeid et al. 2 reported three additional cases of EUOM also containing CD30+ atypical cells. In one of the patients skin nodules followed the oral lesion. PCR analysis showed a monoclonal rearrangement of the TCR-c chain gene in all lesions and in the patient with skin lesions the same rearrangement was demonstrated in both oral and cutaneous specimens. The authors concluded that these cases with CD30+ atypical lymphocytes may represent a subset of EUOM that is probably a heterogeneous category of disorders.
Spontaneous healing usually occurs within 1 month, but may rarely take as long as 8 months 6. An incisional biopsy is often required for definitive diagnosis when no evidence of spontaneous healing is observed at 1-month follow up 5. Surgical excision is the most commonly cited treatment as shown by Ada et al. 1. In our case, the lesion persisted for more 1 month, thus an excisional biopsy was the most appropriate diagnostic and therapeutic choice. Topical steroids or mouthwashes can be prescribed, despite there being no conclusive evidence of its efficacy. Mezei et al. 6 related that other therapeutic modalities include intralesional steroids and topical antibiotics, curettage and cryotherapy.
No further local recurrences are usually noted after excision, however according to Segura and Pujol 11, development of new lesions in other mucosal sites may occur but in our case at 1 year follow up there was no recurrence and an excisional biopsy showed to be a good choice of treatment.
Conclusion
Our case is of interest because provides useful information on clinical and pathological features, diagnosis, treatment, and prognosis of EUOM, as well as suggesting the possible etiology of this uncommon lesion. We reinforce that recurrent trauma may either lead to an alteration in tissue antigens or introduce microbial products into the tissues, initiating a local immune reaction which would cause EUOM.
References
1. Ada S, Seckin D, Tarhan E, Buyuklu F, Cakmak O, Arikan U. Eosinophilic ulcer of the tongue. Australas J Dermatol. 2007 Nov;48(4):248-50. [ Links ]
2. Alobeid B, Pan LX, Milligan L, Budel L, Frizzera G. Eosinophil-rich CD30+ lymphoproliferative disorder of the oral mucosa. A form of "traumatic eosinophilic granuloma". Am J Clin Pathol. 2004 Jan;121(1):43-50.
3. El-Mofty SK, Swanson PE, Wick MR, Miller AS. Eosinophilic ulcer of the oral mucosa. Report of 38 new cases with immunohistochemical observations. Oral Surg Oral Med Oral Pathol. 1993 Jun;75(6):716-22.
4. Ficarra G, Prignano F, Romagnoli P. Traumatic eosinophilic granuloma of the oral mucosa: a CD30+(Ki-1) lymphoproliferative disorder? Oral Oncol. 1997 Sep;33(5):375-9.
5. Gao S, Wang Y, Liu N, Li S, Du J. Eosinophilic ulcer of the oral mucosa: a clinicopathological analysis. Chin I Dent Res. 2000 May;3(1):47-50.
6. Mezei MM, Tron VA, Stewart WD, Rivers JK. Eosinophilic ulcer of the oral mucosa. J Am Acad Dermatol. 1995 Nov;33(5 Pt 1):734-40.
7.Misterska M, Dmochowski M, Szulczynska-Gabor J, Walkowiak H, Bowszyc-Dmochowska M, Kaczmarek J et al. Eosinophilic ulcer of the oral mucosa: report of a child with CD30-negative cells in an infiltration on the lower lip. Med Sci Monit. 2010 Aug 1;16(8):CS95-9.
8. Nikitakis NG, Brooks JK. Persistent tongue ulcer. Eosinophilic ulceration. Gen Dent. 2010 Mar-Apr;58(2):150-3.
9. Regezi JA, Zarbo RJ, Daniels TE, Greenspan JS. Oral traumatic granuloma. Characterization of the cellular infiltrate. Oral Surg Oral Med Oral Pathol. 1993 Jun;75(6):723-7.
10. Ribeiro AL, Oliveira Mendes FR, Alves Jr SD, Pinheiro JD. Eosinophilic ulcer: the role of stress-induced psychoneuroimmunologic factors. Oral Maxillofac Surg. 2010 Jul;14. [Epub ahead of print].
11. Segura S, Pujol RM. Eosinophilic ulcer of the oral mucosa: a distinct entity or a non-specific reactive pattern? Oral Dis. 2008 May;14(4):287-95.
12. Shapiro L, Juhlin EA. Eosinophilic ulcer of the tongue report of two cases and review of the literature. Dermatologica. 1970;140(4):242-50.
13. Vélez A, Alamillos FJ, Dean A, Rodas J, Acosta A. Eosinophilic ulcer of the oral mucosa: report of a recurrent case on the tongue. Clin Exp Dermatol. 1997 May;22(3):154-6.
 Correspondence:
Correspondence:
Marcelo Gadelha Vasconcelos
Avenida Praia dos Búzios, n.º 9.067 – Ponta-Negra
CEP 59092-200 – Natal – RN – Brasil
E-mail: marcelo.vasconcelos@yahoo.com.br
Received for publication: December 20, 2010
Accepted for publication: January 31, 2011













