Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.9 no.1 Joinville Jan./Mar. 2012
Case Report Article
Misdiagnosis of lip squamous cell carcinoma
Fabiano de Sant'Ana dos Santos I; Miguel Alfredo Isper I; José Pereira Novo-Neto I; Antonio Carlos Marqueti I; Cintia Piccolo Pereira I; Felipe Gai Isper I
I University Center of Educational Foundation of Barretos – Barretos – SP – Brazil.
ABSTRACT
Introduction : Lip squamous cell carcinoma is a malignant lesion of aggressive behavior, which must be recognized by health professionals to prevent damage to patient's health.Objective:To present incisional biopsy importance as an effective clinical approach for the diagnosis of lip squamous cell carcinoma and actinic cheilitis malignancy as well as the professional's lack of knowledge on these two diseases. Case report:The patient was under medical treatment due to be positive for human immunodeficiency virus and because of the actinic cheilitis on lower lip. Because the patient did not observe the labial lesion regression, he searched for the School of Dentistry of the University Center of the Educational Foundation of Barretos, where he underwent biopsy. This procedure confirmed the diagnosis of lip squamous cell carcinoma. The patient was referred for treatment in a specialized cancer center and has been living with the cancer consequences. Conclusion:The physician and dentist must be aware of the main clinical features of lip squamous cell carcinoma so that they can establish its correct diagnosis and early treatment.
Keywords: oral cancer; oral squamous cells carcinoma; diagnosis; Dentistry.
Introduction
Oral cancer affects lips and oral cavity. In Brazil, the number of new cases of oral cancer estimated for 2010 is 14,120 (10,330 males and 3,790 females), occupying the seventh position among all cancer types. Data of 2007 demonstrated that the number of deaths by this disease was 6,064 (4,814 males and 1,250 females).
Lip cancer is most common in Caucasians, aging above 40 years-old, most frequently occurring in lower lip 3,4,14. Lip cancer is the most frequent malign lesion of oral cavity, constituting 15% of oral cavity cancers. Lower lip cancer is twenty times more prevalent than upper lip 6,7. Lip cancer initiates as a chronic process and the continuous exposure to sunlight favors the development of a potentially precancerous lesion, so-called actinic cheilitis (AC) that generally can be transformed into epidermoid carcinoma (EC). This malign neoplasia's synonyms are squamous cells carcinoma, squamous-cellular carcinoma and spinous cellular carcinoma. In Brazil, lip cancer is of great importance because we live in a tropical country whose economy is based on rural activities in which the workers are exposed to sunlight for longer periods 8,9,11,12.
Studies describing oral cancer are of great complexity and health professional's lack of knowledge and resources are highlighted as well patient's fear of suffering prejudice. These complications are harmful, delaying the diagnosis and treatment and worsening the disease's prognosis. This disease's medical treatment is surgery or radiotherapy 5.
The aim of this study was to report the importance of incisional biopsy as an effective clinical approach to lip EC as well as to present the AC malignancy and the professional's misdiagnosis of these two pathologies.
Case report
A Caucasian male alcoholic patient, aging 55 years-old, working as a foreman, was referred to the Service of Oral Diagnosis and Surgery of the School of Dentistry of the University Center of the Educational Foundation of Barretos (short UNIFEB), Sao Paulo. He complained about an ulcerous lesion on lower lip. During anamnesis, patient reported that he had been undergoing a medical treatment and using antiretroviral drugs for human immunodeficiency virus (HIV), at daily basis. Also, he revealed that he had been using a dermatologic cream (Noskote®, Mantecorp, São Paulo, SP) for treating a labial lesion. This product was prescribed by the dermatologist of the Health Basic Unit from his neighborhood, who was following-up this lesion for more than two years. The patient showed to the dentist two recent lip biopsy reports whose histopathological result was AC. The patient also informed that he last dermatologist's appointment had been 10 days ago. After the patient signed a free and clarified consent form, he was submitted to clinical examination where we observed that the lesion occupied at least 50% of the lower lip. The lesion has a fissured aspect with red and white spots and yellow and dry crusts (figure 1). By touching the lesion, we verified its hard aspect and sublingual, submandibular and cervical lymphoadenomegaly. At this clinical procedure, patient complained of mild pain. This symptomatology occurred sporadically to speak, chew, and swallow. The patient presented poor oral hygiene and severe halitosis. We also observed the presence of chronic periodontal disease and the partial absence of the posterior teeth. No prosthesis had been used.
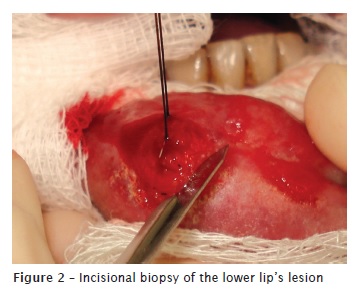
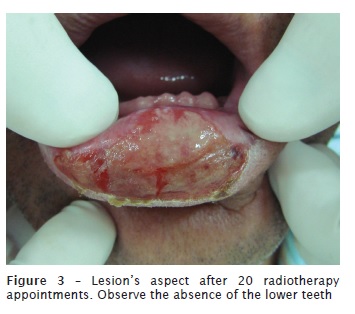
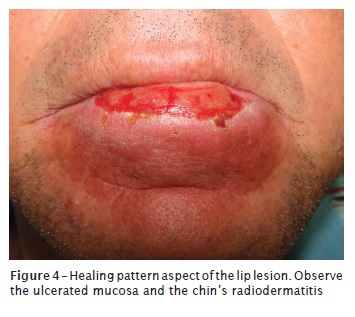
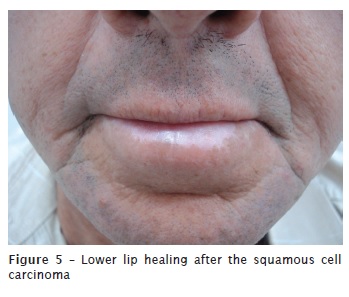
Even with the two aforementioned biopsy reports, we executed a new incisional biopsy at that first appointment (figure 2). The surgical piece was referred to the Service of Oral Pathology of UNIFEB. Histopathologic analysis was well-differentiated acantholytic squamous cell carcinoma. The patient was immediately referred to the Cancer Hospital of Barretos, Sao Paulo. The tumor clinical staging was T1N0M0. The patient's lower teeth were extracted due to medical instructions. The treatment comprised 20 radiotherapy appointments, at every 10 days (figure 3). Three months after the radiotherapy, the patient showed the following side-effects: disfagia, loss of taste, smell and xerostomia. The lip exhibited an ulcerated aspect and the chin showed radiodermatitis (figure 4). Twelve months after the diagnosis, the patient still presented mild radiodermatitis, lack of beard on the chin, cicatricial fibrosis and the recovering oral mucosa (figure 5). Patient will be annually followed-up by the Dentistry Department of The Cancer Hospital of Barretos.

Discussion
This clinical report's patient is at risk for lip EC. Costa et al. 7 conducted a study on 120 patients' files presenting oral EC treated in a hospital of Natal, RN, Brazil and verified this disease predominance in men above 50 years-old, observing that lip lesions were more frequent in patients exposed to sun. These data corroborated those found by other authors 6,14,16. Santos et al. 16 analysed oral cancer epidemiological profile in Alagoas (Brazil) and reported higher frequency of lip EC in women. It is believed that such result may be associated to the fact that in this area, women are more exposed to sun to work, aiming to increase their family income.
This present study is important because reported a clinical case in which the patient had been continuously treated by the Brazilian public health. The fact that the patient had been exhibiting a precancerous lesion (AC) for more than two years on the lower lip, which had been treated with a cosmetic cream, draw our attention. Another noticeable fact was that the results of the previous biopsies showed the presence of atypical epithelial lesions. It is known that when this occurred, the recommended approach is the total removal of the precancerous lesion. It is a literature consensus that this aforementioned approach would prevent lip EC 9,11. Notwithstanding, we detected in time the patient's lip squamous cell carcinoma, allowing his referral and treatment in a specialized hospital.
Studies have drawn attention for the professional lack of prepare in detecting oral cancer as well as for the detection of failures in filling in the patient's files exhibiting this disease 13,16,18. It is understood that any health professional is responsible to diagnose or refer, urgently, doubtful cases which may put the patient's life at risk. Also, the maintenance and updating of the patient's health information is of great importance. This entire situation shows a deficiency in the access and quality of the Brazilian public health services. Therefore, we believe that this could be improved if the Brazilian public health policies (national, state, and municipal) established the planning of preventive and controlling measurements for oral cancer as well as other ways of treatment or therapeutic assistance, according to what has been already proposed 2,17.
In a descriptive study on the Campaign of Prevention and Early Diagnosis of Oral Cancer conducted in Sao Paulo (April, 2004) and coordinated by the Technical Center of Oral Health of the State Health Department, it was verified the lack of resolutivity 1. Consequently, the results of the aforementioned study reinforce that there is a need of more investments in campaigns for prevention and instruction of oral cancer in Brazil.
Although the lip EC reported here was at the initial phase, it can be affirmed that its diagnosis was late, mainly because patient was under professional treatment. It is highlighted that this type of disease, even at its initial phases, leaves sequelae 15. Although the patient did not report fear of the diagnosis, he was very concerned about his treatment. Radiotherapy aims the destruction of the precancerous lesions; however, it is known that normal cells are also damaged. Frequently, patients show side-effects within oral cavity during treatment, similarly to those observed in this case report's patient. The patient exhibited xerostomia, among other side-effects, condition that have been largely discussed in other studies 19. Post-radiotherapy late reactions described by Lopes et al. 10 are: mandibular osteoradionecrosis, mucosa's ulceration, trismus, tooth caries, endocrine dysfunction, larynx's edema, mucosa's necrosis, and cicatricial fibrosis. This latter was seen by this study.
Conclusion
According to this case report, it can be concluded:
Biopsy is a simple, low-cost procedure of great importance in the detection of lesions as AC and lip EC;
AC is a lesion which if not correctly treated can lead to lip EC development;
Some professionals still did not know the precancerous potential of AC in lip EC.
Acknowledgements
We thank to Hélio Massaiochi Tanimoto, PhD – Professor of the Diagnosis and Surgery Discipline of UNIFEB and Head of the Department of Dentistry of Cancer Hospital of Barretos – Pio XII Foundation; Dr. Raphael Carlos Comelli Lia, PhD and Renata Hebling Marins, Msc – Heads of the Service of Pathology of the University Center of the Educational Foundation of Barretos – UNIFEB.
References
1. Antunes JLF, Toporcov TN, Wünsch-Filho V. Resolutividade da campanha de prevenção e diagnóstico precoce do câncer bucal em São Paulo, Brasil. Rev Panam Salud Publica. 2007;21(1):30-6. [ Links ]
2. Araújo Filho VJF, De Carlucci JD, Sasaki SU. Perfil da incidência do câncer oral em um hospital geral em São Paulo. Rev Hosp Clín Fac Med São Paulo. 1998;55(3):110-3.
3. Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Instituto Nacional de Câncer. Coordenação de Prevenção e Vigilância de Câncer. Estimativas 2010: incidência de câncer no Brasil. Rio de Janeiro: INCA; 2009.
4. Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Instituto Nacional de Câncer. Coordenação de Prevenção e Vigilância de Câncer. Estimativas 2008: incidência de câncer no Brasil. Rio de Janeiro: INCA; 2007.
5. Brener S, Jeunon FA, Barbosa AA, Grandinetti HAM. Carcinoma de células escamosas bucal: uma revisão de literatura entre o perfil do paciente, estadiamento clínico e tratamento proposto. Rev Bras Cancer. 2007;53(1):63-9.
6. Champion R, Burton J, Ebling F. Rook's textbook of Dermatology. 5. ed. Oxford: Blackwell Scientific Publications; 1992.
7. Costa ALL, Pereira JC, Nunes AAF, Arruda MLF. Correlação entre a classificação TNM, gradação histológica e localização anatômica em carcinoma epidermóide oral. Pesqui Odontol Bras. 2002;16(3):216-20.
8. Jitomirski F. Câncer bucal. In: Pinto VG. Saúde bucal coletiva. São Paulo: Santos; 2000. p. 445-56.
9. Kaugars GE, Pillion T, Svirsky JA, Page DG, Burns JC, Abbey LM. Actinic cheilitis: a review of 152 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Oral Endod. 1999;88:181-6.
10. Lopes AM, Coletta RD, Alves FA, Abbade N, Rossi Junior A. Reconhecendo e controlando os efeitos colaterais da radioterapia. Rev Assoc Paul Cir Dent. 1998;52(3):241-4.
11. Martins MD, Marques LO, Martins MAT, Bussadori SK, Fernandes KPS. Queilite actínica: relato de caso clínico. Conscientiae Saúde. 2007;6(1):105-10.
12. Neville BW, Day TA. Oral cancer and precancerous lesions. CA Cancer J Clin. 2002;52(4):195-215.
13. Oliveira EF, Silva OMP, Blachman IT, Poi MRB. Perfil epidemiológico das neoplasias orais malignas no município de São Paulo, Brasil. Rev Odontol Unesp. 2005;34(4):141-7.
14. Parkin DM, Pisani P, Ferlay J. Estimates of the worldwide incidence of 25 major cancers in 1990. Int J Cancer. 1999;80:827-41.
15. Santos FS, Tanimoto HM, Isper MA, Isper FG, Andrade RB. Carcinoma espinocelular invasivo de boca – relato de caso. Rev ABO Nac. 2010;18(1):59-62.
16. Santos LCO, Cangussu MCT, Batista OM, Santos JP. Câncer bucal: amostra populacional do estado de Alagoas em hospital de referência. Braz J Otorhinolaryngol. 2009;75(4):524-9.
17. Sassi LM, Oliveira BV, Pedruzzi PAG, Ramo GHA, Stramandinoli RT, Gugelmin G et al. Carcinoma espinocelular de boca em paciente jovem: relato de caso e avaliação dos fatores de risco. RSBO. 2010 Mar;7(1):105-9.
18. Scully C, Porter S. ABC of oral health: Oral cancer. BMJ. 2000;321:97-100.
19. Spolidorio DMP, Spolidorio LC, Barbeiro RH, Höfling JF, Bernardo WLC, Pavan S. Quantitative evaluation of Streptococcus mutans and Candida sp and salivary factors in the oral cavity of patients submitted to radiotherapy. Pesqui Odontol Bras. 2001;15(4):354-8.
 Correspondence:
Correspondence:
Fabiano de Sant'Ana dos Santos
Av. 27, n.º 931 – Centro
CEP 14780-340 – Barretos – SP – Brasil
E-mail:fabiano@feb.br / fss@uol.com.br
Received for publication: December 17, 2010.
Accepted for publication: May 16, 2011.













