Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.9 no.2 Joinville Abr./Jun. 2012
Original Research Article
Assessment of preload in carbon coated prosthetic screws
Dilcele Silva Moreira Dziedzic I; Juliane Nhata II; Vanessa Helena Jamcoski III; Maurício Dziedzic IV
I Department of Dentistry, Positivo University – Curitiba – PR – Brazil.
II Department of Dentistry, University of Ribeirão Preto – Ribeirão Preto – SP – Brazil.
III Latin American Institute of Research in Dentistry – Curitiba – PR – Brazil.
IV Graduate Program in Environmental Management, Positivo University – Curitiba – PR – Brazil.
ABSTRACT
Introduction : The mechanical aspects of tightening screws over implants are important to ensure a successful prosthetic rehabilitation. Screw loosening is a common problem that can be avoided with passive adaptation of the components and an increased tensile force developed in the screw, a preload. Objective: This in vitro study evaluated the effect on preload of a carbon lubricant deposited on the surface of titanium alloy prosthetic screws: conventional Ti6Al4V and surface enhanced. Material and methods: Conventional titanium alloy prosthetic (n = 7) and carbon coating surface enhanced screws (n = 7) were compared. Each prosthetic screw supporting a metallic UCLA over an implant was tightened with the manufacturers recommended torque of 32 N.cm. The removal torque values, recorded for ten consecutive cycles of tightening and removal, were used to estimate the preload. Implant blocks were then sectioned and the interfaces were observed by light microscopy.Results: The lowest removal torque, and consequently the highest preload values, was achieved for the lubricated group in most cycles. The contacts between threads were located at the coronal aspect of all observed screw mating threads.Conclusion: Data indicate that the lower coefficient of friction of a carbon lubricant can generate higher preload. The machining precision observed produced the adaptation and regular contact interfaces.
Keywords: implant; torque; preload.
Introduction
Screws or cements retain rehabilitations onto osseointegrated implants. Screws for abutments and prosthetic crowns are used to fasten these components to the implants, with the objectives of maintaining the stability and the integrity of both the implant and prosthesis, during insertions and removals for the period of prosthesis manufacture and throughout clinical life. The loosening of screws is considered one of the most common causes of failure for screw-retained prosthesis 2,7,11,12.
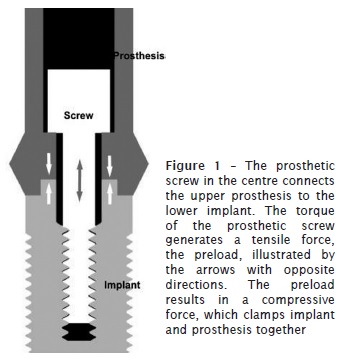
Torque movements of a screw during tightening, in order to clamp prosthesis onto an implant, subject the screw to fastener tension. This tensile elastic deformation of the screw, denominated preload, maintains the prosthesis and implant tightened clinically. The frictional force between the external threads of the screw and the internal threads of the implant stabilizes the connection, as illustrated in figure 1. The tightening of two parts by a screw can be denominated screw joint, and the clamping force, or preload, is the force that keeps them together 15. The parts may unfasten if the resultant of the forces trying to separate them overcomes the clamping force. Therefore, the separating forces do not have to be eliminated, but should be lower than the clamping forces, in order to have no interference 15. Consequently, there are two primary factors involved in the retention of prosthesis screwed over implants, an adequate torque for maximal preload and minimal separation force.
The intermediary and gold prosthetic screws, when subjected to masticatory forces, may loosen due to torque related reasons: inadequate torque, low preload development and operator inconsistencies, caused by repeated cycles, variations on the clinical torque and difficult access to the posterior mouth regions 10. Some authors regarded the loss of preload in prosthetic gold screws as a function of time as well 1,5.
Burguete et al. (1994) explain that the screw loosening process occurs initially when the external forces applied to the screw joint induce a negative effect, as a result of the compression of the preload, for example during mastication 3. In an analogy to a spring, the screw is stretched by torque in order to tighten the components and the friction on the threads keeps the tension. Any external force, axial or transversal, that produces a small slippage between the threads, disregarding its intensity, reduces part of the stretching and lowers the preload 8,15. Therefore, the higher the preload the higher will be the loosening resistance. However, in order to be effective, the preload must be lower than the elastic limit of the material, lower than the yield strength to avoid any damage, and higher than the loads applied during clinical function.
The success of a screw joint is related to the preservation of the preload, which depends on several properties of the material, such as: modulus of elasticity, composition, clamping of the parts, screw head design, strain, finishing of the interfaces, and presence of lubricant 15. Burguete et al. (1994) reported that the lubrication of the screws reduces the friction, resulting in higher preload for the same torque value compared with non-lubricated screws 3.
In view of the fact that an inadequate torque during tightening of the screw and loss of preload predispose to screw loosening, the purpose of the present study was to analyze the effect of a solid lubricant, a coating of vaporized carbon applied on titanium alloy prosthetic screws (Neotorque, Neodent, Brazil), on preload values.
Material and methods
Dental implants and prosthetic components (Neodent Implante Osseointegrável, Curitiba, PR, Brazil) were used in this in vitro study: 14 Titamax Ti Cortical implants (external hexagon 4.0, cpTi), 14 UCLAs (4.1 non-rotational, Ti6Al4V), 7 prosthetic screws Titânio (4.1, 4.3, Ti6Al4V), and 7 prosthetic screws Neotorque (4.1, 4.3, Ti6Al4V). Prosthetic screws of group 1, Neotorque, and group 2, Titânio,were identically machined, but the former received a 2 to 3 µm coating of vaporized carbon (manufacturer communication). Thus, the number of available screws determined the number of tests that could be performed.
The implants were mounted onto a perforated Teflon base, with a torque hand wrench (Neodent, Curitiba, PR, Brazil) with 80 N.cm torque, leaving five threads above the base. The UCLAs were secured onto the implants with the prosthetic screws from both groups, with 20 N.cm pretorque, using a hexagonal screwdriver fixed onto a prosthetic torque meter (Neodent, Curitiba, PR, Brazil). The same screwdriver was adapted onto a digital torque meter TQ-680 (Instrutherm, São Paulo, SP, Brazil) to tighten the screws to the manufacturer recommendation of 32 N.cm torque. The torque meter is calibrated every 12 months (K&L Laboratory of Metrology, São José dos Pinhais, Paraná, Brazil), accredited by the Brazilian Institute of Metrology (Inmetro).
The tests consisted of ten series of tightening and removal torques on coated and uncoated prosthetic screw groups. The tests were performed by the same operator, visually keeping the digital torque meter perpendicular to the base and without compressive force. The digital torque meter was used to ensure 32 N.cm torque for tightening and to verify the value of the removal torque necessary to loosen the screws, five minutes after their tightening.
The removal torque values from ten consecutives cycles were used to estimate the preload with equation 1 9,14.
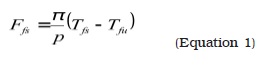
Where: Ffs = estimated preload, Tfs = applied torque, Tfu = removal torque and P = thread pitch.
The values of thread pitch (P = 0.4 mm) and applied torque (Tfs = 32 N.cm) were kept constant. The preload numerical values in the first cycle were decreased by 25% of their total, following 9 recommendation, in order to reduce the equation error in this cycle, which lies between -10 and -40%.
The values of preload were compared based on the specific characteristics of both screw groups. The results obtained were investigated using the Anderson-Darling normality test and Paired-differences analysis of the raw data (significance level 0.1).
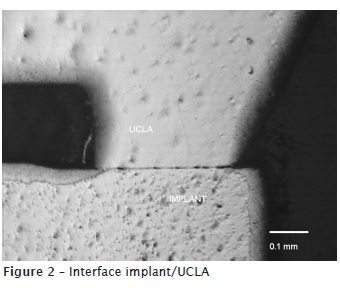
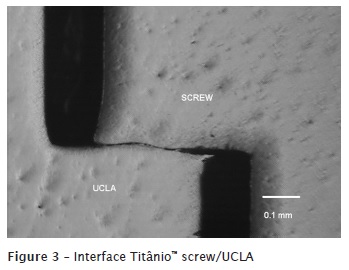
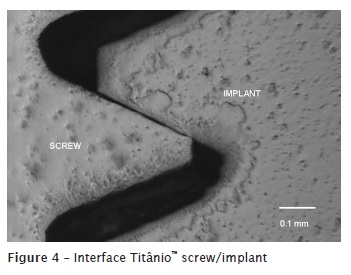
After numerical data collection, the Teflon base was sectioned and the segments with Neotorque screws and Titânio screws were embedded in polymethyl methacrylate (Clássico, São Paulo, SP, Brazil). The resulting blocks were abraded and polished with 120, 240, 320, 400, 600, 800, and 1200-grit silicon carbide paper (Politriz DP10, Panambra, São Paulo, SP, Brazil), in order to expose the screw joint connection longitudinally. The adaptation of three interfaces: implant/UCLA, screw/UCLA, and screw/implant was examined using light microscopy (100x magnification; LAMBDA 17-T, Atto Instruments, New Territories, Hong Kong, China).
Results
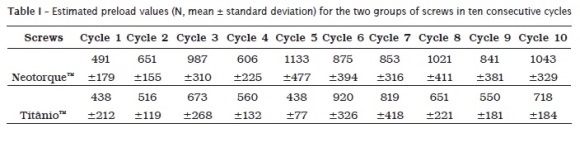
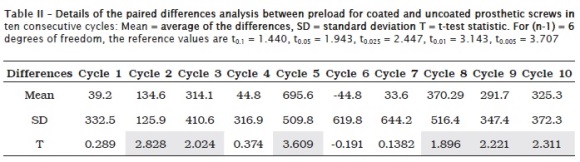
The values of removal torque for the fourteen prosthetic screws were always lower than the applied tightening torque, varying from 10 to 29 N.cm on the 10 tested cycles. The mean values of preload were calculated from the removal torque (table I), and the data was analysed statically (table II).
Between cycles 1 and 3, the mean preload values of both groups increased. Up to the fifth cycle the preload for coated screws was higher than that for uncoated ones. In cycles 6 and 7 both groups presented similar values. It can be observed in table I that after cycle 6 the variation of the mean preload values was not as pronounced as in the first five cycles, but the general tendency of higher mean preload values for coated prosthetic screws was maintained.
The Anderson-Darling normality test was used to determine whether the data follow a normal distribution. Visually, most plots show that the data lie close to a straight line, and a normal distribution could be assumed (data not shown).
Table II shows the preload differences between both screw groups. Gray cells indicate that for a 90% confidence level, cycles 2, 3, 5, 8, 9 and 10 show a significant difference between the groups of screws. For a 99.5% confidence level, no cycle shows a significant difference between groups.
Microscopic analyses of the samples demonstrated the adaptation between implant/UCLA (figure 2), screw/UCLA (figure 3), and screw/implant (figure 4), in both groups of screws, with the recommended tightening torque. The interface screw/implant for both groups was regular, with contact interfaces observed in the coronal side of all geared threads and symmetrical spaces on the opposite side. Quantitative analysis of the interfaces was not performed, since no visual difference was observed among the samples.
Discussion
The applied tightening torque with the digital torque meter on the prosthetic screws of both groups tested was always the torque recommended by themanufacturer: 32 N.cm. Even though the use of this type of digital torque meter has no clinical indication due to its size, when employed for in vitro tests it allows precision on all the cycles and acquisition of removal torque values 14.
All removal torque values in this study were lower than the tightening ones; corroborating the findings of authors who propose that the embedment, with gradual accommodation and adaptation between the contact interfaces, results in a reduction of the friction coefficient 6,9,14,18,19.
Pesun et al (2001) and Siamos et al. (2002) observed that tightening and removal may include compressive forces, decreasing the preload 17-18. Also according to these authors, the compressive force applied is higher in loosening than when tightening the connection. Therefore, any pressure exerted during removal could be responsible for lowering the preload. In the present study, this aspect was controlled during the tests, performed by one skilled operator, keeping the digital torque meter aligned with the connection without exerting any pressure, besides the actual weight of the measuring device.
The preload is of great importance to the stability of the screw connection and is used to describe the phenomena of screw loosening and subsequent implant malfunction. For that reason, if the preload decreases during clinical use of the prosthesis, the loosening of the screw reduces the connection stability, and may consequently lead to clinical failure. The present comparative study between two identical connections, differing only by application of a carbon lubricant, allowed the observation of higher preload on the latter. The results demonstrated that the lubricant used can be responsible for lowering torque removal and consequently increasing the preload. Further study with a larger number of samples could lead to statistically more significant results.
The application of the solid amorphous vaporized carbon lubricant was the aspect explored on the design of lower friction coefficient screw components used in the present study. In gold prosthetic screws higher preload due to decrease in friction was also observed, associated with lower removal torque and higher screw rotation angle 19. The application of a coating, in order to lubricate screws and increase the preload, has been well explored. Gold coated screws induced higher preloads for different insertion torques, when compared to titanium alloy and gold alloy 4. TiN coating of abutment screw can reduce the loss of preload with low coefficient of friction in order to maintain screw joint stability 13. Likewise, tungsten carbide carbon surface coated screws provided higher preload and were more effective in maintaining the preload, than uncoated titanium alloy screws 16.
The purpose to use standard metallic UCLAs was to achieve the connection of all parts machined from the same manufacturer, allowing the investigation to be focused on the surface finish of the threads. Similar to Martin et al. 14, who detected generalized contact between threads of the screw with the implant, the contact up to the last mating thread in the present study, results from their machining.
Martin et al. (2001) concluded that, as friction decreases the preload of the screw joint increases 14. Tzenakis et al. (2002) also tested the effect of repetitive cycles of insertion and removal of prosthetic screws on implants and concluded that it could be beneficial, with an increase of preload observed with additional cycles caused by the lowering of the friction coefficient between the mating threads 19. The present study validates these observations, where the same applied tightening torque generated a lower removal torque after consecutive cycles, and therefore higher preload. The increase of preload values may lower the risk of screw loosening and failure of the connected components, because it improves their clamping.
Conclusion
The carbon coating applied on the prosthetic screws reduced the friction coefficient between the mating threads and produced higher preload when compared with uncoated screws.
Acknowledgments
The authors thank Neodent (Curitiba, PR, Brazil) for the donation of dental implants and prosthetic components.
References
1. Al Jabbari YS, Fournelle R, Ziebert G, Toth J, Iacopino AM. Mechanical behavior and failure analysis of prosthetic retaining screws after long-term use in vivo. Part 1: Characterization of adhesive wear and structure of retaining screws. J Prosthodont. 2008 Apr;17(3):168-80. [ Links ]
2. Binon PP. The effect of implant/abutment hexagonal misfit on screw joint stability. Int J Prosthodont. 1996 Mar-Apr;9(2):149-60.
3. Burguete RL, Johns RB, King T, Patterson EA. Tightening characteristics for screwed joints in osseointegrated dental implants. J Prosthet Dent. 1994 Jun;71(6):592-9.
4. Byrne D, Jacobs S, O'Connell B, Houston F, Claffey N. Preloads generated with repeated tightening in three types of screws used in dental implant assemblies. J Prosthodont. 2006 May-Jun;15(3):164-71.
5. Cantwell A, Hobkirk JA. Preload loss in gold prosthesis-retaining screws as a function of time. Int J Oral Maxillofac Implants. 2004 Jan-Feb;19(1):124-32.
6. Cibirka RM, Nelson SK, Lang BR, Rueggeberg FA. Examination of the implant-abutment interface after fatigue testing. J Prosthet Dent. 2001 Mar;85(3):268-75.
7. Gratton DG, Aquilino SA, Stanford CM. Micromotion and dynamic fatigue properties of the dental implant-abutment interface. J Prosthet Dent. 2001 Jan;85(1):47-52.
8. Haack JE, Sakaguchi RL, Sun T, Coffey JP. Elongation and preload stress in dental implant abutment screws. Int J Oral Maxillofac Implants. 1995 Sep-Oct;10(5):529-36.
9. Hagiwara M, Ohashi N. A new tightening technique for threaded fasteners. Journal of Offshore Mechanics and Arctic Engineering. 1994;116:64-9.
10. Hill EE, Phillips SM, Breeding LC. Implant abutment screw torque generated by general dentists using a hand driver in a limited access space simulating the mouth. J Oral Implantol. 2007;33(5):277-9.
11. Jemt T, Lekholm U. Measurements of bone and frame-work deformations induced by misfit of implant superstructures. A pilot study in rabbits. Clin Oral Implants Res. 1998 Aug;9(4):272-80.
12. Jemt T, Lekholm U, Johansson CB. Bone response to implant-supported frameworks with differing degrees of misfit preload: in vivo study in rabbits. Clin Implant Dent Relat Res. 2000;2(3):129-37.
13. Jung SW, Son MK, Chung CH, Kim HJ. Abrasion of abutment screw coated with TiN. J Adv Prosthodont. 2009 Jul;1(2):102-6.
14. Martin WC, Woody RD, Miller BH, Miller AW. Implant abutment screw rotations and preloads for four different screw materials and surfaces. J Prosthet Dent. 2001 Jul;86(1):24-32.
15. McGlumphy EA. Keeping implant screws tight: the solution. J Dent Symp. 1993 Aug;1:20-3.
16. Park JK, Choi JU, Jeon YC, Choi KS, Jeong CM. Effects of abutment screw coating on implant preload. J Prosthodont. 2010 Aug;19(6):458-64.
17. Pesun IJ, Brosky ME, Korioth TW, Hodges J, Devoe BJ. Operator-induced compressive axial forces during implant gold screw fastening. J Prosthet Dent. 2001 Jul;86(1):15-9.
18. Siamos G, Winkler S, Boberick KG. Relationship between implant preload and screw loosening on implant-supported prostheses. J Oral Implantol. 2002;28(2):67-73.
19. Tzenakis GK, Nagy WW, Fournelle RA, Dhuru VB. The effect of repeated torque and salivary contamination on the preload of slotted gold implant prosthetic screws. J Prosthet Dent. 2002 Aug;88(2):183-91.
 Correspondence:
Correspondence:
Milton Carlos Kuga
Av. Saul Silveira, 5-01
CEP 17.018-260 – Bauru – SP – Brasil
E-mail:kuga@foar.unesp.br
Received for publication: October 27, 2011.
Accepted for publication: December 14 2011.













