Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.9 no.2 Joinville Abr./Jun. 2012
Original Research Article
Nursing habits in cleft lip and palate children
Cintia Magali da Silva I; Beatriz Costa II; Lucimara Teixeira das NevesII
I Carianos Health Center – SMS – Florianópolis – SC – Brazil.
II Pediatric Dentistry Department – HRAC – USP – Bauru – SP – Brazil.
ABSTRACT
Introduction: Cleft lip and palate anomalies are malformations that affect patients causing some alterations. These alterations can compromise maternal nursing and lead to early introduction of bottle feeding and sugar in the diet of cleft lip and palate infants, compromising their oral health and the surgical/rehabilitation process. Objective: The purpose of this study was to evaluate the nursing habits and the use of baby bottles in a group of cleft lip and palate infants. Material and methods: Two hundred and twenty nine mothers of cleft lip and palate infants in the age range from 6 to 36 months enrolled in the Hospital for Rehabilitation of Craniofacial Anomalies – USP/Bauru were interviewed. It was obtained data on family socioeconomic characteristics as well as mother educational level using the patients file. Using a pre-structured questionnaire accomplished always by the same interviewer, information on natural and artificial nursing pattern was obtained.Results: Only 21.4% of the mothers accomplished breastfed their babies. 98.25% of mothers used bottle feeding with milk and other sucrose liquids at one to ten times frequency. Nocturnal nursing habit was verified in 59.38% of total sample.Conclusion: Cleft lip and palate infants presented inadequate nursing habits in relation to both the content and the frequency ingestion, suggesting the need of a multidisciplinary guidance and following-up of infants during this age range.
Keywords: infant; cleft lip; cleft palate.
Introduction
Cleft lip and palate is a congenital malformation occurring between the fourth and twelfth week of intra-uterine live, period corresponding to the face development. Because of the lack of development of nasal and maxillary process, an interruption in upper lip formation occurs and causes the cleft lip which can be classified into either unilateral or bilateral. On the other hand, the lack of fusion of the median nasal and maxillary process causes the cleft palate. This is the most frequent anomaly occurring in the human face 17, where the interference of genetic and environmental factors may act either single or in association 12. By evaluating the incidence of cleft lip and palate in children, França and Locks in 2003 9, found a relation of 1.24 per each 1,000 born alive. The cleft lip and palate is the most common type compared to cleft palate or cleft lip only 2. Coutinho et al. 5 also observed in a study conducted in the northeast of Brazil a greater prevalence of cleft lip and palate occurring most in male patients.
The presence of malformation results in several functional, aesthetic, and psychosocial alterations 14,15, with a complex extensive rehabilitation process based on a multidisciplinary team. Accordingly, this subjects rehabilitation comprises a set of attention to health actions where the role of doctors, nurses, dentists, nutritionists, speech and language therapists, psychologists, physiotherapists and social workers is necessary; they should work in an integrated manner, offering the best treatment. For parents, the birth of a cleft lip and palate child causes a greater impact. Depending on the lesion severity, the rehabilitative process reach the adult age; therefore, the patients should receive support during all the rehabilitation process, aiming to their integration to the social and familiar environment 2. The family should be welcomed and supported by all the health team, receiving all the necessary support.
At the cleft lip and palate birth, one of the first difficulties found by the parents is nursing. Many times, to feed a child is difficult, mainly when the family did not receive any guidance. Because of the altered anatomy, the baby tends to present suction difficulties due to lack of negative intraoral pressure. The nursing time is longer; also it is common the occurrence of choking and regurgitations. This can lead to anxiety and concern of parents and/or caregivers 7.
Also, it is important to emphasize that the surgical treatment onset initiates at an early stage of the child life 6. Lip reconstructive surgery, so-called cheiloplasty, is indicated at the third month of life once the baby is healthy and weighing at least 5 kg. At one year of age, palatoplasty (palate reconstructive surgery) can be performed if the baby is healthy and weighing at least 9 kg.
The suction difficulty and the anxiety because of the surgery may lead the parents to opt by the use of bottles early, and consequently, to sucrose introduction 6. On the other hand, it is known that sucrose consumption at an early age enables the creation of cariogenic food habits 19. According to dental literature, these dietary habits has direct influence in the oral health condition of the subject at infancy age 19, by the development of caries, which in this patient group may compromise the success of the rehabilitative process because of the presence of infectious focus. Pain symptomatology caused by caries, especially in its acute phase, results in discomfort acting negatively in the persons health and well-being.
The aim of this study is to know the nursing habits and the use of bottles by cleft lip and palate infants, as well as to alert both health professionals and parents about the habits that may represent risk to good oral health condition. Therefore, it is aimed to contribute to the organization of actions prioritizing health promotion of cleft lip and palate children.
Material and methods
This study is a descriptive quantitative research. Prior to the research onset, an analysis to determine the sample size was performed which found that a sample of 200 children was needed to detect significant results. Therefore, 229 mothers of cleft lip and palate infants regularly enrolled in the Hospital for the Rehabilitation of the Craniofacial Anomalies – University of São Paulo (HRAC – USP ) participated in the study. The childrens age ranged from 6 to 36 months, without race and socioeconomic classification distinction. The participants were randomly selected, according to the treatment performed at the Baby Clinics of the Pediatric Dentistry Department during a period of three months. It is worth noting that the dental appointment is a routine procedure when the child visits the hospital because the adequate oral health condition is fundamental for the rehabilitative process. The mothers of the children with either suspicion or diagnosis of syndromes were excluded from the research to avoid the influence of other factors in the nursing pattern. This information was based on the clinical observation and anamnesis and it was always confirmed by consulting the patients file aiming to the correct diagnosis of the anomaly presented by the baby.
This study was approved by the Ethical Committee in Research of HRAC-USP (Protocol #3232) and was in agreement with the guidelines of the Brazilian Ethical Committee in Research. All participants read and signed a Free and Clarified Consent form prior to the beginning of the study Data regarding to patients (identification, age range, cleft type) and mothers profile (scholarity degree and socioeconomic classification) were obtained through patients file. The socioeconomic classification is executed by a social worker from the Social Service Department of HRAC-USP, who observes the familys profile data such as family income, parents degree of instruction, house conditions, among others.
Next, an interview was carried out at the Baby Clinics of HRAC-USP, always by the same examiner (a dentist enrolled in the Course of Specialization in Pediatric Dentistry of HRAC-USP). Observation bias was avoided by conducting a pre-test of the questionnaire through a pilot study with 25 participants always by the same examiner aiming also the examiners training. The participants of the pilot study did not enroll in the study. A structure questionnaire was used in the interview, comprising questions on the childs nursing habits. In the interview, the mother was questioned concerning to the use of breast or bottle feeding, its content and the frequency of the l nursing even if during the childs sleep.
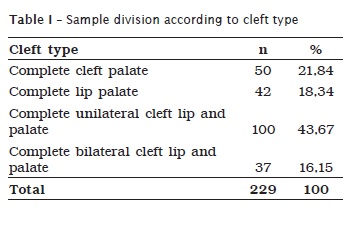
A total of 229 patients, 139 male (n=60.69%) and 90 female (n=39.31%) whose mean age was 20.94 months (standard deviation = 7.35), was divided into 4 groups according to the cleft type classification of Spina et al. 20, adopted by HRAC-USP. This cleft lip and palate classification, very used in Brazil, takes into consideration the location of the anomaly in relation to the incisor foramen. Therefore, the studys participants were 50 mothers of complete cleft palate, 42 mothers of complete cleft lip, 100 mothers of complete unilateral cleft lip and palate and 37 mothers of complete bilateral cleft lip and palate, as seen in table I.
Results
According to the analysis of the patients file, it was observed that 88.63% of the families (n=203) were socioeconomically classified as low and 11.37% (n=26) as medium, according to data displayed in table II .
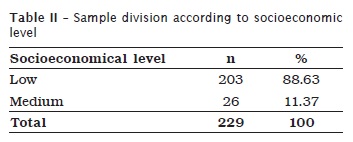
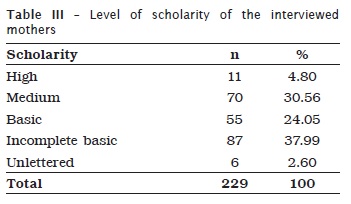
Table III show the level of scholarity of the interviewed mothers. It is woeth noting the small number of participant mothers with high scholarity level (n=11). Additionally, most mothers showed a low scholarity level with only the basic school. It is also highlighted the presence of unlettered participants (n=6).
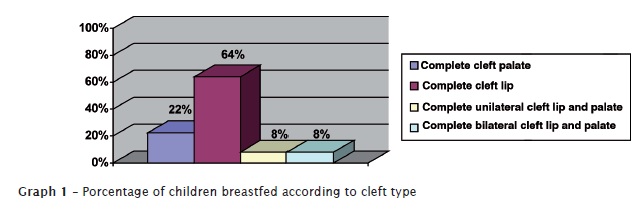
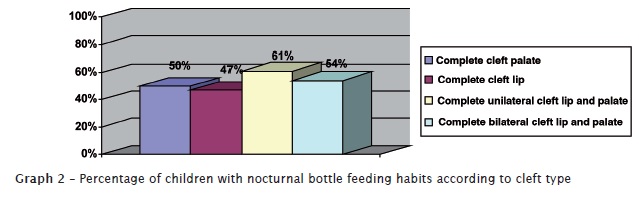
The nursing pattern features will be displayed according to the different cleft type groups. In complete cleft palate group, only 22% of the mothers breastfed their babies (n=11). Additionally, at the moment of the interview, all babies were using bottles (n=50), at frequency ranging from 1 to 7 times/day. They consumed milk containing any form of sucrose, such as chocolate powder, lacteal flours, or only sugar. The aggravating factor was that 76% (n=38) had nocturnal bottle or breast feeding habit.
By analyzing the complete cleft lip group, we observed that 64.28% (n=27) of the babies had been breastfed. Concerning to the use of bottles, 92.85% of the mothers reported that they were offered at 2 to 8 times per day. Of these patients, 85.7% used bottles containing milk with sugar, associated or not with chocolate powder or lacteal flour. On the other hand, nocturnal bottle or breast feeding were reported by 47.61% of the mothers (n=20).
In complete unilateral cleft lip and palate group, only 8% (n=8) of the mothers reported to breastfeed. We observed that, at the moment of the interviews, 99% (n=99) of the children were using bottles. In this group, 92% used bottles at a frequency of up to 10 times per day for milk consumption with any type of sugar complement. Of these children, 61% (n=61) presented nocturnal bottle feeding.
Concerning to breastfeeding, only 3 mothers in the complete bilateral cleft lip and palate group reported to perform it. In this group, 100%, at the study moment, used bottle with milk and sugar at a frequency of up 7 times per day. Regarding to nocturnal breast or bottle feeding, 54.05% of the babies presented such habit.
By analyzing the total number of participants, it could be noted that 78.6% affirmed that they had not breastfed (n=180). Breastfeeding in the different types of cleft is seen in graph 1.
According to this study, 98.25% of the total number of participants reported to use bottle feeding at a frequency of 1 to 10 times per day for nursing their children (n=225), of which 93.88% added any sucrose form in its content. Still analyzing the total number of participants, 59.38% (n=136) affirmed that their children had nocturnal bottle feeding habit. Graph 2 demonstrated the percentages of children with nocturnal bottle feeding habit according to cleft types. Another aspect observed in the total sample was that 27% and 7.7% consumed respectively juices and teas with either sugar or honey and 7.6% consumed soft drinks.
Discussion
It can be observed that most of the participants were mothers of complete unilateral cleft lip and palate children (n=100), which is in agreement with the findings of Brazilian researchers 9 who reported this cleft type as the most prevalent.
The importance of the knowledge of feeding habits of cleft lip and palate babies is the fact that such habits directly influence in oral health maintenance 3. This, on the other hand, is mandatory during all the rehabilitative process of cleft lip and palate patient. The presence of infectious foci as caries contraindicate the execution of the surgical procedures because of both the contamination and the possibility of pain of odontogenic origin at the post-surgical recovery period.
Many times, the deleterious habits may be influenced by the cultural and socioeconomic level of population. Therefore, we investigated the mothers degree of instruction because they have been the person responsible for infants care. We found a low scholarity level in total sample, including also the presence of unlettered mothers. These data are in agreement with those of another Brazilian study on cleft lip and palate patients 4.
It is worth noting the fact that most of the families presented a low socioeconomic level, few families were at a medium level and none at a high level. Such finding corroborates those of Durning et al. (2007) 8, because these authors correlated the higher prevalence of clefts to material privation. This large number of cleft lip and palate patients at a low socioeconomic level may demonstrate a higher predisposition to clefts because these have been related to not only genetic but also environmental factors. In many situations, pregnant women may be more prone to infections and nutritional deficiencies which will fatally lead to malformation in the baby 10.
With the malformation presence, it is necessary that a multidisciplinary team act integrally, aiming to the comprehensive patients treatment. The cleft generally results in psychological, aesthetical and functional problems for patients 14 occurring in a significant number of Brazilian subjects 16. The attention to patient requires not only the execution of surgical procedures, but also demands a continuous following-up of the patient and family 15. Accordingly, it is mandatory that the health professionals be well prepared to diagnose and treat clefts 5.
Therefore, a very important aspect in the approach of cleft lip and palate children is nursing habits. Children born with cleft lip and palate underwent an interference of their natural capacity to be fed properly, presenting negative aspects in their normal evolution 1. Early guidance on the best feeding techniques should be performed. Children of well oriented families grow more, have an easier feeding and their parents presenting less anxiety. The establishment of breastfeeding should be attempted and stimulated, observing the physiological, psychological and social limits involving the child and family. Breastfeeding is beneficial because of the nutritive value and antibacterial quality, helping to prevent infections 1,6. In addition, the suction movement promotes the development of the orofacial muscles 18, acting as a physiotherapy effect for surgical recovery.
Despite all stimulus for breastfeeding through campaigns and knowledge about its benefits for the baby (nutritional value, muscle development, mother contact with the baby), the mothers of cleft lip and palate babies face, at birth, doubts and difficulties inherent to the malformation presence. Such fact may lead to the early use of bottles because of the concern with nutrition, growth and development of the baby 22.
Mothers of cleft lip and palate children show great expectancy regarding to the execution of the plastic surgical procedures for defect correction because this procedure demands that the children present an adequate body weight. Consequently, weight gain is a concern for many parents 7. Because sugar is one of the cheapest caloric sources, this could be the reason that leads these mothers to used bottle with sugar. On the other hand, early sucrose consumption lead to the establishment of inappropriate food habits which become difficult to be modified 19.
This studys results reaffirm these difficulties since only 21.4% of the babies from the total sample had been breastfed. Most of these babies (graph 1) presented a complete cleft lip (64%). This cleft type may only compromise the breast apprehension, which can be solved by adapting the baby position. These data are in agreement with those of Dalben et al. (2003) 7 in a study conducted at HRAC-USP.
However, it is known that complete cleft palate babies show a suction impairment due to difficulty in developing negative pressure required for suction and expressing the milk. Despite these difficulties, breastfeeding must always be stimulated since the child can be capable of adapting and establishing this negative intraoral pressure to suction 6. Therefore, it is recommended to breastfeed the newborn for five minutes per breast aiming to the milk suction and also to reinforce the contact between mother and baby. After this period, expressed milk can be offered in a bottle 1.
It is important to guide the parents during breast or bottle feeding that the baby must be at semi-sitting position to avoid reflux, aspiration and choking. Additionally this position also prevents milk accumulation within the hearing cavity and consequently otitis episodes. It is worth highlighting the necessity of pauses during breastfeeding to enable regurgitation. Also, the cleft area should be stimulated through the contact between either the mothers or the bottles nipple aiming to exercise the affected muscles. Concerning to the bottles nipples, they should be of orthodontic type because they are shorter and more anatomic. The nipple should be placed at a 90° angle in relation to the face with its orifice upwards. The gravity together with the childs (semi-sitting) and the bottle nipples (90º) position impedes that the content be directed to the nasal cavity. Also, the parents should be guided to perform oral hygiene with cotton swabs and/or wet gauzes before and after feeding to avoid the permanence of residues and milk within the cleft area 1.
A deleterious habit that put the child at risk for caries is the use of bottle feeding at high frequency and during sleep. This was reported by 59.38% of the total sample. This situation of caries disease risk is aggravated because the babies show reduced saliva action by flow velocity decrease, reduced facial muscle movements, and inefficient self-cleaning action of the tongue compared to adults, enabling a faster development of caries 19.
It is also observed that many mothers (28.3%) reported to offer citric juices with sugar or honey. This guidance is provided to treat the physiologic anemia commonly found in cleft lip and palate infants, which could impede the execution of the surgical procedure. The acid components of citric juices collaborate to the biofilms pH decrease and consequently to the onset and evolution of the process of tooth structure demineralization which makes the oral environment suitable for caries disease development 7. Some mothers also reported to offer soft drinks and teas with honey. Several times, parents and even pediatric doctors use or recommend honey because they do not know about its cariogenic features. Accordingly, it is important that both health professionals and parents be guided regarding the caries risk of soft drinks and honey consumption.
This study showed that the nursing habits of cleft lip and palate children are inappropriate, representing an additional health risk according to literature 11,13. Therefore, it is obvious that this population needs special attention from dental professionals through constant follow-up of and programs of mother-and-child care where breastfeeding and diet guidance should be emphasized and reinforced to provide and maintain an adequate health condition aiming the rehabilitation success, patient/family satisfaction and life quality.
Conclusion
Based on this studys interviews, it can be concluded that the studied population present inappropriate nursing habits concerning to both sucrose consumption, ingestion frequencies and periods. It is mandatory that these patientd be followed-up by a multidisciplinary team where the dentist plays an important role
References
1. Araruna RC, Vendrúsculo DMS. Alimentação da criança com fissura de lábio e/ou palato – um estudo bibliográfico. Rev Latinoam Enferm. 2000 Apr;8(2):99-105. [ Links ]
2. Augusto HS, Bordon AKCD, Duarte DA. Estudo da fissura labiopalatal. Aspectos clínicos desta malformação e suas repercussões. Considerações relativas à terapêutica. JBP, J Bras Odontopediatr Odontol Bebê. 2002 Sep-Oct;5(27):432-6.
3. Bian Z, Holt R, Du M, Jin H, Bedi R, Fan M. Caries experience and oral health behavior in Chinese children with cleft lip and/or palate. Pediatr Dent. 2001 May;23(5):431-4.
4. Castilho ARF, Neves LT, Carrara CFC. Evaluation of oral health knowledge and oral health status in mothers and their children with cleft lip and palate. Cleft Palate Craniofac J. 2006 Apr;43(4):726-30.
5. Coutinho ALF, Lima MC, Kitamura MAP, Pereira RM, Ferreira Neto J. Perfil epidemiológico de portadores de fissuras orofaciais atendidos em um centro de referência no nordeste do Brasil. Rev Bras Saúde Mater Infant. 2009 Apr-Jun;9(2):149-56.
6. Dalben GS, Costa B, Gomide MR, Neves LT. Amamentação em bebês portadores de fissuras labiopalatais. JBP, J Bras Odontopediatr Odontol Bebê. 2001 Jul-Aug;4(20):317-20.
7. Dalben GS, Costa B, Gomide MR, Neves LT. Breast-feeding and sugar intake in babies with cleft lip and palate. Cleft Palate Craniofac J. 2003 Jan;40(1):84-7.
8. Durning P, Chestnutt IG, Morgan MZ, Lester NJ. The relationship between orofacial clefts and material deprivation in Wales. Cleft Palate Craniofac J. 2007 Mar;44(2):203-7.
9. França CMC, Locks A. Incidência das fissuras lábio-palatinas de crianças nascidas na cidade de Joinville (SC) no período de 1994 a 2000. J Bras Ortodon Ortop Facial. 2003 Nov-Dec;8(4):429-36.
10. Freitas JAS, Dalben GS, Santamaria JR M, Freitas PZ. Current data on the characterization of oral clefts in Brazil. Braz Oral Res. 2004 Apr-Jun;18(2):128-32.
11. Hewson AR, McNamara CM, Foley TF, Sandy JR. Dental experience of cleft affected children in the west of Ireland. Int Dent J. 2001 Apr;51(2):73-6.
12. Leite ICG, Paumgartten FJR, Koifmann S. Fendas orofaciais no recém-nascido e o uso de medicamentos e condições de saúde materna: um estudo de caso-controle na cidade do Rio de Janeiro. Rev Bras Saúde Matern Infant. 2005 Jan-Mar;5(1):35-43.
13. Lucas VS, Gupta R, Ololade O, Gelbier M, Roberts GJ. Dental health indices and caries associated microflora in children with unilateral cleft lip and palate. Cleft Palate Craniofac J. 2000 Sep;37(5):447-52.
14. Miguel LCM, Locks A, Prado ML. O relato das mães quando do início escolar de seus filhos portadores de má-formação labiopalatal. RSBO. 2009 Jun;6(2):155-61.
15. Monlléo IL, Lopes VLGS. Anomalias craniofaciais: descrição e avaliação das características gerais da atenção no Sistema Único de Saúde. Cad Saúde Pública. 2006 May;22(5):913-22.
16. Nunes LMN, Pereira AC, Queluz DP. Fissuras orais e sua notificação no sistema de informação: análise da Declaração de Nascidos Vivos (DNV) em Campos dos Goytacazes, Rio de Janeiro, 1999-2004. Ciênc Saúde Coletiva. 2010 Mar;15(2):345-52.
17. Rezende KMPC, Zöllner MSAC. Ocorrência das fissuras labiopalatais no município de Taubaté nos anos de 2002 e 2006. Pediatr Mod. 2008 Nov-Dec;30(4):203-7.
18. Ribeiro EM, Moreira ASCG. Atualização sobre o tratamento multidisciplinar das fissuras labiais e palatais. RBPS. 2005 Jan-Mar;18(1):31-41.
19. Silva CM, Basso DF, Locks A. Alimentação na primeira infância: abordagem para a promoção da saúde bucal. RSBO. 2010 Oct-Dec;7(4):458-65.
20. Spina V, Psillakis JM, Lapa FS, Ferreira MC. Classificação das fissuras lábio-palatinas: sugestão de modificação. Rev Hosp Clín Fac Med. 1972 Jan;27(1):5-6.
21. Steffens H, Brandão AA, Guariza Filho O, Grégio AMT, Steffens JP. Avaliação do potencial do cloranfenicol para induzir teratogenicamente o aparecimento de fissura palatina em ratos Wistar. RSBO. 2010 Jun;7(2):154-8.
22. Yong JL, Oriordan M, Goldstein JA, Robin NH. What information do parents of newborns with cleft lip, palate or both want know? Cleft Palate Craniofac J. 2001 Jan;38(1):55-8.
 Correspondence:
Correspondence:
Cintia Magali da Silva
Rua José Joaquim dos Santos, n.º 49 – Centro
CEP 88302-030 – Itajaí – SC – Brasil – RJ – Brasil
E-mail:cintiaodonto@yahoo.com.br
Received for publication: March 21, 2011.
Accepted for publication: November 23, 2011.













