Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.9 no.2 Joinville Abr./Jun. 2012
Original Research Article
Evaluation of shear bond strength of orthodontic resin and resin modified glass ionomer cement on bonding of metal and ceramic brackets
Rosana Costa Casanovas de Carvalho I; Natália Maria Porto de Carvalho I; Synara Santos Herênio I ; José Roberto de Oliveira Bauer I Antonio Ernandes Macedo Paiva II; José Ferreira Costa I; Elizabeth Lima Costa I
I Federal University of Maranhão – São Luís
II Department of Mechanics and Materials of the Federal Technological Institute of Maranhão – São Luís – MA – Brazill.
ABSTRACT
Objective:The aim of this study was to evaluate the shear bond strength of orthodontic resin and resin-modified glass ionomer cement on bonding of metal and ceramic brackets. Material and methods: Forty bovine teeth were sectioned and embedded into PVC with chemically-cured acrylic resin. The labial surfaces were flattened and received prophylaxis with pumice and water. Then they were divided into four groups, according to the bonding material and the type of bracket. Group 1: metallic bracket + Transbond XT; Group 2: metallic bracket + Vitremer; Group 3: ceramic bracket + Transbond XT; Group 4: ceramic bracket + Vitremer. The bonding was performed according to the manufacturers’ recommendations. The shear bond strength test was conducted in a universal testing machine (TIRAtest 2420) at a crosshead speed of 0.5 mm/min. Then, the fractured surfaces were evaluated using a stereomicroscope (x15 magnification) to check the adhesive remnant index. Data was subjected to two-way ANOVA and Tukey’s test for pairwise comparisons (a = 0.05).Results: The results suggested a non-significant effect of the interaction (p > 0.97), and only main factors were significant (p = 0.0001). The bond strength of Transbond XT was statistically higher than Vitremer. Ceramic brackets obtained the highest values of resistance when compared with metal brackets. Conclusion: The ceramic brackets bonded with Transbond XT orthodontic resin have excellent bond strength results.
Keywords: shear bond strength; dental bonding; orthodontic brackets.
Introduction
The dental advanced has stimulated numerous researches aiming to analyze different adhesive materials which could be used in orthodontic brackets bonding to tooth enamel. Additionally, it is of fundamental importance that the material present an effective bonding to tooth surface, resisting to masticatory and orthodontic forces constantly applied. However, it is necessary that the material also enable an easy removal without damaging the enamel 5,7,10,13,18,21.
The first reports on direct bonding of brackets to enamel surface, according to literature, was conducted by Sadler in 1958, and initially the bracket bonding was performed through orthodontic bands on all teeth. In 1977, Zachrisson 27 described numerous disadvantages of this procedure: difficulty of performing oral hygiene, larger chairtime, and poor aesthetics. Therefore, direct bonding technique of orthodontic brackets was an indispensable advancement for treatment developing and simplification. However, this technique was only possible because of the etching of tooth enamel, described by Buonocore in 1955 4, resulting in a routine treatment in daily practice. Attempting to facilitate the procedures during orthodontic bonding, the manufacturers have developed materials promising efficacy and aiming to decrease the number of clinical steps and to meet the demand on aesthetics and comfort 5,6,9,18. The association of the etching of enamel surface with Bis-GMA-based composite resins has been, since the 80s, the bonding method of choice and the scope of several studies because this association presents clinically satisfactory bond strength and dimensional stability 10,15,16,19.
Glass ionomer cement and compomer materials have been evaluated and available on dental market for performing the bonding of orthodontic brackets because they show the single feature of fluoride releasing; this is capable of preventing caries lesions around orthodontic brackets and bands after the treatment ending as well as of enabling the chemical adhesion to tooth structure, not necessitating previous enamel etching 5,13,17,21,26.
Orthodontic brackets may be composed of several materials, such as stainless steel, polymers, porcelain, titanium or their combination. Ceramic brackets have been available for clinical use since 1987. They were designed to combine its excellent aesthetics with the well-known reliability of stainless steel brackets. However, a greater risk of enamel fracture during bracket debonding has limited its use 1,2,7,25.
The current need of testing the numerous materials used to bond orthodontic brackets justifies this present study, whose aim was to analyze and compare in vitro the shear bond strength of two different materials (Transbond XT resin cement and Vitremer resin-modified glass ionomer cement) for the bonding of metallic and ceramic orthodontic brackets as well as to evaluate the enamel conditions after the debonding, through adhesive remnant index (ARI).
Material and methods
Forty sound mandibular incisor teeth were selected. The teeth were cleaned and stored in a plastic recipient with distilled water under refrigeration, at 6°C until their use 22.
The study was based on the methodology established by the International Organization for Standardization (ISO), specification TR11405 for mechanical bond strength tests 11.
The root portion was sectioned with aid of carborundum discs, mounted in straight handpiece (Dabi Atlante, Ribeirão Preto, São Paulo, Brazil), at low speed, under refrigeration, at 1 cm shorter of the incisal edge. Tooth blocks were embedded in chemically–cured resin (Clássico Artigos Odontológicos, São Paulo, Brazil) within PVC tubes.
With the aid of a horizontal polishing machine (Aropol 2V, Arotec, Cotia, São Paulo, Brazil) and sandpapers in descending order #120, #220, #400 and #600 (3M, Sumaré, São Paulo, Brazil), the enamel surface was flattened under refrigeration.
Prior to bonding, tooth surfaces underwent dental prophylaxis with Robinson brush (Microdont, São Paulo, Brazil) mounted in contra-angle handpiece (Dabi Atlante, Ribeirão Preto, São Paulo, Brazil), at low speed, and superfine pumice (SS White, Rio de Janeiro, Brazil) and water for 10 seconds. Following the surfaces were washed by water/air spray for 10 seconds and dried by air jet.
At this stage of the study, the samples were randomly divided into four groups (n = 10), according to the bonding material and the bracket type. The brackets used were Roth type for maxillary right central incisor, with bracket base design of 12.03 mm2.
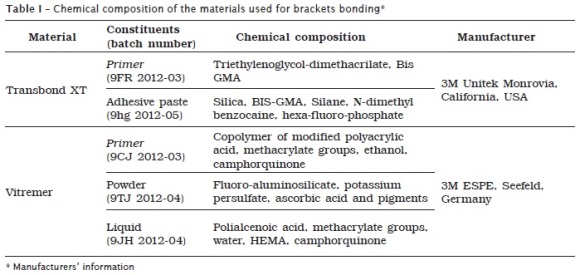
Group 1 was composed by metallic brackets (3M Unitek, Monrovia, California, USA) + Transbond XT; group 2 was composed by metallic bracket + Vitremer resin-modified glass ionomer cement; group 3 was composed by ceramic brackets (3M Unitek, Monrovia, California, USA) + Transbond XT; and group 4 was composed by ceramic brackets + Vitremer resin-modified glass ionomer cement (table I). The sequence used for bonding technique is described below:
Groups 1 and 3: enamel etching with 37% phosphoric acid for 15 seconds, washing and drying for the same time, application of XT primer, brackets bonding with Transbond XT resin, removal of the excesses through dental probe, light-curing for 40 seconds: 10 seconds at each tooth surface (mesial, distal, incisal and gingival) at a distance of 1 mm from the bracket;
Groups 2 and 4: application of Vitremer primer for 30 seconds on tooth surface, drying of the primer with air jet for 15 seconds, light-curing for 20 seconds, mixing of the powder and liquid for until 45 seconds, brackets bonding with the cement, removal of the excesses with dental probe, light-curing for 40 seconds: 10 seconds (mesial, distal, incisal and gingival) at a distance of 1 mm from the bracket.
Light-curing was accomplished by using Ultralux (Dabi Atlante, Ribeirão Preto, São Paulo, Brazil), a device composed of halogen light of mean intensity of 400 mW/cm2.
After bonding, the samples were kept into distilled water at 37±2°C for 24 hours. Next, to perform the test, the bonded bracket was involved by a hook made of metallic orthodontic wire (Morelli Ortodontia, Sorocaba, São Paulo, Brazil) with 0.6 mm thickness 7,23, through load cell of 500 N in a universal testing machine (TIRAtest 2420, TIRA Maschinenbau Gmbh, Schalkau, Germany), at crosshead speed of 0.5 mm/min.
Shear bond strength values were obtained in Newtons (N), which were next calculated in MegaPascals (MPa). The shear bond stress was calculated by using the load applied through the formula S = F/A, in which S = shear bond strength, F = load (N) required for the disruption of the bracket/tooth union and A = area of bracket base (mm2).
Bond strength data were submitted to two-way ANOVA (bond material X bracket type ) and Tukey test for means contrast at a = 0.05.
After the trial, each fractured surface of the samples was evaluated by using stereomicroscope (Quimis Q7355–TZ, Diadema, São Paulo, Brazil), at x15 magnification, to quantify the adhesive remnant index (ARI).
Results
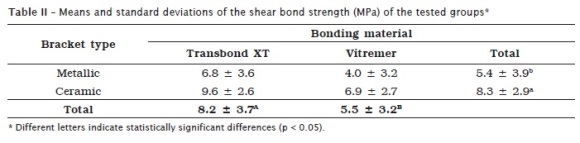
Shear bond strength values of the tested groups are seen in table II. The analysis of variance showed that the interaction of the factors was not significant (p > 0.97), only the main factors were statistically significant (p = 0.0001).
Transbond XT (8.2 ± 3.7 MPa) showed the highest shear bond values when compared to Vitremer (5.5 ± 3.2 MPa). The ceramic bracket (8.3 ± 2.9 MPa) obtained shear bond strength values higher than metallic brackets (5.4 ± 3.9 MPa).
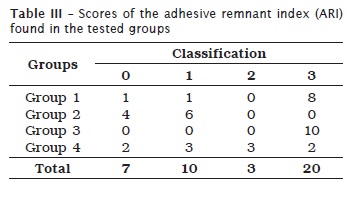
The assessment of ARI scores met the criteria idealized by Årtun and Bergland in 1984 3: 0 – none amount of composite adhered to the enamel; 1 – less than half of the composite adhered to the enamel; 2 – more than half of the composite adhered to enamel; and 3 – all composite adhered to enamel, including impression of the bracket net.
At this stage, we did not apply any statistical test; only the frequency of each index in each group was evaluated. In the assessment of ARI, the scores were observed within each group (table III).
Discussion
Bracket bonding to enamel has been a critical issue in Orthodontics since the direct bonding introduction, where is extremely important the biomechanical stability of the bracket/adhesive interface which transfers the force generated by the archwires activation to the tooth 10. The occurrence of accidental debonding of brackets is a frustrating aspect inherent to orthodontic practice, resulting in treatment time increase. A good orthodontic treatment path is mandatory for malocclusion correction, and therefore, the use of safer and more reliable materials is always desirable 7.
Bracket bonding has been the scope of several studies evaluating its bond strength aiming to improve the adhesive systems for orthodontic purposes 8,10,13.
The bonding of materials to enamel has been studied by several researchers, indicating that this type of substrate for shear bond strength testing 6,7,8,12,15,17,18,19,20. The use of bovine teeth by this study was motivated by the studies of Nakamichi et al. 14, who in 1983 studied the possibility of substituting human teeth in adhesion tests.
Because bovine tooth surfaces are very irregular, making difficulty the bonding of metallic brackets to the straight base of the metallic brackets, we opted by the flattening of the bovine tooth enamel to standardize the surface to be bonded; this allowed that at the moment of brackets bonding, the cement agents show a thickness as equal as possible 7,8,12,14,19.
Although dental market displays different types of brackets made of different materials, we chose stainless steel because they are the most used brackets in clinical practice 15,16,17,19,20, and ceramic brackets because of the increasing aesthetic demand of orthodontic patients 1,2,7,25.
The combination of 37% phosphoric acid and Transbond XT was the protocol selected by control group because of its efficacy and excellent values obtained when tested with other bonding materials 1,2,8,10,11,15,16,17,18,25,26.
Resin-modified glass ionomer cements (RMGIC) showed a shear bond strength value smaller than the resin material. Based on these results, one may assume that the low bond strength of Vitremer was probably because of the manufacturers recommendation of not performing enamel etching. The lack of microporosities on the substrate jeopardizes the formation of the mechanical bond between the enamel and Vitremer; therefore, bonding occurs only through chemical bond which should resist to mechanical efforts 5. Another reason may be the low cohesive resistance of the ionomer materials.
On the other hand, this low cohesive resistance may be beneficial because it may cause lesser damage to enamel surface than phosphoric acid etching, during debonding. This is because the highest pH of polyacrylic acid than phosphoric acid. This lower bond strength of RMGICs could constitute an advantage, once it facilitates the removal of the bonding materials remnants during enamel finishing and polishing; however, this may lead to the early debonding of the brackets, interfering in the treatment prognosis.
Despite of the fact that glass ionomer cements reduce the biochemical problem of caries lesions provoked by poor oral hygiene and their improvement regarding physical properties, doubts are still raised regarding the advantages of their use in brackets bonding 17,23.
According to the results of this present study, there were statistically significant differences between the brackets materials. The mean shear bond strength was always higher for ceramic than for metallic brackets. This can be attributed to the more effective light-curing in ceramic brackets because of their translucence, enabling greater light transmission to the bonding material and also because of the materials compatibility. Concerning to metallic brackets, incomplete light-curing of the bonding material could have happened below the brackets base because this material does not allow the correct light passage. According to Al-Saleh and El-Mowafy (2010) 2, even if greater time amounts were used, the authors did not reach a satisfactory light-curing.
Due to these aforementioned reasons, the results found by this present study are in agreement with numerous studies demonstrating that ceramic brackets show the highest bond strength values when compared with metallic brackets 1,2,7,25.
Concerning to the adhesive remnant index (ARI), in groups 1 and 3 (Transbond XT), the most found score was 3, showing that most of the fractures after debonding occurred at the composite/bracket interface and indicating the efficient bonding of the material to tooth substrate. On the other hand, in groups 2 and 4 (Vitremer), the most found scores were 0 and 1, indicating an unsatisfactory bonding of the material to tooth substrate.
These results are in agreement with many studies in literature, in which cohesive fractures occurred within the composite, that is, the material remains bonded to the enamel surface and consequently preventing the enamel from eventual traumas 8,15,16,20,21,25. This seems to be the fracture interface most favorable for a safe debonding because it demonstrates that the enamels cohesive force was higher than the bonding force between the bracket base and the adhesive. Therefore, the occurrence of enamel fractures is practically inexistent, and the removal of the residual adhesive is executed with the aid of specific burs which do not damage the tooth tissue 7,19.
ARI results showed by this study is of great interest because it enables the orthodontist to choose better materials presenting clinical responses with greater adhesive remnant on tooth surface after bracket debonding, which may be safer, avoiding enamel fractures and maintaining the tooths integrity 16.
Conclusion
Considering this studys methodology and results, it can be concluded that the ceramic bracket bonded with the orthodontic resin Transbond XT showed excellent shear bond strength results.
References
1. Abu Alhaija ESJ, Abu Alreesh IA, Alwahadni AMS. Factors affecting the shear bond strength of metal and ceramic brackets bonded to different ceramic surfaces. Eur J Orthod. 2010;32(3):274-380. [ Links ]
2. Al-Saleh M, El-Mowafy O. Bond strength of orthodontic brackets with new self-adhesive resin cements. Am J Orthod Dentofacial Orthop. 2010;137(4):528-33.
3. Årtun J, Bergland S. Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am J Orthod. 1984;85(4):333-40.
4. Buonocore MG. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res. 1955;34(6):849-53.
5. Chicri RO, Sasaki RT, Carvalho AS, Nouer PRA, Lima-Arsati YBO. Effect of enamel pretreatment on shear bond strength of brackets bonded with resin-modified glass-ionomer cement. J Orthod. 2010;11(1):11-5.
6. Di Nicoló R, Araujo MAM, Alves LAC, Souza ROA, Rocha DM. Shear bond strength of orthodontic brackets bonded using halogen light and light-emitting diode at different debond times. Braz Oral Res. 2010;24(1):64-9.
7. Fleischmann LA, Sobral MC, Santos Jr GC, Habib F. Estudo comparativo de seis tipos de brackets ortodônticos quanto à força de adesão. Dental Press Ortodon Ortop Facial. 2008;13(4):107-16.
8. Giannini C, Francisconi PAS. Resistência à remoção de brackets ortodônticos sob ação de diferentes cargas contínuas. Dental Press Ortodon Ortop Facial. 2008;13(3):50-9.
9. House K, Ireland AJ, Sherriff M. An in-vitro investigation into the use of a single component self-etching primer adhesive system for orthodontic bonding: a pilot study. J Orthod. 2006;33(2):116-24.
10. Ianni Filho D, Silva TBC, Simplício AHM, Loffredo LCM, Ribeiro RP. Avaliação in vitro da força de adesão de materiais de colagem em ortodontia: ensaios mecânicos de cisalhamento. R Dental Press Ortodon Ortop Facial. 2004;9(1):39-48.
11. International Organization for Standardization. ISO TR 11405 Dental Materials-guidance on Testing of Adhesion to Tooth Structure. Geneva, Switzerland: WHO; 1994. p. 1-13.
12. Melo TRNB, Maia AMA, Cavalcanti AL, Nascimento ABL, Valença AMG. Avaliação da resistência ao cisalhamento de adesivos monocomponentes em dentes bovinos. Odontologia Clín-Científ. 2006;5(4):275-80.
13. Menezes Filho PF, Marques CC. Adesão dos braquetes ortodônticos ao esmalte – revisão de literatura. International Journal of Dentistry. 2006;1(2):52-7.
14. Nakamichi I, Iwaku M, Fusayama T. Bovine teeth as possible substitutes in the adhesion test. J Dent Res. 1983;62(10):1076-81.
15. Pithon MM, Bernardes LAA, Ruellas ACO, Romano FL. Avaliação da resistência ao cisalhamento do compósito Right-On em diferentes condições de esmalte. R Dental Press Ortodon Ortop Facial. 2008;13(3):60-5.
16. Pithon MM, Oliveira MV, Santanna EF, Ruellas ACO. Avaliação da resistência ao cisalhamento do compósito Eagle Bond. Rev Saúde Com. 2007;3(2):3-9.
17. Pithon MM, Oliveira MV, Santos RL, Bolognese AM, Ruellas ACO. Avaliação in vitro da resistência ao cisalhamento e liberação de flúor de dois cimentos de ionômero de vidro reforçado por resina. Rev Odonto Ciênc. 2007;22(58):305-10.
18. Pithon MM, Santos RL. Shear bond strength of a new composite for orthodontic use under different situations. Braz J Oral Sci. 2009;8(1):34-7.
19. Pithon MM, Santos RL, Oliveira MV, Ruellas ACO. Estudo comparativo in vitro da resistência ao cisalhamento da colagem e do índice de remanescente adesivo entre os compósitos Concise e Fill Magic. R Dental Press Ortodon Ortop Facial. 2006;11(4):76-80.
20. Romano FL, Tavares SW, Ramalli EL, Magnani MBBA, Nouer DF. Análise in vitro da resistência ao cisalhamento de brackets metálicos colados em incisivos bovinos e humanos. R Dental Press Ortodon Ortop Facial. 2004;9(6):63-9.
21. Shinya M, Shinya A, Lassila LV, Gomi H, Varrela J, Vallittu PK et al. Treated enamel surface patterns associated with five orthodontic adhesive systems – surface morphology and shear bond strength. Dent Mater J. 2008;27(1):1-6.
22. Silva MF, Mandarino F, Sassi JF, Menezes M, Centola ALB, Nonaka T. Influência do tipo de armazenamento e do método de desinfecção de dentes extraídos sobre a adesão à estrutura dental. Rev Odontol Univ Cid São Paulo. 2006;18(2):175-80.
23. Sobrinho LC, Correr GM, Consani S, Sinhoreti MAC, Consani RLX. Influência do tempo pós-fixação na resistência ao cisalhamento de braquetes colados com diferentes materiais. Pesq Odontol Bras. 2002;16(1):43-9.
24. Tabrizi S, Salemis E, Usumez S. Flowable composites for bonding orthodontic retainers. Angle Orthod. 2010;80(1):195-200.
25. Uysal T, Ustdal A, Kurt G. Evaluation of shear bond strength of metallic and ceramic brackets bonded to enamel prepared with self-etching primer. Eur J Orthod. 2010;32(2):214-8.
26. Vicente A, Bravo LA, Romero M, Ortiz AJ, Canteras M. A comparison of the shear bond strength of a resin cement and two orthodontic resin adhesive systems. Angle Orthod. 2005;75(1):109-13.
27. Zachrisson BU. Clinical experience with direct-bonded orthodontic retainers. Am J Orthod. 1977;71(4):440-8.
 Correspondence:
Correspondence:
José Roberto de Oliveira Bauer
Universidade Federal do Maranhão (UFMA)
Departamento de Odontologia I, Curso de Odontologia
Rua dos Portugueses, s/n.º – Campus Universitário do Bacanga
CEP 65080-805 – São Luís – MA – Brasil
E-mail:bauer@ufma.br
Received for publication: August 04, 2011.
Accepted for publication: October 18, 2011.













