Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.9 no.2 Joinville Abr./Jun. 2012
Case Report Article
Surgical approach and the use of cryotherapy in a keratocystic odontogenic tumor after 12 months of decompression
Claudio Maranhão Pereira I Danilo Santos Carneiro II Renan Correia Arcanjo II Mauro Silva Filho II Flávio Augusto Cardoso da Silva III Alberto Ferreira da Silva Júnior II
I School of Dentistry, Paulista University – Brasília – DF – Brazil.
II School of Dentistry, Paulista University – Goiânia – GO – Brazil.
III School of Dentistry, São Leopoldo Mandic University – Campinas – SP – Brazil.
ABSTRACT
Introduction: The Keratocystic Odontogenic Tumor (KOT) is a pathology classified as an odontogenic cyst and began to be considered an odontogenic tumor in 2005, because of the presence of intrinsic characteristics compatible with neoplasm, such as its high rate of recurrence and differentiated mechanism of growth. Although its etiology is still unknown, its origin is believed to be related to the remnants of the dental lamina. Clinically it presents aggressive behavior and high rates of recurrence. Various types of treatment have been related, ranging from more conservative methods to radical surgery. With the goal of diminishing the potential for recurrence of these lesions, some authors have recommended the use of adjunct therapies such as peripheral osteotomy with burs, treatment of the surgical site with Carnoys solution, electrocauterization, cryotherapy and resection. Objective:The aim of the present study is to report the case of a patient with a KOT of large proportions in the mandible. Case report: Treatment was taken to perform decompression of the lesion for 12 months, and after this treatment comprised curettage and cryotherapy. Conclusion: This procedure is considered useful and conservative, as it avoids traumatisms to the noble structures close to the lesion.
Keywords: odontogenic tumors; odontogenic cysts; mandible.
Introduction
The term odontogenic keratocyst was used by some authors in the mid 1950s, to describe the cystic pathology with peculiar histologic characteristics and behavior. It was only in 1992 that the World Health Organization (WHO) ratified the nomenclature as a cyst whose development originated from remnants of the dental lamina, and attributed its aggressive behavior and high recurrence rates to this. It is represented by 10% of the odontogenic cysts 8,13.
Since 2005, the most recent classification (WHO) began to consider the odontogenic keratocyst as an entity classified within the group of odontogenic tumors 2,7. This entity, now designated as Keratocystic Odontogenic Tumor (KOT), received this denomination because of its aggressive behavior and high rates of recurrence, and began to be considered a true neoplasm 2.
Clinically KOT can present a large volume, capacity for expansion and fast growth 4. It has a predilection for the male gender, affects individuals in the second and third decades of life, and has a remarkable tendency to involve the posterior region and ascendant ramus of the mandible, sometimes associated with an impacted tooth 7,8.
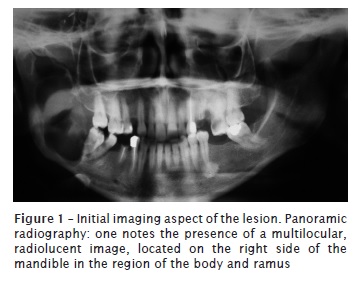
Radiographically, the lesions may present a unilocular or multilocular aspect due to their size. Thus, they generally present a radiolucent, multiloculated aspect with well defined limits associated with a dental crown 4,12.
Lesions such as the dentigerous cyst, ameloblastoma, calcifying odontogenic cyst, adenomatoid odontogenic tumor, central giant cells lesion and ameloblastic fibroma, due to their radiographic appearance, are considered differential diagnosis 1,3,4,12.
The most used treatment is enucleation followed by curettage; however, its friable nature associated with a thin fibrous conjunctive tissue makes it difficult to remove it completely 3. Various types of treatment have been suggested, ranging from more conservative methods to radical surgery. Curettage and marsupialization only are related to a large number of recurrences. Various adjunct therapies have been described to diminish the potential for recurrence of these lesions, including peripheral osteotomy with burs, treatment of the surgical site with Carnoys solution, electrocauterization, cryotherapy and resection 1,3,11. Decompression presents a high success rate in relation to aggressive treatments, as it promotes less morbidity and preserves important structures, such as bone structures, teeth and nerve endings 1,6,11.
Herein, we describe a case of a patient with KOT, in which decompression of the cystic lesion was performed for 12 months, and after it was performed the curettage followed by cryotherapy, preserving the inferior alveolar nerve, and thus, avoiding a possible pathological fracture.
Case report
The patient, a 36-year-old woman, appeared at the buccomaxillofacial surgery and traumatology service of the Goiânia General Hospital in October, 2009, complaining of an increase in volume in the mandible in the right posterior region about a year ago, without pain. Previous personal and family medical history was noncontributory as well the previous personal laboratory tests.
On extra-oral clinical exam, facial asymmetry was found, and nodular growth in the regions between the body and ramus of the mandible on the right side was observed. The lesion presented a rigid consistency and was painless on palpation.
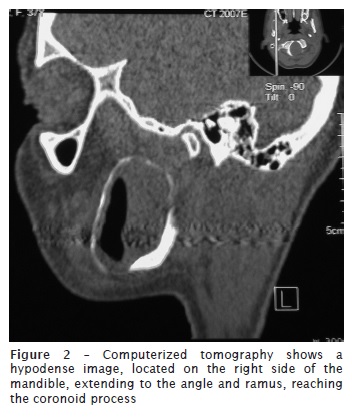
On intra-oral examination, it was observed a mass on the posterior right mandible region covered by normal mucosa. The ppanoramic radiography of the face, lateral oblique jaw and computed tomography exam was performed and, after evaluating the clinical and imaging exams, the diagnostic hypotheses of KOT, solid ameloblastoma and central giant cells lesion were reached.
Panoramic radiography, lateral oblique jawwwwand CT exams showed the presence of a hypodense, multilocular image, located on the right side of the mandible in the region of the body, extending to the angle and ramus, and reaching the coronoid process (figures 1 and 2).
Due to the large extension of the lesion, a more conservative treatment was proposed to the patient, preserving the important structures such as the inferior alveolar vascular-nervous bundle and integrity of the mandible basis. In November 2009, the patient was referred to the School of Dentistry of the Universidade Paulista de Goiânia, to have an incisional biopsy and lesion decompression.
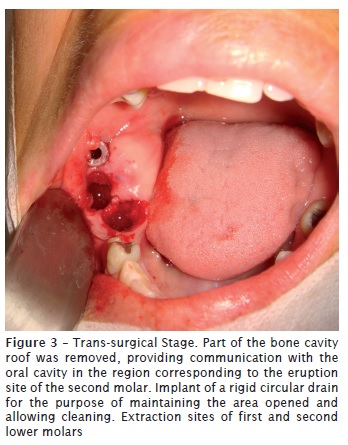
The surgical procedure was initially carried out with an aspiration to rule out possible intraosseous vascular lesion. It was performed an incisional biopsy on the right posterior mandible region. Part of the bone cavity roof was removed, providing communication with the oral cavity in the region corresponding to the eruption site of the second molar. In the space created by the removal of biopsy tissue a hard drain made of anesthetic plastic tube for dental use (without rubber diaphragm and plunger) was installed. This drain was placed in order to keep the region open and allow the cleaning of the cavity by repeated irrigation with saline solution at 0.9%. After 30 days, the extractions of teeth 47 and 48 were performed, as they were without bone support (figure 3).
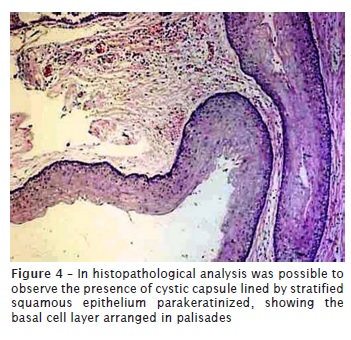
In the histopathological analysis it was possible to observe the presence of a cystic capsule of fibrous connective tissue, lined with parakeratinized, pavimentous stratified epithelium, exhibiting basal layer cells in a palisade arrangement and a corrugated surface layer. It was also possible to observe detachment of the epithelium from the subjacent connective layer and a keratin type of content, so that the diagnosis of a KOT tumor was reached (figure 4).
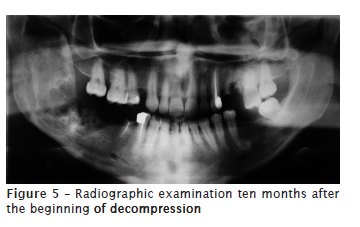
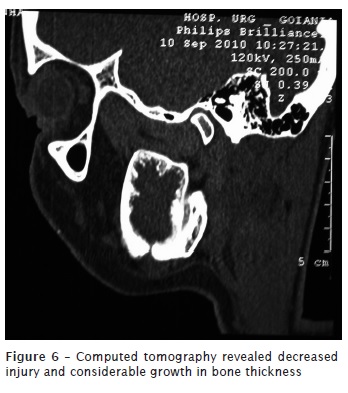
As post-operative care, the patient was recommended to perform strict oral cavity hygiene and cleaning of the cystic cavity by means of daily irrigation with 0.9% saline solution. Initially appointments were made for the patient to return weekly, and finally, at every two weeks. During each visit the cystic cavity hygiene was observed and reinforced. Three months after decompression began, it was noted that facial asymmetry had diminished considerably. Elimination of hyaline secretion was still noted without signs of infection. Imaging exams were requested for follow up, in which there was evident reduction in the cystic volume and increase in bone thickness that involved the lesion. Ten months after decompression had begun, there was no further report of drainage of secretions at the site. New radiographic exams were requested, in which it could be observed that the lesion had diminished and there was considerable growth of bone thickness (figures 5 and 6). In view of the result obtained by decompression, in November 2010, a proposal was made to the patient to have surgery performed in a hospital environment, under general anesthesia in order to perform curettage followed by cryotherapy. Intra-oral access was used for surgical removal of the lesion and after detachment the superior mandible cortically body, angle and ramus were removed with a spherical bur. Exhaustive and meticulous curettage was performed, the internal loculations were removed with the aid of spherical burs. After the procedure of curettage, nitrogen liquid in spray form was applied on the internal walls of the surgical recess in two 10-second applications, interspersed by a period of thawing for 2.5 minutes. The cystic capsule was shown to be very friable and all of its fragments were sent for anatomopathologic exam, confirming the diagnosis of KOT.
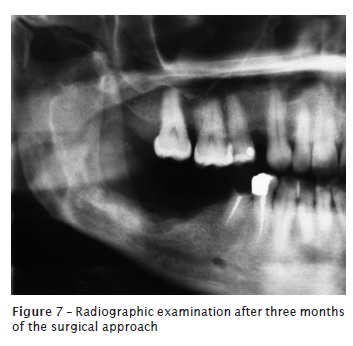
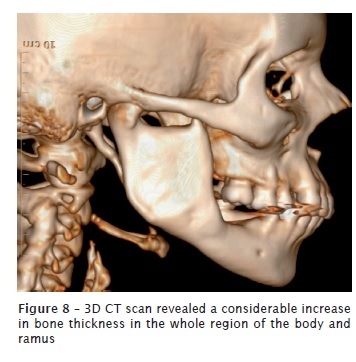
At present, the patient is still being followed-up, and about 3 months after the treatment, radiographic images have shown that the areas previously affected by the lesion have undergone bone regeneration, including visualization of the alveolar inferior canal. The referred nerve was preserved and the patient presented normal sensitivity in the lower lip on the surgery side (figures 7 and 8).
Discussion
KOT is an intraosseous cystic lesion of odontogenic origin, which presents a high rate of recurrence and predilection for the male gender. Increased volume and pain are clinical manifestations that vary according to the extension of the lesion 5,13. This case report corroborated the studies in literature, regarding to the most frequent age-range, most affected region and clinical manifestations, with the exception of the gender.
In large cases of KOT, the goal of conservative treatment with a special device (tube) used for decompression is to reduce the cyst as well as reinforce the thin cortical bone, with curettage being performed afterwards, in order to verify bone regeneration and non-recurrence of the lesion 6,11. According to some authors, therapy of this entity with peripheral osteotomy with or without the use of Carnoys solution (tissue fixer containing 6 ml of absolute alcohol, 3 ml of chloroform and 1 g of ferric acid) in the surgical recess for three minutes after enucleation, may reduce the chance of recurrence, and this may also be achieved with the use of cryotherapy 3,6,11.
Cryotherapy has been shown to be an important alternative for the treatment of intraosseous lesions, as it promotes a bone necrosis of approximately 2 to 3 mm, but maintains the inorganic matrix of the walls surrounding the lesion 9,10. The open system is extremely aggressive to the lesion, as the spray penetrates into the interior of the bone and the sudden and intensive cooling causes necrosis of the tumoral cells, which may have remained in the bone bed after curettage. Penetration into the bone and the induced cryonecrosis provide the safety margin required, and at the same time, this technique is described as conservative for the patient, since it prevents large segments or sections of the maxilla or mandible from being resectioned, thus avoiding large defects or mutilations in these patients 9. The surgical procedure adopted, considering the extension of the lesion, consisted of curettage followed by cryotherapy, because it is a more conservative technique. The technique adopted diminished the risks of reappearance of the lesion, and it is recommended in patients who are strictly followed up, as was the patient in this reported case.
The adopted technique has several advantages since it preserves anatomical structures adjacent to the lesion, favors the cystic capsule becomes thicker and capable of complete removal, and can be held up in an outpatient setting under local anesthesia. However, this technique has the major disadvantage of leaving the pathological tissue in situ, facilitating the development of secondary infections as a result of food debris left inside the lesion. So given the high rate of recurrence, it is mandatory to perform clinical and radiographic long-term follow-up, as in our case.
References
1. August M, Faquin WC, Troulis MJ, Kaban LB. Dedifferentiation of odontogenic keratocyst epithelium after cyst decompression. J Oral Maxillofac Surg. 2003;61:678-83. [ Links ]
2. Barnes L, Eveson JW, Reichart P, Sidransky D, editors. World Health Organization Classification of Tumours. Pathology and genetics of head and neck tumours. Lyon:Iarc Press; 2005.
3. Blanas N, Freund B, Schwartz M, Furst I. Systematic review of treatment and prognosis of the odontogenic keratocyst. Oral Surg Oral Med Oral Pathol. 2000;90(5):553-8.
4. Chirapathomsakul D, Sastravaha P, Jansisyanont P. A review of odontogenic keratocysts and the behavior of recurrences. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:5-9.
5. Forssel K, Forssel H, Kahnberg H. Recurrences of keratocysts in a long term follow-up study. Int J Oral Maxillof Surg. 1998;17:25-8.
6. Jung Y-S, Lee S-H, Park H-S. Decompression of large odontogenic keratocysts of the mandible. J Oral Maxillofac Surg. 2005;63:267-71.
7. Mateus GCP, Lanza GHSP, Moura PHR, Marigo HA, Horta MCR. Cell proliferation and apoptosis in keratocystic odontogenic tumors. Med Oral Patol Oral Cir Bucal. 2008;13:E697-702.
8. Morgan TA, Burton CC, Qian F. A retrospective review of treatment of the odontogenic keratocyst. J Oral Maxillofac Surg. 2005;63:635-9.
9. Pogrel MA. The management of lesions of the jaws with liquid nitrogen cryotherapy. J Calif Dent Assoc. 1995;23(12):54-7.
10. Pogrel MA. The use of liquid nitrogen cryotherapy in management of locally aggressive bone lesion. J Oral Maxillofac Surg. 1993;51(3):269-73.
11. Pogrel MA. Treatment of keratocysts: the case for decompression and marsupialization. J Oral Maxillofac Surg. 2005;63:1667-73.
12. Shear M. The aggressive nature of the odontogenic keratocyst: is it a benign cystic neoplasm? Part 1. Clinical and early experimental evidence of aggressive behaviour. Oral Oncol.2002;38:219-26.
13. Slootweg PJ. Odontogenic tumours – an update.Current Diag Pathol. 2006;12:54-65
 Correspondence:
Correspondence:
Claudio Maranhão Pereira
Faculdade de Odontologia da Universidade Paulista – Campus Brasília
Coordenação de Odontologia
SGAS Quadra 913, s/n.º – Conjunto B – Asa Sul
CEP 70390-130 - Brasilia - DF - Brasil
E-mail:claudiomaranhao@hotmail.com
Received for publication: February 17, 2011.
Accepted for publication: October 04, 2011.













