Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.9 no.4 Joinville Out./Dez. 2012
Original Research Article
Morphologic assessment of dental surface/ glass ionomer cement interface: influence of Er:YAG laser pretreatment
Aline Evangelista Souza-Gabriel I ; Daniela Thomazatti Chimello-Sousa I ; Regina Guenka Palma-Dibb I ; Jesus Djalma Pécora I ; Silmara Aparecida Milori Corona I
ABSTRACT
Introduction and objective: The aim of this study was to assess the surface and the substrate/glass ionomer cement (GIC) interface after Er:YAG laser irradiation by means of scanning electron microcopy. Material and methods: Thirty human third molars were selected and had their roots removed. Crowns were sectioned to obtain discs that were randomly assigned to three groups according to the surface pretreatment: 40% polyacrylic acid (control); Er:YAG laser irradiation (80mJ/2Hz) or Er:YAG laser followed by 40% polyacrylic acid. Two discs of each group were put aside to the surface analysis and the others were bisected. One half received Ketac-Fil and the other received Fuji II LC. Specimens were prepared for SEM and were analyzed under different magnifications. Results: Er:YAG laser group showed no adhesive interface for both enamel and dentin, but strongly damaged the interface build-up for dentin/Fuji II LC. The application of laser irradiation followed by the polyacrylic acid exhibited gaps and irregularities for both substrates. Conclusion: Er:YAG laser irradiation combined or not with 40% polyacrylic acid produced a surface unfavorable for GIC interaction, especially for the resin-modified ones.
Keywords: Er:YAG laser; glass ionomer cement; SEM.
Introduction
The development of new dental outfits and alternative techniques for teeth restoration are regarded to be relevant to obtain a better bonding between dental structure and restorative materials 2,7,17. Adhesion mechanisms of composite resin systems to dental surface by using acid etching are widely accepted and its efficiency is sufficiently proven 13,18. However, surface pretreatment with an acid or other technique prior to glass ionomer cement has not been included in the conventional procedure 4,9,22,23.
Polyacrylic acid is being used before glass ionomer cement restorations to remove only the smear layer without either demineralizing the dentin or removing the plugs 1,19,21. The calcium ions are kept available for chemical reaction with carboxyl ions of hydroxyapatite and allow the cement penetration into the hydrophilic substrate 19. Indeed, polyacrylic acid improves surface wettability, a prerequisite to effective adhesion 3.
In the last years, alternative techniques to treat enamel and dentin surface have been proposed, aiming to improve the adhesion of restorative systems to dental substrate 6,12,14,15. Among them, the irradiation of dental surface with the Er:YAG laser at low parameters can be highlighted 2,5,20.
During irradiation, the energy is absorbed by water molecules of organic dentinal structures, thus causing heating and water vaporization. The resulting pressure within the irradiated tissue leads to the occurrence of successive microexplosions that causes the ejection of both organic and inorganic particles 5,7,11,20. This process successfully occurs because of the Er:YAG laser wavelength of 2.94 μm that is coincident to the absorption pick of water and hydroxyapatite 7.
In dental structures, Er:YAG laser produces a micro-retentive pattern with cracks and fissures that helps the adhesion of resinous restorative materials 2,8. Some researchers reported the exposure of dentinal tubules 15,20 and appearance of "laser-modified layer" after laser treatment 20, but no alteration of calcium, phosphorus or oxygen contents were found 10.
Despite the effectiveness of Er:YAG laser for dental ablation 7, controversial results were verified considering the effects of lasing tooth structure before bonding restorative materials 2,15,23. Moreover, the literature is scarce in studies that report the use of Er:YAG laser in dental surface before the application of glass ionomer cements. Therefore, this study assessed the morphological aspect of dental substrate/glass ionomer cement interface (using both conventional and resinmodified products) and also the dentin and enamel surfaces after Er:YAG laser pretreatment, combined or not with polyacrylic acid, through scanning electron microscopy.
Material and methods
Caries-free thi rd molars, ext racted for orthodontics reasons and stored into 0.1% thymol solution at 9°C were washed in running water for 24 h to eliminate thymol residues and were examined at x10 stereoscopic magnifying glass (Carl Zeiss- Jena), discarding those with structural defects. Thirty molars were selected and their crowns were sectioned perpendicular to the long axis, in parallel sections, obtaining dentin discs of approximately 1 mm thick.
Smear layer was standardized by water glass paper in decreasing grit size (#280, #320, #400 and #600) for 30 seconds each.
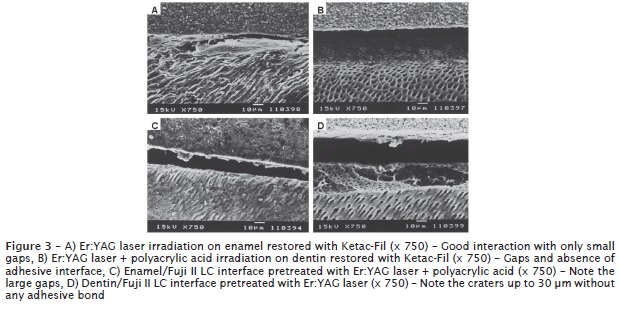
Discs were randomly assigned to two groups according to the glass ionomer cement used: conventional GIC (Ketac-fil, 3M/ESPE, Germany) and resin-modified GIC (Fuji II LC, GC Corporation Tokyo, Japan) (table I).
Following, the discs were subdivided into three subgroups according to the surface treatment procedure: 40% polyacrylic acid (Durelon liquid – 3M/ESPE), Er:YAG laser (Kavo Co., Biberach- Germany) and Er:YAG laser + polyacrylic acid.
The surfaces etched by polyacrylic acid were actively treated for 10 seconds. Next, the samples were washed in tap water and excess water was removed with absorbing paper, in order to obtain a moist surface.
For laser conditioning, Kavo Key Laser 2 (Kavo Co., Biberach-Germany) was used, comprising a high power output Er:YAG laser, with 2.94 μm wavelength, power output adjustable between 60 and 250 mJ, 1 to 5 Hz frequency, 250 to 500 μs pulse duration and 12 to 15 mm distance between the lens and target tissue. In this study, the laser beam was used in a defocused 8 non-contact mode at a 17 mm focal distance 11,14, 80 mJ power output, 2 Hz frequency and under constant refrigeration (3 ml/min).
After the surface treatment, each disc was bisected: one hemi section received the glass ionomer cement (1 mm thick), while the other was prepared for SEM analysis.
Specimens were sectioned in a perpendicular direction to the tooth/restoration interface and sanded with decreasing grit sand paper (#280, #320, #400, #600 and #1200) and thus, they were polished with alumina and diamond solution on silk fabric.
The samples were washed and immersed into a glutaraldehyde solution (2.5%) in sodium cacodilate (0.1M) buffer with a 7.4 pH, for 12 hours at 4°C. After being fixed, the samples were cleaned by ultrasound (Ultrasonic Cleaner T-1449-D, Odontobrás Ind. e Com.) for ten minutes to remove any residues from the bisected surface. Sequentially, it was performed the surface etching with 37% phosphoric acid (3M, Scotchbond Etchant) for 10 seconds. The samples were cleaned in distilled water, dried and finally dehydrated in increasing ethanol series of 20, 50, 75, 95 and 100% for 20, 20, 20, 30 and 60 minutes, respectively, and then immersed in hexamethyldisilazane (HDMS) for 10 minutes. The specimens were metalized with a fine gold overlay, submitted to SEM and photographed at different magnifications, so that the surfaces and the adhesive/enamel and adhesive/dentin interfaces could be qualitatively analyzed.
Results
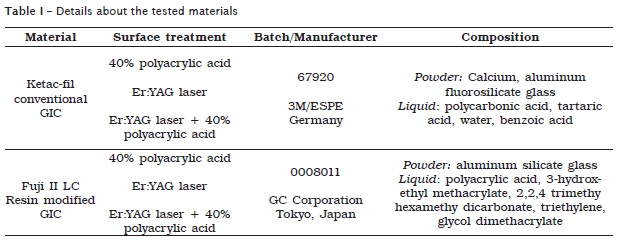
It was observed that the surface treatment with 40% polyacrylic acid produced micro-porosities in enamel and removal of the smear layer in dentin, but no complete removal of smear plug from dentinal tubules. The analysis of enamel/material interface revealed formation of an adhesive interface for Ketac-Fil (figure 1A) and an "intermediate layer" for Fuji II LC (figure 1C). The analysis of the dentin/ GIC interface revealed formation of small gaps for Ketac-Fil (figure 1B) and good interaction for Fuji II LC (figure 1D).
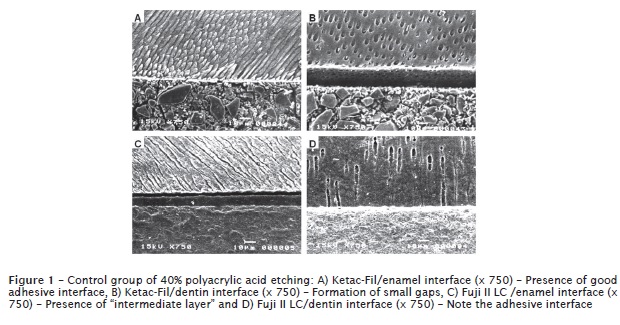
Er:YAG laser irradiation on enamel resulted in formation of a chipped irregular surface, without smear layer, some melting areas were also observed (figure 2A). For dentin, the surface became even more irregular, with open dentinal tubules and absence of smear layer (figure 2B). Surface treatment with Er:YAG laser combined with 40% polyacrylic acid produced for enamel an irregular and scaly surface (figure 2C), and for dentin a superficial aspect similar to the application of Er:YAG laser solely, with open dentinal tubules, absence of smear layer and fissures (figure 2D).
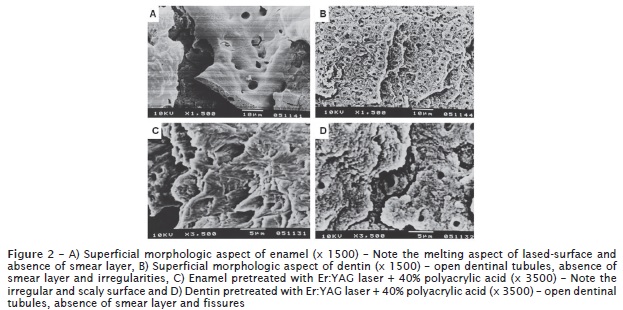
The combination Er:YAG laser with polyacrylic acid kept the adhesive interface similar to those that only received the laser application. In the interfaces analysis, it was verified a good interaction with only small gaps for enamel/Ketac-Fil pretreated with Er: YAG (figure 3A). For dentin/Ketac Fil, laser Er:YAG, combined or not with acid, produced and interface with gaps without any adhesive bond (figure 3B). The interface for enamel/Fuji II LC, pretreated with Er:YAG laser and acid also had evident gaps in the most of the specimens (figure 3C). In dentin pretreated with laser or laser/acid and restored with Fuji II LC, craters up to 30 μm without adhesive bond were found (figure 3D).
Overall, the analysis of the morphological aspects revealed that Er:YAG laser irradiation had stronger influence in the formation of an adhesive interface for GIC restorative material, regardless of the subsequent application of polyacrilic acid.
Discussion
Glass ionomer cement bonds to tooth structure via direct chemical bonding without using any adhesive system 16,24. To improve the adhesion of this material, pretreating the dentin surface with a conditioner is recommended 9,21.
In this study, it was verified that the superficial morphology of enamel and dentin irradiated by Er:YAG laser, whether combined or not with acid conditioning, was different from those achieved by conventional conditioning with polyacrylic acid. Er: YAG laser pretreatment resulted in another type of adhesive interface that impaired the ionomer cements, mainly in dentin substrate.
This outcome can possibly be explained by the stronger action of laser on dentin, rather than on enamel 11,23. Such difference of action on the substrates is because of a greater water content from dentinal tubules and a smaller rate of hydroxyapatite in dentin as compared to enamel 13,18. On the other hand, dentin is a less favorable substrate than enamel for adhesion due to its tubular structure, significant water content, occurrence of microstructural alterations and greater rate of organic matrix 18.
It is known that the Er:YAG laser irradiates at the 2.94 μm wavelength, which is very near to water absorption wavelength, therefore a strong absorption of the radiated energy up to water vaporization occurs 2,7. A quick shock wave develops, causing expansion of the tissues followed by micro-explosions that eliminate micro-particles able to remove the dental tissue and leave behind a rough surface 2,23. So, the laser-irradiated substrate exposed an irregular surface, with microcracks, fissures and crater formation, absence of a smear layer and open tubules in dentin 20. Other authors also found this morphological aspect on Er:YAG lased-dental 15,20 and Ceballos et al. 5 reported denatured collagen fibers. All these morphological characteristics of the substrate may have impaired the bonding of ionomer cements, specially the resin-modified ones.
Conventional glass ionomer cement (Ketac-Fil) adheres to enamel and dentin by chelation of the polyacid carboxylic groups to hydroxyapatite calcium 19, so it is possible that this chemical reaction is not impaired by the superficial irregularities caused by laser irradiation as it does not modify the chemical composition of dental substrates 24. Nevertheless, resin-modified glass ionomer cement (Fuji II LC) may have had its adhering mechanism hampered by laser irradiation, because its adhesion process is chemical as in conventional glass ionomer cement; however, it needs an additionally mechanical micro-retention 1 to a well-structured organic matter, so that the resinous components (HEMA) can penetrate the collagen fiber interstices to form the hybrid layer 24.
The combination Er:YAG laser with polyacrylic acid kept the adhesive interface similar to those that only received the laser application. Surface morphology is similar, with open dentinal tubules 23 and probably increasing dental substrate permeability, which could impair the adhesion of glass ionomer cement to dentin. A recent study concluded that surface treatment with phosphoric acid or Er,Cr:YSGG laser increased the bond strength of GIC to composite resin 17.
It should be noticed that that clinical applications of Er:YAG laser is rather distant from those of the laboratory experiments. Depending on the parameter settings used, a specific laser morphological pattern should be expected. Therefore, despite of the divergences as to the morphological appearance of dental surface after Er:YAG laser irradiation, there are important questions of safety, efficacy and substrate interaction with different types of restorative materials that should be analyzed before such technique can be considered as technically feasible.
Conclusion
Based on the microscopic observations and according to the tested parameters, it can be concluded that Er:YAG laser application, whether combined or not to 40% polyacrylic acid, produces an unfavorable surface for the interaction of glass ionomer cements, especially the resin-modified ones.
Acknowledgment
To the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) for financial support.
References
1. Abdalla AI. Morphological interface between hybrid ionomers and dentin with and without smearlayer removal. J Oral Reabil. 2000;27(9):808-14. [ Links ]
2. Amaral FL, Colucci V, Souza-Gabriel AE, Chinelatti MA, Palma-Dibb RG, Corona SA. Bond durability in Erbium:yttrium-aluminumgarnet laser-irradiated enamel. Lasers Med Sci. 2010;25(2):155-63.
3. Atmeh AR, Chong EZ, Richard G, Festy F, Watson TF. Dentin-cement interfacial interaction: calcium silicates and polyalkenoates. J Dent Res. 2012;91(5):454-9.
4. Bishara SE, Vonwald L, Laffoon JF, Jakobsen JR. Effect of altering the type of enamel conditioner on the shear bond strength of a resin-reinforced glass ionomer adhesive. Am J Orth Dent Orth. 2000;118(3):288-94.
5. Ceballos L, Osorio R, Toledano M, Tay FR, Marshall GW. Bonding to Er:YAG laser treated dentin. J Dent Res. 2002;81(2):119-22.
6. Cooper LF, Myers ML, Nelson DGA, Mowery AS. Shear strength of composite bonded to laserpretreated dentin. J Prosth Dent. 1988;60(1):45-9.
7. Corona SA, Souza-Gabriel AE, Chinelatti MA, Pécora JD, Borsatto MC, Palma-Dibb RG. Influence of energy and pulse repetition rate of Er:YAG laser on enamel ablation ability and morphological analysis of the laser-irradiated surface. J Biomed Mater Res. 2008;84(3):569-75.
8. Delmé KI, Deman PJ, De Bruyne MA, De Moor RJ. Microleakage of four different restorative glass ionomer formulations in class V cavities: Er:YAG laser versus conventional preparation. Photomed Laser Surg. 2008;26(6):541-9.
9. Ekworapoj P, Sidhu SK, McCabe JF. Effect of surface conditioning on adhesion of glass ionomer cement to Er,Cr:YSGG laser-irradiated human dentin. Photomed Laser Surg. 2007;25(2):118-23.
10. Gómez C, Bisheimer M, Costela A, García- Moreno I, García A, García JA. Evaluation of the effects of Er:YAG and Nd:YAG lasers and ultrasonic instrumentation on root surfaces. Photomed Laser Surg. 2009;27(1):43-8.
11. Hossain M, Nakamura Y, Yamada Y, Kimura Y, Nakamura G, Matsumoto K. Ablation depths and morphological changes in human enamel and dentin after Er:YAG laser irradiation with and without water mist. J Clin Laser Med Surg. 1999;17(3):105-9.
12. Liberman R, Segal TH, Nordenberg D, Serebro LI. Adhesion of composite materials to enamel: comparison between the use of acid and lasing as pretreatment. Lasers Surg Med. 1984;4(4):323-7.
13. Manuja N, Nagpal R, Pandit IK. Dental adhesion: mechanism, techniques and durability. J Clin Pediatr Dent. 2012;36(3):223-34.
14. Markovic D, Petrovic B, Peric T, Miletic I, Andjelkovic S. The impact of fissure depth and enamel conditioning protocols on glass-ionomer and resin-based fissure sealant penetration. J Adhes Dent. 2011;13(2):171-8.
15. Martinez-Insua A, Da Silva Dominguez L, Rivera FG, Santana-Penin UA. Differences in bonding to acid-etched or Er:YAG-laser-treated enamel and dentin surfaces. J Prosthetic Dent. 2000;84(3):280-8.
16. Mickenautsch S. Research gaps identified during systematic reviews of clinical trials: glass-ionomer cements. BMC Oral Health. 2012;12(1):18-29.
17. Navimipour EJ, Oskoee SS, Oskoee PA, Bahari M, Rikhtegaran S, Ghojazadeh M. Effect of acid and laser etching on shear bond strength of conventional and resin-modified glass-ionomer cements to composite resin. Lasers Med Sci. 2012;27(2):305-11.
18. Pashley DH. Dentin: a dynamic substrate – a review. Scanning Microsc. 1989;3(1):161-74. 19. Powis D, Folleras T, Merson SA, Wilson AD. Improved adhesion of glass ionomer cement to dentine and enamel. J Dent Res. 1982;61(12):1416-22.
20. Souza-Gabriel AE, Chinelatti MA, Borsatto MC, Pécora JD, Palma-Dibb RG, Corona SA. SEM analysis of enamel surface treated by Er:YAG laser: influence of irradiation distance. Microsc Res Tech. 2008;71(7):536-41.
21. Tanumiharja M, Burrw MF, Tyas MJ. Microtensile bond strength of glass ionomer (polyalkenoate) cements to dentine using four conditioners. J Dent. 2000;28(5):361-6.
22. Tay FR, Smales RJ, Ngo H, Wei SH, Pashley DH. Effect of different conditioning protocols on adhesion of a GIC to dentin. J Adhes Dent. 2001;3(2):153-67.
23. Visuri SR, Gilbert JL, Wright DD, Wigdor HA, Walsh JT. Shear strength of composite bonded to Er:YAG laser-prepared dentin. J Dent Res. 1996;75(1):599-605.
24. Xie D, Brantley WA, Culberston BM, Wang G. Mechanical properties and microstructures of glassionomer cements. Dent Mat. 2000;16(2):129-38.
 Correspondence:
Correspondence:
Aline Evangelista Souza-Gabriel
Av. Portugal, n. 1.690, apto. 84 – Jardim São Luis
CEP 14020-380 – Ribeirão Preto – SP – Brasil
E-mail: aline.gabriel@gmail.com













