Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.9 no.4 Joinville Out./Dez. 2012
Original Research Article
Health risks and complications associated with the use of intraoral and perioral piercing: knowledge of young adults
Gerônimo Schettert Fortes I ; Tommy Luiz Rasmussen I ; Constanza Marin I ; Elisabete Rabaldo Bottan I
ABSTRACT
Objective: The aim of this study was to identify the knowledge of young adults on health risks and complications associated with the use of intraoral and perioral piercing. Material and methods: A descriptive transversal study using primary data. The study group comprised individuals with 18 years of age or more who were found in collective spaces, in the urban perimeter of Balneário Camboriu (Santa Catarina). The probabilistic sample was calculated as infinite population, defining a margin of error of 5%. The survey data were collected through an in-person structured questionnaire. Results: 395 individuals (39.5% male; 60.5% female) participated in the research, with ages ranging from 18 to 26 years-old. Most of the individuals (74.2%) have medium level of education. Six percent (6%) were or had been using oral piercing. Sixty-seven percent (67%) did not have received any information about the possible implications for health, as a result of the use of oral piercing; however, 89.7% believed that the use of this accessory offered risks to health. The percentage of users of oral piercing in the group was 6%, among which 93% told that they had observed some type of alteration as a result of the use of oral piercing. Conclusion: Most of the participants of this research did not have suitable knowledge on the health risks, as a result of the use of an oral piercing. Therefore the accomplishment of information campaigns for general population is fundamental, in which the -dentist must play a significant role.
Keywords: knowledge; body piercing; health promotion.
Introduction
The word piercing derives from the word pierce which means to penetrate, to perforate. Therefore, the perforation of the skin and its underlying layers aiming to insert an object, generally constructed with some type of metal, is called piercing. It is an ancient practice adopted for more than five thousand years in Indonesia, Rome, and Egypt and societies as the American Indians, African tribes and aristocrats of the Middle Ages. This habit gained popularity among young adults of several socioeconomic layers worldwide. Several reasons account for the use of these accessories: need of social inclusion, wide dissemination by the media, reduction of the prejudice in relation to their users who until little time were seen as marginalized people 1,3,5,6,8,16,27.
The accessory is considered as a form of intraoral injury, from the Dentistry point of view. Even performing a good oral hygiene, the users are not free of some alteration type, These oral perforations exhibit a potential for complications ranging from swelling to cancer lesions, depending on the site of placement, type of accessory, sterilization of the material used, experience of the professionals executing the perforations, and the general health of the patients 2,9,16.
The installation and use of piercings may be related to transitory alterations and irreversible problems, with oral and systemic repercussion. Several side effects coming from the installation of these accessories may be harmful to local structures, such as: infect ion, format ion of hypertrophic healing, gingival recession and dental fractures. Other complications reported have been: deglutition of the piece, halitosis, hepatitis, allergic processes, and bleeding. Oral piercings have been also related to the risk of the development of endocarditis because the perforation enables that the numerous microorganisms within oral cavity come in the bloodstream and be housed in the heart of the susceptible patients 1,5,7,12,16,17,28.
Considering the importance of the information on this issue, this present study aimed to identify the knowledge of young adults from the city of Balneario Camboriu, (Santa Catarina, Brazil) on the health risks of the use of oral.
Material and methods
This Project was submitted and approved by the Ethical Committee in Research of the University of Itajai Valley, under protocol number 255/10.
This study was characterized as a descriptive, transversal research through primary data collect ion. The target populat ion comprised individuals aging from 18 to 26 years-old who were in locals of public circulation, in the central perimeter of Balneario Camboriu, city of Santa Catarina, Brazil.
To determine the sampling plan, the population was considered as infinite by defining a margin of error of 5%. Thus, the minimum number of individuals for sampling composition was calculated in 304. The sample was randomly selected according to the following inclusion criteria: a) to present physical and mental conditions to understand the questions of the instrument of data collection; b) to have age between 18 and 26 years-old; c) to read, understand and sign a Free and Clarified Consent Form to participate in the research.
The instrument of the data collection was a questionnaire composed of close, dichotomous, multiple-choice questions divided into two parts. The first part comprised three questions aiming to the socio-demographic characterization of the participants (gender, age and degree of scholarity). The second part comprised seven questions on the aspects regarding to the knowledge on the use of the piercing and its relationship with health.
Previously to the execution of the research, a pilot study was conducted with 20 individuals who met the inclusion criteria of the research. The aims of the pilot study were: to validate and adapt the instrument of data collection regarding to the presentation form and difficulties of comprehension and to calibrate the researchers.
The pilot study did not evidence the need of reformulating the instrument questions of data collection. Notwithstanding, we opted not to include these questionnaires in the final study.
The calibration of the examiners comprised the orientation about how to approach the participants and the essential caution to the questionnaire application. The examiners were oriented as follows: to read each question slowly; to record exactly the answers without exerting any type of influence on the participant; to repeat the question with the participant did not understand it; and to move to the next question whether the participant did not answer the present question. The questionnaire was applied during the period of April to June of 2011.
Data were tabulated and organized with the aid of Microsoft Excel 2007 software, to obtain the relative frequency of the answers of each question. Data were exhibited as descriptive analysis.
Results
Three hundred and ninety-five individuals participated in the research, of which 39.5% were male and 60.5% female. The age of the participants ranged from 18 to 26 years-old: 43.8% were at the age-range from 18 to 20 years and 56.2% were at 21 to 26 years. Most of the participants (74.2%) has o middle school, 11.6% were enrolled in high school, and 14.2% has junior school.
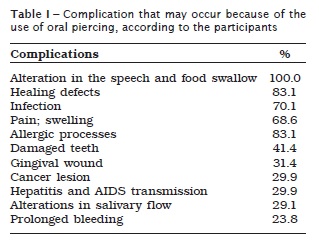
Among the participants, 67% reported they did not receive information on the possible health implication because of the use of oral piercing. However, 89.7% believed that the use of this accessory may injure their health. From a list of possible complications presented, the following items were highl ighted: speech alterat ions, difficulty of swallowing food, defects of healing and infection. The frequencies of answers on the possible complication associated with the use of oral piercing are seen in table I.
A low percentage (6%) of the participants affirmed to use oral piercing, of which 74% were placed on the tongue and 26% on the tooth. All users of piercing on the tongue placed it with a body piercing professional and the users of tooth piercing had it placed by a dentist.
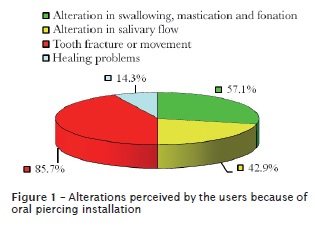
The time of the use of the piercing ranged from 6 months to 6 years. A very higher percentage (93%) of the users reported they observed any type of alteration because of the use of the accessory (figure 1).
Discussion
Likely to the ancient people who performed body ornamentation with several meanings (religious, sexual, or marital), current young adults use this jewelry with the aim to decorate their appearance, express themselves, or even to identify themselves with some sociocultural groups 1,8,10,13,27.
Oral and perioral piercings, currently have been pointed out as the most used. They may be placed on the tongue, lip mucosa, lip frenulum and cheeks; the first two aforementioned sites have been the most found and described as the probable etiological agents accounting for traumas in oral tissue 6,10,14,19,21,23,24. The findings of this present study corroborate the data reported in the literature, because piercing on the tongue was the most prevalent among the individuals who affirmed that they use or had used piercing.
The studies on the use of these accessories do not still indicate the real number of users; however, some studies have evidenced their frequency in some populations. In the United States of America (USA), between 17% and 51% of the undergraduate students have either tattoo or piercing 5,15. An investigation conducted on subjects aging between 18 and 50 years, also in USA, identified that 8% of the participants used or had used piercing at an area of the mouth 14. In Helsinki (Finland), in a sample of undergraduate students, it was observed that 3.4% had the accessory 26. In Buffalo (New York), a research conducted in five schools recorded that 10% of the teenagers used the accessory 19. In the city of Rosário (Argentine), among teenagers and young adults the frequency was of 36.9% 2. In São José dos Campos (São Paulo, Brazil), a study conducted with students between 14 and 18 years reported a frequency of 3.6% 11.
The procedure of the accessory installment and its use puts health at risk and causes adverse consequences. Consequently, even if the percentage of users is low, this fact deserves special attention because the complications are significant. Notwithstanding, in this study most of the participants did not receive any information on the possible reactions. Although several participants had admitted that oral piercing may cause alterations in the body, they ignored how the accessory would interfere in health conditions.
The placement of these accessories on the soft tissues of the oral cavity, especially the tongue and lips, may cause systemic complications. After the procedure of installation, the associated complications are: pain, swelling, infections, bleeding, and hematomas. Long-term effects have been observed as gingival recessions, mainly in cases of lip piercings 5-7,12-14,16,17,19,21,22,26,28.
Reactions such as increasing of saliva, bleeding, difficulty to chew and speak, formation of galvanic current, tooth fracture, hyperplasia of the tissue and gingival trauma have been the most common reactions when the accessory is installed on the tongue or jugal mucosa 3-7,10,13-20,22,26,28.
Still, there have been reports that oral or perioral piercing is associated with the accumulation of calculus, halitosis, streptococcal endocarditis and thrombophlebitis of the sigmoid sinus. Because the accessory causes a chronic trauma, its association with smoking and alcohol (carcinogenic factors) may contribute to the occurrence of oral cancer 1,4,5-7,12,25.
Some authors reported that the piercing on the orofacial region may cause problems in cases of hospitalizations demanding orothracheal intubation or the use of electrocautery 16,17,23.
Among the complications associated with the use of oral piercing noted by the participants and found by the literature: tooth fracture and movement, speech alteration, difficulty in swallowing and mastication.
Thus, the findings of this research – lack of information and report of the alterations caused by the use of the accessory –, which were also found by the other studies, reinforce the importance that the previous appointment with a doctor or dentist to understand the complications and cautions with the hygiene of the site of installment.
The physical conditions should be previously considered. It should be known that the person exhibits diabetes, heart disease or other disease contraindicating the use of this type of accessory. However, most of the persons do not take this care because they do not have this knowledge. Generally, the installment of the piercing is performed by the body piercing professional or piercers, situation which was confirmed by this study. This professional, in several times, does not have the professional qualification, know the human anatomy and the systemic conditions of the patient and the correct methods of sterilization and asepsis. Moreover, they do not have a license for using either local anesthetics or prescribing postoperative medication; consequently, complications such as pain and swelling are common 15,25.
In view of the innumerous adverse situations which may occur due to the placement of this type of accessory, it is recommended that the piercing installment be performed by professionals regulated by the government because that during the perforation there is the risk of disease transmission such as AIDS, herpes and hepatitis 5,14.
The user or the person wanting to use these accessories need to be clarified on the risks to which is exposed, through the correct and clarified orientation by health area professional. The procedure of the perforation should be executed by qualified professional and it demands the regular appointment with the dentist for a systematic followup, assuring therefore the early detection of adverse effects associated with this practice. Accordingly, the Brazilian National Board of Dentistry intend to interfere in this situation, because the dentist is responsible for alerting the population on the importance regarding to the conscious use of this type of this accessory 4.
Other fact found by this research which should be highlighted is regarded to the use of tooth piercing. Although the word twinkles has been incorrectly employed because there is no perforation, the literature has highlighted that it is a healthier alternative 9,13,15,21. Unlikely to oral piercings, tooth piercing is an extremely simple, noninvasive procedure which does not damage the oral mucosa, cause pain, and it can be removed without leaving any type of vestige. The main care is regarding to the plaque accumulation; therefore it should not be indicated to patients at high risk for caries 9,13,15,21.
Accordingly, by considering that the practice of the use of this accessory has gain increasingly popularity in the last years, it is necessary that the dentists be prepared to treat the problems caused by its use and to provide information on the health risks 1,9,13-17,20,21,23,28.
Because of this, it is of extreme importance that the offer of campaigns be stimulated and the dentist has an important role in this. It is necessary that the dentists act preventively and guide the users on the risks and care involved by proposing public policies aiming to the regulamentation and supervision of the professionals performing the perforation of piercing installment in their offices, therefore collaborating with the health promotion of the individuals.
Conclusion
Considering the aim of this study and the results obtained, it can be concluded that most of the participants did not exhibit an adequate knowledge on the health risks because of the use of oral and perioral piercing.
Acknowledgements
We thank to the Program of Scientific Initiation Scholarship of the Dean of Research, Post- Graduation, Extension and Culture of Univali by supporting the research.
References
1. Alves LV, Silva AMB, Fonseca ACL, Miranda MS. Problemas relacionados com o uso de piercing na língua – relato de caso. Adolesc Saúde. 2011; 8(1):59-62.
2. Amato R, Morero S, Leto D, Borra V. Adolescencia: piercings y tatuajes como indicadores de riesgo. 2010 [cited 2011 May 20].Availablefrom:URL:http//www.iracian.com.ar/.../ADOLESCENCIA%20PIERCIG%20Y%20TATUAJES%20COMO%20INDI CADORES%20DE%20RIESGO%20WEB[1].pdf.
3. Clavería Clark RA, Ortiz Moncada C, Fouces Gutiérres Y, Tabateres Urdanete RR, Muñoz Torres Y. Cuidado con los piercings bucales. Medisan. 2009;13(3).
4. Cont i MCS. Uso do piercing bucal e a responsabilidade odontológica. 2005 [cited 2010 May 27]. Available from: URL:http://www.nagib. net/arquivos/ArtigoPiercingBucal.doc.
5. Dubose J, Pratt JW. Victim of fashion: endocarditis after oral piercing. Curr Surg. 2004;61(5):474-7.
6. Espírito Santo RA, Santos LFG, Conceição JG, Pontes JRM, Israel MS, Ramos MEB. Piercing oral: fator de risco para o câncer? Rev Ciênc Med Biol. 2007;6(2):233-9.
7. Fenato MC, Miura CSN, Boleta-Ceranto DCF. Piercing bucal: sua saúde vale esse modismo? Arq Ciênc Saúde Unipar. 2010;14(2):157-61.
8. Ferreira VS. Tatuagem, body piercing e a experiência da dor: emoção, ritualização e medicalização. Saúde Soc. 2010;19(2):231-48.
9. Feuzer L, Monteiro Junior S, Araújo E. Piercing: um adorno para o corpo, um adorno para os dentes. Rev Dental Press Estet. 2007;4(1):50-62.
10. Fragelli CMB, Campos JADB, Gaspar AMM. Considerações sobre o uso do piercing lingual. RGO. 2010;58(4):451-5.
11. Firoozmand LM, Paschotto DR, Almeida JD. Oral piercing complications among teenage students. Oral Health Prev Dent. 2009;7(1):77-81.
12. Henneguin-Hoenderdos NL, Slot DE, Van Der Weijden GA. Complications of oral and peri-oral piercings: a summary of case reports. Int J Dent Hyg. 2011;9(2):101-9.
13. Jeger F, Lussi A, Zimmerli B. Oral jewelry: a review. Schweiz Monatsschr Zahnmed. 2009;119(6):615-31.
14. Lauman AE, Derick DJ. Tattoos and body piercings in the United States: a national data set. J Am Acad Dermatol. 2006;55:413-21.
15. Marquezan M, Souza LT, Tanaka O. Piercing oral: beleza, riscos e o papel da odontologia. Rev Fac Odontol Porto Alegre. 2008;49(1):12-5.
16. Maheu-Robert LF, Andrian E, Grenier D. Overview of complications secondary to tongue and lip piercings. JCDA. 2007;73(4):327-31.
17. Moor R, Witte A, Delmé K, Bruyene M, Hommez G. Dental and buccal complications of lip and tongue piercing. Rev Belg Med Dent. 2007;62(2):104-12.
18. Mustelier Ferrer HL, Gala Vidal H, Bertrán Bahades J, Ortiz Angulo L, Cuñat Ramírez L. Piercing: moda inofensiva? Medisan. 2007;11(4).
19. Pearose MM, Perinpanayagam MK, Wells MD. Trends in oral piercing in Buffalo, New York, high schools. N Y State Dent J. 2006;72(5):30-2.
20. Pécora GA, Reyes A, Pedron IG, Utumi ER, Borsatti MA. Complicações decorrentes da utilização do piercing bucal – avaliação e conduta clínica. Odonto. 2010;18(36):51-7.
21. Samplonius A. Piercing oral: nuevas tendencias en odontología cosmética. Vision Dental Revista Estomatológica Peruana. 2006;9(33).
22. Santiago LM, Santana AF, Aguiar CRB, Santos EV. Alterações intra-bucais causadas pelo uso do piercing. Odontologia Clín-Cient. 2007;6(2):143-6.
23. Saquet PN, Saleh SB, Marchiori JC, Pozzobon R. Perfil dos usuários de piercing oral e implicações decorrentes de seu uso. RGO. 2009;57(1):41-5.
24. Silva ER, Oliveira Junior JP. Piercing oral e perioral: revisão bibliográfica. Biosci J. 2005;21(2):115-22.
25. Soares LP, Oliveira MG, Ferreira ICSR. Reação de corpo estranho causada por piercing oral. Rev Bras Patol Oral. 2004;3(2):88-91.
26. Ventä I, Lakoma A, Haahtela S, Peltola J, Ylipaavalniemi P, Turtola L. Oral piercings among first-year university students. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:546-9.
27. Vieira EP, Ribeiro AL, Pinheiro JD, Alves Júnior MS. Oral piercings: immediate and late complications. J Oral Maxillofac Surg. 2011;69(12):3032-7.
28. Ziebolz D, Stuehmer C, Nüss K, Hornecker E, Mausberg RF. Complications of tongue piercing: a review of the literature and three case reports. J Contemp Dent Pract. 2009;10(6):E65-71.
 Correspondence:
Correspondence:
Elisabete Rabaldo Bottan
Av. Atlântica, n. 1.020, ap. 1.801
CEP 88330-006 – Balneário Camboriú – SC – Brasil
E-mail: erabaldo@univali.br













