Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.9 no.4 Joinville Out./Dez. 2012
Short Communication
Review of pulp therapy in primary teeth
Allan Abuabara I ; Bruno Monguilhott Crozeta II ; Flares Baratto-Filho III,IV
II Graduate Student of the Master Course in Clinical Dentistry with emphasis on Endodontics and Specialization in Endodontics, Positivo University – Curitiba – PR – Brazil
III Department of Dentistry, University of the Region of Joinville – Joinville – PR – Brazil
IV Department of Dentistry, Positivo University – Curitiba – PR – Brazil
ABSTRACT
Introduction: It is extremely important for the dentist the knowledge of the signs and symptoms caused by inflammation of the pulp of primary tooth, especially when the issue is either to keep or extract it. Objective: To develop a guide to assist dentists in the diagnosis and management of pulp therapy of primary teeth. Methodology: The protocols of the American Association of Pediatric Dentistry (reviewed in 2009), the British Society of Pediatric Dentistry (reviewed in 2006) and Cochrane Library (August of 2011) were sought for the best evidence to assist managers and professionals in the most appropriate decisions for their patients. Conclusion: Regardless of the decision concerning to the primary tooth and to the different treatment modalities, attention should be directed to the prognosis of the tooth in question, by restoring its health and function.
Keywords: primary teeth; pulpotomy; conservative treatment.
Introduction and methodology
The first decision regarding to the primary tooth should be either to keep it or extract it. For standardization, the signs and symptoms caused by pulp inflammation are history of spontaneous pain, especially at night; pain when chewing; fistula; history or increasing of swelling in the face, need for analgesics.
• Keep the tooth: systemic factors that contraindicate extraction (risk of bleeding, as in the case of hematological diseases, uncontrolled cardiac abnormalities or without prior medical contact); agenesis of the permanent tooth, and thus preserving the space for the eruption of the permanent teeth.
• Extraction: patient at risk for systemic infection, e.g., endocarditis or immunosuppressed patient (see protocol for antibiotic prophylaxis); non-restorable tooth; more than 2/3 of root resorption; acute infection.
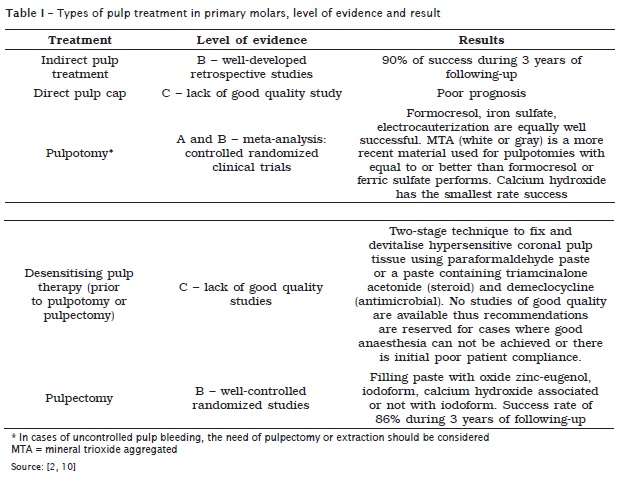
Types of treatment (table I):
1. Indirect pulp capping (level of evidence B – descriptive retrospective or well-conducted studies): The goal of the treatment is to stop the progression of caries and form a reactionary dentin. It is indicated in carious lesions without signs and symptoms of pulpal pathology. All caries at the enamel-dentin junction should be removed. The caries should be removed by using hand curettes or excavators. The soft carious tissue from the bottom wall should be carefully removed to avoid the pulp. Sealing of the cavity with either glass ionomer or zinc oxideeugenol cement. A superficial resin sealing should be performed to prevent leakage. A success rate of 90% in maintaining the tooth is expected, without signs and symptoms, during a period of 3 years.
2. Direct pulp capping (level of evidence C – lack of good quality study. Based on clinical experience or expert consensus): very limited technique which has been not normally indicated in primary molars. The aim is to form a dentinal bridge in the pulp exposure site. It may be attempted in small traumatic pulp exposures. During the procedure, the bleeding should be controlled with cotton pellet moistened with saline solution, followed by the application of a calcium hydroxide paste or MTA and sealing of the crown . The prognosis is generally poor.
3. Pulpotomy (evidence A and B – meta-analysis: controlled randomized clinical trials): it consists in removing the coronal pulp and maintaining the root pulp. The coronal pulp irreversibly inflamed is removed and the root pulp reversibly inflamed is preserved. It is indicated in asymptomatic teeth or with transitory pain, without signs of periradicular pathology. Preferentially, the coronal pulp should be removed with hand curettes or large burs at low speed. The hemostasis is obtained by gently applying a sterile cotton pellet moistened in saline (about 4 minutes). Pulp medication can be performed with 15.5% iron sulfate for 15 seconds, followed by washing and drying; 20% formocresol for 5 minutes is applied to fix the root pulp; MTA on the root pulp; layer of calcium hydroxide, p.a., directly on the pulp. Next, the restoration with glass ionomer or zinc oxide-eugenol cement and sealing with adhesive or metallic restoration is carried out. Some studies showed that the success rates with the use of calcium hydroxide are smaller than those of the other materials.
4. Desensibilization of the pulp for posterior pulpotomy or pulpectomy (evidence C): it is indicated in the cases of pulp with hyperalgesia and little collaborative children. The pulp should exhibit signs of vitality. The caries is removed and a cotton pellet with antibiotic solution and steroidal antiinflammatory drug (Ledermix) and IRM. After 7-14 days, the pulpotomy or pulpectomy is performed.
5. Pulpectomy (level of evidence B): it consists in the total removal of the pulp and root obturation. It is indicated in cases in which the bleeding during pulpotomy, irreversible pulpitis or pulp necrosis could not be controlled with or without associated infection, in collaborative patients. The roots should be sound or with little resorption. It can be performed in one or two stages. If there is infection and intracanal drainage with difficult drying, the two-stage technique should be preferable, with application of intracanal antibiotics during 7-10 days; the need of prescription of systemic antibiotics should be considered. Before the beginning of the pulpectomy procedure, a radiograph should be taken to verify the integrity of the roots, absolute isolation is mandatory. The coronal pulp is removed and irrigated with saline (0.9%), chlorhexidine (0.4%) or sodium hypochlorite (0.1%). Caution should be taken regarding to the sodium hydroxide irrigation towards the apex because of its irritating and cytotoxic potential. The working length is established at 2 mm short of the apex. Intraradicular cleaning is executed through files with size not greater than #30. Root washing and cleaning is carried out and the obturation is accomplished with an absorbable paste (slow-setting oxide zinc-eugenol cement, calcium hydroxide paste or iodoform paste) and definitive restoration. A success rate of 86% in 3 years is expected.
Relevant considerations
Caution in the diagnosis not to confound a pulp pain with dental papilla pain because of food impaction. This symptomatology disappears with the tooth restoration.
In case of loss of the contra-lateral primary first molar, the extraction can be indicated to prevent the midline shifting.
Some authors recommend that the initial caries removal, restoration with either glass ionomer or zinc oxide-eugenol cement and after 1-3 months the procedure is completed, especially for anxious children. The success rate of this procedure seems to be associated with a good coronal sealing. It is recommended optimum isolation with rubber dam for all treatments modalities.
Six-month following-up should be performed.
Apicification, replantation in cases of avulsion and post and core are not indicated in primary teeth.
Interproximal radiographs are normally enough to evaluate the roots of primary teeth. However, if all root extension cannot be visualized on the interproximal radiograph, a periapical radiograph should be taken.
There are no reliable evidences regarding to the superiority among pulpotomy with formocresol, pulpotomy with iron sulfate, electrosurgical pulpotomy or pulpectomy with the use of oxide zinc-eugenol cement. There is a discussion in literature on the convenience and safe of the use of products based on aldehyde in Pediatric Dentistry 4,8,9. Formocresol is not long used in Canada and Netherlands because of the safe concern. Histological assessments and in vitro studies demonstrated the toxic and mutagenic potential of formaldehyde. However, there are no reports on the adverse effects in any of the studies discussed in this review. There is no direct evidence of the adverse effects after the pulpotomy in primary tooth using formocresol. Iron sulfate can be recommended as a proper substitute of formocresol 7.
Studies have reported good success rates with the use of MTA in the pulpotomy of primary molars. Success rates of 100% (gray MTA) and 90% (white MTA) during 12-month following-up were found 1. By comparing it with formocresol, the study of Holan et al. 3 reached a success rate of 97% in the clinical and radiographic assessments in pulpotomies with MTA, while formocresol had success in 83% of the cases (although without statistical difference). In the meta-analysis review of Peng et al. 6 MTA was greater than formocresol in the pulpotomies of primary molars.
References
1. Agamy HA, Bakry NS, Mounir MM, Avery DR. Comparison of mineral trioxide aggregate and formocresol as pulp-capping agents in pulpotomized primary teeth. Pediatr Dent. 2004 Jul-Aug;26(4):302-9. [ Links ]
2. American Academy of Pediatric Dentistry. Guideline on pulp therapy for primary and immature permanent teeth [cited 2011 Sep 10]. Available from: URL:www.aapd.org/media/ policies_guidelines/g_pulp.pdf.
3. Holan G, Eidelman E, Fuks AB. Long-term evaluation of pulpotomy in primary molars using mineral trioxide aggregate or formocresol. Pediatr Dent. 2005 Mar-Apr;27(2):129-36.
4. Judd PL, Kenny DJ. Formocresol concerns. A review. Journal of the Canadian Dental Association. 1987;53:401-4.
5. Nadin G, Goel BR, Yeung CA, Glenny AM. Pulp treatment for extensive decay in primary teeth.Cochrane Database Syst Rev. 2003;(1): CD003220.
6. Peng L, Ye L, Tan H, Zhou X. Evaluation of the formocresol versus mineral trioxide aggregate primary molar pulpotomy: a meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Dec;102(6):e40-4.
7. Peng L, Ye L, Guo X, Tan H, Zhou X, Wang C et al. Evaluation of formocresol versus ferric sulphate primary molar pulpotomy: a systematic review and meta-analysis. Int Endod J. 2007 Oct;40(10):751-7.
8. Ranly DM. Formocresol toxicity: current knowledge. Acta de Odontologia Pediatrica. 1984;5:93-8.
9. Ranly D, Garcia-Godoy F. Current and potential pulp therapies for primary and young permanent teeth. Journal of Dentistry. 2000;28:153-61.
10. Rodd HD, Waterhouse PJ, Fuks AB, Fayle SA, Moffat MA. British Society of Paediatric Dentistry. Pulp therapy for primary molars. Int J Paediatr Dent. 2006 Sep;16 Suppl 1:15-23.
 Correspondence:
Correspondence:
Allan Abuabara
Rua Adalberto Schmalz, n. 402, casa 4, Condomínio Ibiza – Glória
CEP 89217-260 – Joinville – SC – Brasil
E-mail: allan.abuabara@gmail.com













