Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.10 no.1 Joinville Jan./Mar. 2013
ORIGINAL RESEARCH ARTICLE
A comprehensive method to classify subgroups of bruxers in temporomandibular disorders (TMDs) individuals: frequency, clinical and psychological implications
Omar Franklin MolinaI, II; Zeila Coelho SantosII; Bruno Ricardo Huber SimiãoII; Rógerio Ferreira MarchezanII; Natalia de Paula e SilvaII; Karla Regina GamaII
IHarvard University – USA.
IICentro Universitário UnirG – Gurupi – TO – Brasil.
ABSTRACT
Introduction: Bruxism is an oral pnenomenon described as a parafunctional activity involving nocturnal and/or diurnal tooth clenching and/or grinding which may cause teeth wearing, fatigue, pain in the muscles and temporomandibular joints and limitations in mandibular movements.
Objective: To classify bruxers in four different subgroups.
Material and methods: Evaluation of 162 individuals presenting temporomandibular disorders (TMDs) referred consecutively over a period of six years. Chief complaint, history of signs/symptoms and clinical examination were used to gather data. Individuals were classified as TMDs if they were seeking active treatment for the following complaints: pain in the masticatory muscles and/or temporomandibular joints (TMJs), difficulties to perform normal jaw movements, tenderness to palpation of muscle and joints, joint noises and. Patients were classified as mild, moderate, severe and extreme bruxers if they presented 3 to 5, 6 to 10, 11 to 15 or 16 to 25 signs and symptoms of bruxing behavior, respectively. Data was submitted to Chi-square for independence and Fisher's exact test (p < 0.05).(=30).
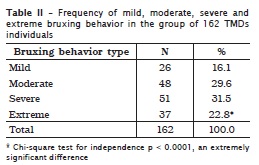
Results: Frequencies of 16.1%, 29.6%, 31.5% and 22.8% of mild, moderate, severe and extreme bruxing behavior were found in this study. Moderate and severe bruxing behavior occurred more frequently than mild and extreme bruxing behavior (p < 0.0001).
Conclusion: The four groups of bruxers occurred more or less frequently in this study and mild and extreme bruxing behavior demonstrated the lowest frequencies of such behavior.
Keywords: bruxism; extreme bruxism; temporomandibular disorders; classification.
Introduction
Reported oral jaw habits in the masticatory system include grinding and clenching the teeth, tongue, cheek and nail biting, excessive talking, smoking, jutting the jaw forward, unilateral chewing, placing objects into the mouth, gum chewing, using some musical instruments and other less known oral jaw habits 15. Bruxism is the term used with the connotation of grinding and clenching the teeth at night and/or during the day. It has been described frequently as an unconscious oral behavior 15, and a significant concomitant factor of periodontal tissue lesions 7 and severe tooth wear 20. Bruxism has also been described as a behavior characterized by involuntary jaw movements manifested as clenching and/or grinding or applying pressure on the teeth 9.
There is an accepted opinion among researchers about the importance of parafunctional habits in the etiology of TMDs (Temporomandibular disorders). Mechanisms through which an intense parafunctional activity causes some pathological effects on the temporomandibular joints (TMJs) and other anatomic structures have not been completely elucidated. It is of upmost importance to understand the etiology and the presence of diverse bruxing behavior subgroups as the behavior occurs frequently in the general population and causes mild, moderate or severe damage to the dentition and supporting structures. Even though bruxing behavior is a potential destructive oral jaw habit causing tooth wear, damage on adjacent anatomic structures, inflammation, gingival recession, muscle and joint pains, headaches and muscle stiffness in the face, head and neck, little is known about bruxism subgroups 19.
Most signs and symptoms assisting the clinician in diagnosing the behavior have been delineated in previous studies 7,19, describing more than 20 sign and symptoms concomitant of the behavior, but such investigations did not classify neither subgroups nor severities of the behavior. One study 18 reported a case of severe bruxism in a child, but researchers did not delineate the criteria for severe bruxism. One investigation 2 reported that some types of bruxism lead to the spread of inflammation to the TMJ capsular ligament and the development of fibrosis, but investigators did not describe the characteristics of such types of bruxing behavior.
Another research 16 in TMDs individuals described mild, moderate and severe subgroups of bruxers and their relationship to the severity of TMJ and muscle disorders. However, taking into account that numerous signs and symptoms of bruxing behavior do exist, it seems apparent that researchers failed to describe an extreme or severest bruxing behavior subgroup. Because there is a diversity of signs and symptoms of bruxing behavior and many of them can be used to form a scale of severity, researchers contend that subgroups of individuals presenting heavy 6, severe 16, recalcitrant and/or frequent bruxism 8, however, a comprehensive scale or degrees of severity does not exist. Thus, the goal of this study is twofold: (1) introduce a method to classify and describe four subgroups of bruxers; (2) determine the frequency of mild, moderate, severe and extreme bruxing behavior.
Material and methods
Sample selection and classification of bruxers
One hundred sixty two individuals presenting TMDs and bruxing behavior were referred consecutively over a period of 6 years to UNIRG, School of Dentistry, Division of Orofacial pain and Occlusion, for assessment and treatment. The evaluation charts of such individuals were filled in a standardized way by one researcher (OFM) specifically trained in the field of assessing TMDs and bruxer individuals. Patients were classified as presenting TMDs if they demonstrated at least three of the following signs, symptoms or behaviors 16: complaint of pain in the masticatory muscles and/or TMJs, difficulties to perform normal jaw movements, tenderness to palpation of joints/muscles, joint noises, seeking active treatment for their complaints and headaches of temporomandibular origin. The inclusion criteria for TMDs individuals were: at least two TMD signs and symptoms described previously, seeking active treatment for such disorders, and failure of previous modes of treatment. Exclusion criteria were: presence of neurologic disturbances, any disabling complaint and major psychological and/or psychiatric disorders. Inclusion criteria for bruxing behavior were the presence of at least 3 signs and/or symptoms of all those for bruxing behavior described below, to be in good health and seeking active treatment for bruxism/and or TMDs. Exclusion criteria were the presence of neurologic disorders including motor disturbances, compromised mental or physical ability, major psychiatric or psychological disorders and current use of antipsychotic medication.
Because approximately 25 signs and symptoms directly associated to bruxing behavior have been identified and in a previous study the severe group was that presenting 11 to 15 signs and symptoms 16, we reasoned that a fourth group presenting 16 or more signs and symptoms would form the severest or extreme group. We also reasoned that the rationale of this classification would be validated in future studies comparing clinical and psychological data in these four subgroups of bruxers (mild, moderate, severe and extreme). Thus, in this study, the extreme or severest bruxing behavior subgroup would be that exhibiting 16 to 25 signs or symptoms. In theory, it is believed that this group is very different from other subgroups regarding severity of muscle and TMDs, presence of psychological variables including anxiety, depression, somatization and pain in other body sites. Mild, moderate, severe and extreme bruxers were those presenting 3 to 5, 6 to 10, 11 to 15, 16 to 25 signs and symptoms, respectively. In order to discuss the clinical and psychological implications in severe and extreme bruxers, the current literature on this subject will be used. The whole list of signs and symptoms to describe severity of bruxing has been developed based on experts´ descriptions according to the literature and in a previous study on muscle and TMJ signs and symptoms in bruxers 6,8,16:
1. Patient's report of catching himself/herself clenching the teeth during the day;
2. A report of masseter muscle fatigue during the day;
3. Patient's report of masseter muscle fatigue on awakening in the morning;
4. Masseter muscle tension during the day;
5. Masseter muscle tension on awakening in the morning;
6. Patient's report of catching himself/herself grinding or clenching at night;
7. A feeling of jaw locking on awakening at night;
8. Tooth wear, specifically on the anterior and lower teeth on visual inspection;
9. Patient's report of awakening with facial, headache and or TMJ pain in the morning;
10. Patient's report of awakening in the morning with a feeling of pain/discomfort in the teeth;
11. A report of awakening in the morning with a feeling of having slept with the jaws locked, clenching;
12. Toothache on awakening in the morning, not related with caries or a dental lesion;
13. Tooth sensitivity to cold;
14. Hypertrophy of the masseter muscle;
15. Recent history of fracturing teeth and/or restorations;
16. Friends/relatives' report of clenching or grinding the teeth at night;
17. Cervical pain on awakening in the morning;
18. A feeling of body fatigue on awakening in the morning;
19. Patient's report of feeling tired or with a feeling of daytime sleepiness;
20. Presence of cheek biting;
21. Presence of tongue biting or tongue indentations;
22. Exostosis in the maxilla and or in the mandible;
23. Tori in the maxilla and or mandible;
24. Difficulties to open the mouth on awakening in the morning;
25. History of fracture, breaking or excessive damage of an occlusal splint.
Determination of the frequency of each bruxing behavior subgroup
The clinical value of this method is that by using patients' report and clinical observations (tooth wear, cheek and tongue biting, maxillary and/or mandibular tori and exostosis of the jaws), it allows the examiner to obtain data on different severities and frequencies of bruxing behavior as it would not be practical to use sophisticated methods when assessing a large sample of individuals in epidemiological studies. Moreover, the list of 25 signs and symptoms also allows the clinician or researcher to classify bruxers by the degree of severity, readily. According to one investigation 11, a gradient method (mild, moderate, severe or extreme bruxing behavior), provides an additional element which strengthens the independent variable being studied (in this case, severity of bruxism as related to clinical sign and symptoms).
Clinical and psychological implications of severe and extreme bruxism
We assumed that by using this method of self-report and clinical examination, subgroups of severe and extreme bruxers would be found in this study. Even though we used psychological tests to gather data on anxiety and depression, it was not the scope of this study to compare data about such psychological disorders in bruxers, with data from other studies. Rather, clinical and psychological data about severe, heavy, extreme, destructive bruxism from other studies will be used to discuss the frequencies of severe and extreme bruxing behavior found in this investigation. Because this study was based on a retrospective review of clinical data and individuals were not assessed purportedly for this research, but rather for the purpose of diagnosis and treatment, it was approved by the Ethical Committee in Research of the School of Dentistry under protocol number 002-2011. A statistical method deemed appropriate in this study was the Chi square test for independence and Fisher´s exact test. The level of significance was set at 0.05.
Results
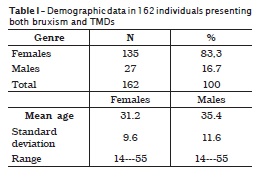
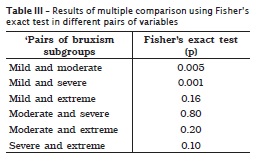
Table I shows that most patients in the group of TMDs and bruxers (N = 162) were females (n = 135 or 83.3%) and the mean age of the group was about 31.2 in females and 35.4 in males. Table II demonstrates that severe and moderate bruxism subgroups showed the highest frequencies of the behavior and mild/extreme bruxers, the lowest ones. Chi-square test for independence demonstrated that the difference in frequencies was statistically significant (p < 0.0001). Table III demonstrates that there were no statistically significant differences when comparing the frequencies of mild and extreme (p = 0.16), moderate and severe (p = 0.80), moderate and extreme (p = 0.20) and severe and extreme bruxing behavior (p = 0.10), respectively. Statistically significant differences were observed when comparing mild and moderate bruxism (p < 0.0005) and mild and severe bruxism (p < 0.001). Thus, moderate and severe bruxism occurred more frequently as compared to mild bruxism.
Discussion
One of the goals of this study was to demonstrate a clinical method to classify bruxers in four subgroups. According to data in this study and using 25 characteristics of bruxing behavior, mild, moderate, severe, and extreme bruxing behavior subgroups were observed with some frequency in this study. The results of this study are supported in part by one research 17 that reported a case of severe bruxing behavior in a child with autism. Another epidemiological investigation 16, reported the presence of mild, moderate and severe bruxing behavior subgroups, but researcher used only 15 signs and symptoms and the subgroup of extreme bruxism was not described. One investigation [6] classified bruxism in "destructive" and "non-destructive", diurnal and nocturnal, centric and eccentric, and used a clinical method to assess bruxism.
Providing additional support for the clinical significance of a classification system, one study 23 classified TMDs and non-TMDs individuals as presenting sleep, depression and destructive bruxism, but researchers used a clinical and polisomnographic method and subgroups were very small, which decreased the generalization of the results. An investigation using clinical methods and psychological tests 8, indicated that there are subgroups of bruxers presenting frequent and non frequent bruxism, those with pain in single and multiple sites and those with and without vulnerability to anxiety and psychosomatic disorders. One investigation 5 studied bruxers and myofascial pain patients and reported the presence of bruxers with and without pain.
In the current study, mild bruxism was observed less frequently as compared to moderate, severe and extreme bruxing behavior; and severe bruxism was the most prevalent behavior. It may be that because mild bruxers present with less sign and symptoms and mild or moderate pain, they were less likely to seek active treatment. One investigation 23, reported a frequency of 19.23% of destructive bruxing behavior, a prevalence which was very similar to the frequency of 22.8% of extreme bruxing behavior found in the current study. It is noteworthy to mention that in the study of Ware and Rugh 23, the samples were very small and it is very likely that the destructive group they evaluated may have been constituted by severe and extreme bruxers. Additionally, researchers used polysomnographic and clinical methods to evaluate their patients and gather data.
A previous investigation 16, reported a lower frequency of severe bruxism (16.3% as compared to 31.5% in the current study), but researchers used only 15 clinical signs and symptoms and did not assess the frequency of extreme bruxing behavior. Additional and partial support for the results of the current study comes from one investigation 4 using electromyographic and biochemical methods, reporting that TMDs individuals may present "light or heavy" nocturnal bruxism. One investigation 8 reported the presence of bruxism with muscular tension and bruxism without muscular tension with a lower level of aggression. It may be that more aggression can be found in those presenting severe and extreme bruxing behavior as bruxism has been correlated with aggression 14 and anxiety 13.
In the current study we found a frequency of 31.5% severe and 22.8% extreme or destructive bruxing behavior, respectively. Thus, the results of this study are in line with one research 23, reporting the presence of a destructive subgroup of bruxers exhibiting clinical and psychological symptoms including headaches, neckaches, backaches and depression. Researchers in that study suggested the use of splint and antidepressants to treat such patients. An antidepressant with an agonist dopaminergic profile such as bupropion may be useful for the treatment of sleep bruxism as dopaminergic deregulation is important etiologically in sleep bruxism 1. The results of the present study are also in accordance at least in part with one investigation 11, indicating that some patients grind once a month whereas others grind "every night", with up to 90% of observed sleep bruxism episodes, these subjects are classified as severe sleep bruxers.
Even though some patients with severe mechanical wear are frequently asymptomatic, report parafunctional habits and need a more simple treatment approach 22, other patients, specifically those with destructive sleep bruxism should be treated using a multidisciplinary team and many modes of therapy to improve quality of life and increase awareness of the behavior 20. Severe bruxers audibly grind their teeth, have severe tooth wear and difficulty to speak, swallow and chew 21.
The intensity of the damage on the joint and muscles in bruxers will depend on the strength of the parafunctionally used forces 12 thus, a specific protocol of treatment should be instituted for temporomandibular joints presenting with clicking, popping or crepitation as some types of bruxism lead to the spread of the inflammation to the TMJ capsule and ligaments. Some neurological disorders which occur concomitantly with severe bruxism may be treated using botulinun toxin 21. Mild bruxism seems not to be a significant clinical problem as the consistency and intensity of forces do not appear to create remarkable injury to the masticatory system 12. However, frequent bruxism can be correlated with more dysfunctional signs and symptoms adjacent and distant to the masticatory system 8.
Some sleep bruxism patients present and anxious personality, are more task oriented, focused on successful performance 19, others are vulnerable to stress, anxiety and psychosomatic disorders 8; and thus, their treatment may include the use of anti-anxiety drugs. In severe bruxers, an acrylic dental guard is usually indicated. A dental guard not only prevents tooth wear, it also really helps to reduce the number of episodes of muscular activity related to grinding of teeth 18. In other cases, a splint does not stop nocturnal bruxism 2, and thus, pharmacological and psychological methods may also be used to reduce anxiety, depression and psychological conflict.
Studies 7 have demonstrated that some many myofascial pain patients may not respond to conventional therapy and such findings reinforce the need to assess the type of bruxing behavior in such patients in order to use alternative modes of therapy. Because in some patients the level of urinary catecholamines may be high, indicating "heavy bruxism" and increased epinephrine excretion has been found to occur in states of anxiety 4, anti-anxiety drugs seems to be indicated to reduce patients' emotionally stressful states. In those cases in which severe bruxism is associated with altered sleep micro-architecture 3, Rapid Eyes Movement sleep behavioral disorders and insomnia 1, Zolpiden which selectively binds to the omega-1 GABA-benzodiazepine receptor complex, may be recommended for those more complex patients 1.
Pitfalls of the current investigation
Even though we assessed a large sample of bruxers and TMDs individuals, described an extreme group based on the number of signs and symptoms, the four subgroups could be considered "large", and we reported significant differences in the frequencies, one limitation of this study is noteworthy of mention: the four subgroups reported in this study and the frequencies of severe or extreme bruxing behavior were compared with other studies in which the samples were not sufficiently large and/or the method of assessment of severity was different.
Such differences decrease somehow the statistical value and generalization of the comparisons. However, such limitations can be avoided in future studies replicating this investigation using large samples and the same methods reported in the current research. We hope that other researches attempt to replicate these results using the same methods to increase or decrease the validity of the results presented in the current investigation.
Conclusion
Based on the results of the current study, it can be concluded that:
• The method presented and based on a questionnaire and clinical examination of sign and symptoms related to bruxing behavior proved to be useful, allowing the classification of mild, moderate, severe and extreme bruxing behavior subgroups;
• Although all subgroups of bruxing behavior were found in the current investigation, higher frequencies of moderate (29.6%) and severe bruxism (31.5%) were observed as compared to lower frequencies of mild (16.1%) and extreme bruxism (22.8%).
References
1. Alóe F, Gonçalves LR, Azevedo A, Barbosa RC. Bruxismo durante o sono. Rev Neurociênc. 2003;11:4-17. [ Links ]
2. Basić V, Mehulić K. Bruxism: an unsolved problem in dental medicine. Acta Stomat Croat. 2004;38(1):93-6. [ Links ]
3. Boutros NN, Montgomery MJ, Hatch JP. The effects of severe bruxism on sleep architecture. Clin Electroencephal. 1993;24:59-63. [ Links ]
4. Clark GT, Rugh JD, Handelman SL. Nocturnal masseter muscle activity and urinary catecholamine levels in bruxers. J Dent Res. 1980;59:1571-6. [ Links ]
5. Dao TT, Lund JP, Lavigne GJ. Comparison of pain and quality of life in bruxers and myofascial pain patients. J Orofac Pain. 1994;8:350-6. [ Links ]
6. Dupont JS, Brown C. Management of nocturnal bruxism with an anterior stop point appliance. J Tennessee Dent Assoc. 2011;88:20-5. [ Links ]
7. Guarda-Nardini L, Manfredini D, Salamone M, Salmaso L, Tonello S, Ferronato G. Efficacy of botulinum toxin in treating myofascial pain in bruxers: a controlled placebo pilot study. J Craniomand Pract. 2008;26:1-9. [ Links ]
8.Kampe T, Edman G, Bader G, Tagdae T, Karlsson S. Personality traits in a group of long-standing bruxing behavior patients. J Oral Rehab. 1997;24:688-93. [ Links ]
9. Lavigne GJ, Goulet JP, Zuconni M, Morrison F, Lobbezoo F. Sleep disorders and the dental patient. Oral Surg Oral Med Oral Pathol Oral Med Oral Radiol Endod. 1999;88:257-72. [ Links ]
10. Lavigne GJ, Kato T, Kolta A, Sessle BJ. Neurobiological mechanisms involved in sleep bruxism. Crit Rev Oral Biol Med. 2003;14:30-46. [ Links ]
11. Lobbezoo F, Lavigne JG. Do bruxism and temporomandibular disorders have a cause-effect relationship? J Orofac Pain. 1997;11:15-23. [ Links ]
12. Mehta NR, Forgione AG, Maloney G, Greene R. Different effects of nocturnal parafunction on the masticatory system: The weak link theory. J Craniomand Pract. 2000;18(4):280-5. [ Links ]
13. Molina OF, Peixoto MG, Tavares PG, Dib JE, Aquilino RN. Anxiety in craniomandibular disorders and bruxing behavior patients. Part I: Inclusion of the extreme bruxing behavior group and report of psychological preliminary data on anxiety. Rev Neurociênc. 2006;14:23-30. [ Links ]
14. Molina OF, Peixoto MG, Coelho ZC, Penoni JD, Aquilino RN, Peixoto MAS. Bruxism as a mechanism subserving hysteria: a new theory. Rev Neurociên. 2008;16(4):259-68. [ Links ]
15. Molina OF, dos Santos J, Nelson SJ, Nowlin T, Mazzeto M, Mainieri ET. Oral jaw behaviors in TMDs and bruxism: a comparison study by the severity of bruxism. J Craniomand Pract. 2001;19:114-21. [ Links ]
16. Molina OF, dos Santos J, Nelson SJ, Nowlin T. A clinical study of signs and symptoms of CMDs in bruxers classified by the degree of severity. J Craniomand Pract. 1999;17:268-79. [ Links ]
17. Mutlu MS, Prathibha KM. Management of a child with autism and severe bruxism: a case report. J Indian Soc Pedod Prevent Dent. 2008 Jun:82-4. [ Links ]
18. Petit D, Montplaisir J. Early childhood parasomnias. Encyclopedia on early child development. 2010 May:1-7. [ Links ]
19. Pingitore G, Chroback V, Petrie J. The social and psychologic factors in bruxism. J Prost Dent. 1991;65:443-6. [ Links ]
20. Rouse JS. The bruxism triad. Inside Dentistry. 2010 May:32-44. [ Links ]
21. Tan EK, Jankovic J. Treating severe bruxism with botulinum toxin. JADA. 2000;131:211-6. [ Links ]
22. Verrett RG. Analyzing the etiology of an extremely worn dentition. Journal of Prosthodontics. 2001;10:224-33. [ Links ]
23. Ware JC, Rugh JD. Destructive bruxism: sleep stage relationships. Sleep. 1988;11:172-81. [ Links ]
 Corresponding author:
Corresponding author:
Omar Franklin Molina
Centro Universitário UnirG – Faculdade de Odontologia
Av. Pará, n. 1.544
CEP 77400-020 – Gurupi – TO – Brasil
E-mail: Ofrank.nyork.harvard.texas@hotmail.com
Received for publication: August 19, 2011
Accepted for publication: August 21, 2012













