Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.10 no.1 Joinville Jan./Mar. 2013
ORIGINAL RESEARCH ARTICLE
Cytological changes in oral epithelium due to Sudanese homemade alcoholic beverages
Hussain Gadelkarim AhmedI; Shima Bushra BakhetI; Awdah M. Al-hazimiII
IDepartment of Histopathology and Cytopathology, FMLS, University of Khartoum – Khartoum – Sudan.
IICollege of Medicine, University of Hail, KSA.
ABSTRACT
Introduction and Objective : The aim of this study was to assess the cytological changes in oral epithelium that might be induced by Sudanese homemade alcoholic beverages.
Material and methods: Oral Exfoliative Cytology (OEFC) was applied to a case control study to assess the presence and severity of oral epithelial atypia (ET) in 300 subjects (150 alcohol abuse individuals (cases); 150 non-alcohol abuse individuals (controls)). All cases were using homemade alcoholic drinks, locally known as, Aragee, Marisa and others. Five patients with oral squamous cell carcinoma (OSCCs) were included as internal controls.
Results: ET was detected in 7 subjects and was not observed in the remaining 293. All the 7 subjects with cytological atypia were cases. Cytological atypia were identified among those using Aragee, Marisa, and Aragee & Marisa together, representing 53%, 28.6%, 18%.4, respectively. Cytological atypia was found in all the 5 control cases with OSCCs. For the cytological atypia among alcohol abuse individuals, the adjusted OR and the 95% CI were found to be 5 (4.34-5.84) and P = 0.008. Inflammatory cells infiltrates were identified among 21 (14%) of the cases and only 12 (8%) of the controls and the adjusted OR and the 95% CI were found to be 5 (2.51-11.21) and P = 0.009.
Conclusion: In view of these findings, Sudanese homemade alcoholic beverages cause oral epithelial atypical changes, which lead to oral precancerous and cancerous lesions. OEFC is a useful procedure for detection and assessment of oral ET.
Keywords: epithelial atypia; homemade alcoholic beverages; Sudan.
Introduction
The prevalence of oral cancer is particularly high among men, the eighth most common cancer worldwide. Incidence rates for oral cancer vary in men from 1 to 10 cases per 100,000 population in many countries 19.
The primary risk factors for development of either OSCCs or Oral Potentially malignant Disorders (OPMD) are considered to be similar 13,8. The cancer epidemic in developed countries, and increasingly in developing countries, is due to the combined effect of the ageing of populations, and the high or increasing levels of prevalence of cancer risk factors. It has been estimated that 43% of cancer deaths worldwide are due to tobacco, unhealthy diet, physical inactivity and infections 18. Tobacco use and excessive alcohol consumption have been estimated to account for about 90% of cancers in the oral cavity. The oral cancer risk increases when tobacco is used in combination with alcohol 16.
In the Sudan, the high incidence of OSCCs and an equally high prevalence of potentially malignant oral mucosal lesions has been strongly attributed some local habits such as snuff use, locally known as Toombak 4. A close relationship between use of toombak and development of OSCCs has been reported 9. Additionally, use of toombak has been shown to produce a variety of oral mucosal changes such as dysplasia and hyperkeratosis 9-11.
In the Sudan, the high prevalence of homemade alcoholic varieties use might be associated with high risk for development of OSCCs and a variety of oral mucosal changes. Nevertheless, most consumers believe that homemade alcoholic varieties are safe and consequently consume huge quantities, and some of them regard it as medication for certain disease such as hypertension and fever. For some tribes, particularly, in Southern and Western Sudan, people considered these varieties particularly Marisa, as a nutritional source in daily basis life. This in addition to the fact that most people attribute the high incidence of oral cancer to the use of toombak ignoring other risk factors. Therefore, the aim of this study was to identify the effects of homemade alcoholic varieties on oral mucosal epithelium that might eventually terminate in OPMD or OSCC.
The most popular alcoholic beverages in Sudan include, Aragee, Marisa, Assalia, Kanin, Knogouoro, others. All these beverages have different preparation methods and alcoholic (ethanol) content. Aragee is a sprit distilled alcoholic beverage that have the highest alcohol content, produced by the distillation of fermented dates. Marisa is a wine containing less alcoholic content than Aragee, produced by fermented maize or fume. Kanin is relatively similar to Marisa but with additional nutritional components, such as, sesame. Assalia is prepared as the same as Marisa, but with very low alcohic content, because it is fermented for a very short period. Knogouoro is a form of Marisa with more additives such as sesame, sweets (Tahania). Although, these are the main alcoholic beverages commonly used in Sudan, there are other minor varieties such as Shurboats and others. However, drink of alcoholic beverages is prohibited in Sudan.
Material and methods
A total of 300 apparently healthy volunteers living in the city of Khartoum have participated in this study, among whom 150 homemade alcoholic beverages abuse individuals (ascertained as cases) and 150 non-alcohol users selected from general population. All cases were accessed in prisons and controls were accessed from people living in the city of Khartoum. Cases and controls were matched for socio-economic status and Body Mass Index (BMI). Smokers and Toombak users were excluded from both cases and controls. Internal positive controls were obtained from five patients with histologically confirmed OSCCs. Internal controls were accessed from Khartoum Dental Teaching Hospital.
Cytological smears of exfoliated cells were collected from buccal mucosa of cases and controls. The material was collected by a smooth brushing of the cheek mucosa, border of the tongue, and floor of the mouth. Regardless of the gender, the study subjects were 18 years of age or older and non-tobacco users. Information of the subject's personal characteristics and alcoholic habits were obtained. Each case was found to use one or more of these homemade alcoholic varieties (Aragee, Marisa, Assalia, Kanin, Knogouoro, others).
Using a flat wooden tongue spatula, cytological smears were collected from all the study subjects. The surface epithelium was scraped and cells were collected, immediately smeared on a cleaned coated glass slide, fixed in 95% ethanol for 15 min and then transferred to the laboratory at the Faculty of Medical Laboratory Science, University of Khartoum.
The smears were stained using the Papanicolaou staining method. Ethyl alcohol fixed smears were hydrated in descending concentrations of 95% alcohol through 70% alcohol to distilled water, for two minutes in each stage. Then the smears were treated with Harris' hematoxylin for five minutes to stain the nuclei, rinsed in distilled water and differentiated in 0.5% aqueous Hydrochloric Acid for a few seconds, to remove the excess stain. They were then immediately rinsed in distilled water, to stop the action of discoloration. Then the smears were blued in alkaline water for a few seconds and dehydrated in ascending alcoholic concentrations from 70%, through two changes of 95% alcohol for two minutes for each change. The smears were next treated with Eosin Azure 50 for four minutes. For cytoplasmic staining, they were treated with Papanicolaou Orange G6 for two minutes, rinsed in 95% alcohol and then dehydrated in absolute alcohol. The smears were then cleared in Xylene and mounted in DPX (Distrene Polystyrene Xylene) mount. All the reagents used were from Thermo Electron Corporation, UK.
Assessment of the results
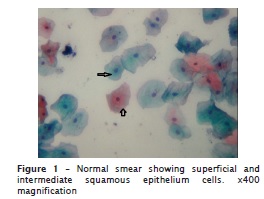
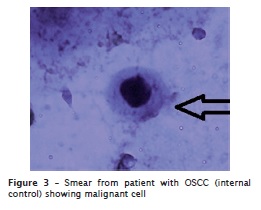
To assess the quality of staining, smears were examined under (x10 magnification) power light microscope. All smears showed fair staining quality with blue nuclei, pink/orange cytoplasm of the keratinizing squamous cells and blue/green staining of the cytoplasm of the non-keratinizing squamous epithelial cells. To increase the reliability and reproducibility, strict quality control measures were applied. We included 5 smears from patients with histopathologically diagnosed OSCCs as Internal positive controls. Cytological smears were labeled in such a way that the examiner was blind to the alcohol habit of each subject. All smears were examined by two independent examiners.
Assessment of the epithelial atypia
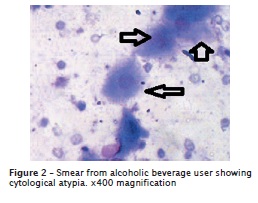
The presence of two or more of the following features were consistent with atypia: nuclear enlargement associated with increase nuclear cytoplasmic ratio, hyperchromatism, chromatin clumping with moderately prominent nucleoli, irregular nuclear membranes and bi or multinucleation, scant cytoplasm, and variation in size and/or shape of the cells and nuclei.
Statistical analysis
Data management was done using Statistical Package for Social Sciences (SPSS version 12). SPSS was used for analysis and to perform Pearson Chi-square test for statistical significance (P value < 0.05). The 95% confidence level and confidence intervals were used.
Ethical consent
The study was approved by Faculty Research board, FMLS, University of Khartoum. All study subjects consented to participation by completing the self-administered questionnaire.
Results
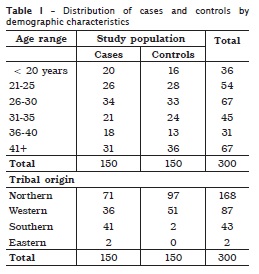
Description of the cases and the controls by demographic characteristics is shown in table I. The age distribution is similar among the cases and the controls. The mean age of the study population was 32±11 years with a range from 18 to 62 years. The great majority of cases and controls were from the Northern followed by Western and Southern Sudan representing, 168, 87, and 43, respectively.
Concerning to the type of alcoholic drink, most of the cases were found to use Aragee constituting 50 (33.3%) followed by a combination of Aragee & Marisa and Marisa, representing 49 (32.64%), 42 (28%) respectively.
Figures 1 and 2 shows, respectively, a normal smear with superficial and intermediate squamous epithelium cells, and a smear from an alcoholic beverage user, indicating cytological atypia. Epithelial cytological atypia was observed among 7 of the cases and could not be ascertained among the remaining 143. All of the cytological atypias were demonstrated with mild degree (mild dyskaryosis). None of the 150 controls showed cytological atypia. The risk of cytological atypia associated with use of alcohol drink with 95% confidence interval was found to be statistically significant p < 0.008. Cytological atypia were identified among those using Aragee, Marisa, and Aragee & Marisa together, representing 53%, 28.6%, 18.4%, respectively. Cytological atypia was found in all the 5 internal control cases with OSCC (figure 3). Inflammatory infiltrates was observed among 21 (14%) of the cases and only 12 (8%) of the controls. Although, the risk of inflammatory cells infiltrate associated with alcoholic drink was found to be statistically insignificant, but it was relatively higher p < 0.09.
Discussion
Oral cancer is one of the major health problems in the Sudan, particularly among men 5. Many risk factors have been proposed to be the etiological factors including, tobacco use (particularly, Toombak) 2,4 and Human Papilloma Virus 1. In this study, the presence of epithelial atypia was quantified by cytology in smears obtained from homemade alcoholic drinks users and non-users. This is the first report from the Sudan to use cytological methods for demonstration of epithelial atypia in smears obtained from Sudanese homemade alcoholic drinks.
Exfoliative cytology has been somewhat discredited over recent years for diagnosis – even of risk for, let alone diagnosis of (OPMD). Putting considerable effort into the technique now is questionable. Exfoliative cytology remains a standard tool worldwide for screening programmes for cancer of the uterine cervix. Here, technological advances, especially various degrees of automated image analysis, have advanced the reliability and utility of the method. Unless this approach were also to be applied to the oral specimens, such as here, it is doubtful if work such as this will advance screening programmes for oral cancer and potentially malignant disorders. There is a fundamental difference between oral and uterine cervix mucosae: the former is para- or ortho-keratinised over large areas, so obtaining consistent cells from lower layers of the epithelium where the stigmata of neoplastic transformation reside, is questionable. That said there have been a number of commercial attempts to automate oral exfoliative cytology over recent years: these have not found widespread take-up, because field studies on their utility are lacking.
We found epithelial atypia in cytological smears from 7 subjects; all of them were alcoholic consumers. These findings suggest that Sudanese homemade alcoholic drinks are associated with a risk for occurrence of oral epithelial atypia, which can be detected by use of simple cytological methods.
The association between alcohol-containing mouth exposure and the development of oral cancer has been a periodic topic of scientific study for many years. Because heavy alcohol consumption is a known risk factor for the development of oral cancer, researchers looked into the possibility that use of alcohol-containing mouth exposure may also put people at risk.
The International Agency for Research on Cancer, an extension of the World Health Organization, now identifies the consumption of ethanol in alcoholic beverages as a carcinogenic risk. Alcohol abuse is associated with cancers of the mouth, pharynx, larynx and esophagus 12. The reason for this association is not fully understood, it may be due to a direct effect of alcohol on these tissue14. However, researchers have also speculated that the alcohol metabolite, acetaldehyde, and alcohol's ability to enhance mucosal penetration of other carcinogenic chemicals may be involved 12. Alcohol abuse and smoking seems to dramatically increase an individual's risk for developing oral cancer. Populations deficient in aldehyde dehydrogenase, the enzyme that clears acetaldehyde from the body, are also at greater risk for developing oral cancer associated with heavy alcohol ingestion17.
However, several studies have reported a relationship between drinking and the risk of both oral cancer and pre-cancerous and a disposition toward it 3,6,15. Although, the present data do not provide evidence that the duration of alcohol intake is an important factor in the development of cytological atypia, it was previously reported that increasing alcohol consumption over a longer period was associated with an increased risk of oral cancer 15. The presence of features of oral epithelia atypia supports the fact that exposure to alcohol affects the pattern of maturation in oral mucosal cells 7. However, the current findings suggest further assessment of the duration of drinking and dose consumption.
Since we have collected the specimens from those arrested due to drink (use of such drinks is illegal in Northern Sudan), the great majority of cases have claimed short durations of drink (>5 years). Consequently, we got no clear association between duration of these drinks and cytological atypia. Alcoholic content within these drinks is also unknown, since it differs in one drink type to another due to different producers and different manufacture procedures. Moreover, no study has measured the mean or limits of alcohol content within these drinks. Another problem is the consumption of huge quantities of these drinks which may give the possibility of increased exposure even if it is low in certain variety. One of the limitations in this study, we were unable to measure ethanol content within these drinks, as well as, un-affordability of getting individuals with prolonged period of use.
Study design has been the major obstacle to reaching conclusions about the relationship between alcohol-containing drinks and oral cancer based on the information about alcohol content within these drinks, as well as, consideration of other related factors. This could be overcome with well-designed prospective studies that document the type of alcoholic drink used, the onset, duration and frequency of drink use, and the presence of other oral cancer risk factors.
In the present study, inflammatory cells infiltrates were more frequently observed among cases than controls. Inflammatory cells infiltrate was identified in 14% of the cases compared with 8% of the controls. We think that this variation evidenced the irritation role of alcohol to stimulate the inflammatory changes. Although, the presence of bacteria in the smears does not make a diagnosis of infection and in regard to the cytological evidences of bacterial changes, the oral cavity is a traditional site for many commensal bacteria. Although the variation between cases and controls, in this respect is mild, we think that the aggregation of bacteria was due to the presence of the dead post irritated epithelial cells, which might stimulate inflammatory cells infiltrate.
Conclusion
The findings of this study indicate that Sudanese homemade alcoholic drinks use might be considered as a risk factor in the occurrence of features of cytological atypia in the buccal mucosa, which are frequently seen in premalignant and malignant oral lesions. Oral exfoliative cytology can be used for the detection of cytological atypia that is associated with oral precancerous and cancerous lesions. Duration of exposure to alcohol requires further assessment, as the majority of cases in this study were shorter duration users. Oral exfoliative cytology might be appropriate within an oral screening program, particularly for high-risk/high-prevalence communities, and users of these beverages.
Acknowledgements
We would like to thank Dr. Abdelmuhsin Omer Ahmed Hassan, at the Department of Internal Medicine, College of Medicine, and University of Hail for help and assistant.
References
1. Ahmed HG, Eltoom FM. Detection of human papilloma virus types 16 and 18 among Sudanese patients with oral squamous cell carcinoma. The Open Cancer Journal. 2010;3:1-5. [ Links ]
2. Ahmed HG, Babiker AA. Assessment of cytological atypia, AgNOR and nuclear area in epithelial cells of normal oral mucosa exposed to toombak and smoking. Rare Tumors. 2009;1(18):28-30. [ Links ]
3. Ahmed HG, Ebnoof SO, Hussein MO, Gbreel AY. Oral epithelial atypical changes in apparently healthy oral mucosa exposed to smoking, alcohol, peppers and hot meals using the AgNOR and Papaniclaou staining techniques. Diagn Cytopathol. 2010 Jul;38(7):489-95. [ Links ]
4. Ahmed HG, Idris AM, Ibrahim SO. Study of oral epithelial atypia among Sudanese tobacco users by exfoliative cytology. Anticancer Res. 2003;23(2C):1943-9. [ Links ]
5. Ahmed HG, Mahgoob RM. Impact of toombak dipping in the etiology of oral cancer. Sudan J Cancer Res Therap. 2007;3(2):127-30. [ Links ]
6. Blot WM, Laughlin JK, WinnMc DM. Smoking and drinking in relation to oral and cancer. Cancer Res. 1988;48:3282-7. [ Links ]
7. Burzlaff JB, Bohrer RL, Paiva F, Visioli F, Sant'Ana Filho M, da Silva VD et al. Exposure to alcohol or tobacco affects the pattern of maturation in oral mucosal cells: a cytohistological study. Cytopathology. 2007;18(6):367-75. [ Links ]
8. Franceschi S, Bidoli E, Herrero R, Munoz N. Comparison of cancers of the oral cavity and pharynx worldwide: etiological clues. Eur J Cancer (Oral Oncol). 2000;36B:106-15. [ Links ]
9. Idris AM, Ahmed HM, Mukhtar BI, Gadir AF, El-beshir EL. Descriptive epidemiology of oral neoplasms in the Sudan 1970-1985, and the role of toombak. Int J Cancer. 1995;61:155-8. [ Links ]
10. Idris AM, Ibrahim YE, Warnakulasuriya KAAS, Cooper DJ, Johnson NW, Nilsen R. Toombak use and cigarette smoking in the Sudan: estimates of prevalence in the nile state. Prev Med. 1998;27:597-603. [ Links ]
11. Idris AM, Warnakulasuriya KAAS, Ibrahim YE, Nilsen R, Cooper D, Johnson NW. Toombak-associated oral mucosal lesions in Sudanese show a low prevalence of epithelial dysplasia. J Oral Pathol Med. 1996;25:239-44. [ Links ]
12. International Agency for Research on Cancer. IARC monographs on the evaluation of carcinogenic risks to humans. Alcoholic beverage consumption and ethyl carbamate (urethane). Lyon; 2007. [ Links ]
13. Johnson NW, Ranasinghe AW, Warnakulasuriya KAAS. Potentially malignant lesions and conditions of the mouth and oropharynx: natural history-cellular and molecular markers of risk. Eur J Cancer Prev. 1993;2(2):31-51. [ Links ]
14. Lachenmeier DW. Safety evaluation of topical applications of ethanol on the skin and inside the oral cavity. J Occup Med Toxicol. 2008;3:26. [ Links ]
15. Morse DE, Katz RV, Pendrys DG, Holford TR, Krutchkoff DJ, Eisenberg E et al. Smoking and drinking in relation to oral epithelial dysplasia. Cancer Epidemiol Biomarkers Prev. 1996;5:769-77. [ Links ]
16. Reibel J. Tobacco and oral diseases: an update on the evidence, with recommendations. Med Princ Pract. 2003;12:22-32. [ Links ]
17. Salaspuro, M. Acetaldehyde as a common denominator and cumulative carcinogen in digestive tract cancers. Scandinavian Journal of Gastroenterology. 2009;44(8):912-25. [ Links ]
18. Stewart BW, Kleihues P (Eds.). World Cancer Report. Lyon: WHO International Agency for Research on Cancer; 2003. Available from: URL:http://www.iarc.fr/en/publications/pdfs-online/wcr/2003/index.php. [ Links ]
19. WHO. Strengthening the prevention of oral cancer: the WHO perspective. Community Dent Oral Epidemiol. 2005;33:397-9. [ Links ]
 Corresponding author:
Corresponding author:
Hussain Gadelkarim Ahmed
University of Khartoum, 102 – Faculty of Medical Laboratory Sciences
Khartoum, Sudan
E-mail: hussaingad1972@yahoo.com
Received for publication: June 4, 2012
Accepted for publication: October 1, 2012













