Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.10 no.2 Joinville Abr./Jun. 2013
ORIGINAL RESEARCH ARTICLE
Endodontic treatment for necrotic immature permanent teeth using MTA and calcium hydroxide. A retrospective study
Claudio Maniglia-FerreiraI; Fabio de Almeida GomesI; Nadine Luísa Soares de Lima GuimarãesII; Marcelo de Moraes VitorianoII; Tatyana Albuquerque XimenesII; Bruno Carvalho de SousaIII; Roberto Alves dos SantosIV
I Department of Endodontics, University of Fortaleza – Fortaleza – CE – Brazil.
II School of Dentistry, University of Fortaleza – Fortaleza – CE – Brazil.
III Department of Endodontics, Federal University of Ceará – Fortaleza – CE – Brazil.
IV Department of Endodontics, University of Pernambuco – Recife – PE – Brazil.
ABSTRACT
Introduction: Endodontic treatment of young permanent teeth with incomplete root formation and necrotic pulp has been a challenge for the dentist. It is necessary to induce the formation of apical barrier (apical plug), enabling the complete root canal filling.
Objective: This retrospective clinical study compared the protocols for treatment of teeth with incomplete root formation, using calcium hydroxide (CH) or mineral trioxide aggregate (MTA).
Material and methods: 28 patients with incomplete root formation have undergone root canal treatments in the period from 2000 to 2009 were selected. The procedures for cleaning, shaping and intracanal medication (CH paste) were performed in a standardized manner. In 13 patients, after using the CH paste (14 days), apical plugs with MTA were made. In the remaining 15 teeth monthly exchanges with CH paste were executed until it was observed radiographically the formation of the apical barrier. In all cases the canals were filled conventionally with gutta-percha and sealer. Initially, follow-ups were made on a quarterly and semiannually at the end of first year.
Results: All apical lesions showed apical healing between 4 and 13 months after starting treatment. There was not noted the continuing process of root formation.
Conclusion: It was concluded that the treatment of teeth with incomplete root formation and necrotic pulp with the use of MTA as apical plug has the same clinical results compared with the use of CH, with the advantage of less clinical time.
Keywords: incomplete root formation; apical plug; MTA; calcium hydroxide.
Introduction
Tooth trauma is the most frequent cause of pulpal necrosis in teeth with incomplete root formation and it requires an endodontic treatment1, 10. The strategies of treatment for young adults with immature dentition are important for the long-term prognosis of these teeth and they must aim to the integrity of the periapical tissues, and if possible, the vitality of the pulpal remnant, to assure the maturation and development of the roots of the teeth22.
However, the rupture of the vascular-nervous bundle may occur definitively, resulting in pulpal necrosis and the paralyzation of the stimulus responsible for the induction of the root formation13, 15. Apexification refers to a process of induction of the calcified barrier in teeth with pulpal necrosis in which there was not the completion of the root apex1. Currently, there are studies showing another treatment approach which would be based in revascularization. When the apexification was executed and compared with calcium hydroxide (CH) and mineral trioxide aggregate (MTA), it exhibited a significantly longer increasing in the root lenght in addition to the survival rate of the teeth closer to 100%12.
The use of CH as intracanal pulpal medication to induce the formation of a barrier of hard apical tissue has been reported and successfully applied since the 1960s4,9. This induction occurs due to its high pH, which after causing a superficial contact necrosis with the periapical tissue guides the deposition of hard tissue on the area20, by forming a barrier of an osteoid or cementoid material firmly adhered to the cementum and dentine11. Several clinical studies demonstrated that this treatment approach is efficient for the treatment of immature permanent teeth with pulpal necrosis and apical lesion3, 4, 9, 15, 19; however, this requires a longer treatment time15.
The MTA is a powder composed of thin hydrophilic particles that agglutinates in the presence of humidity, forming a colloidal gel and setting11, with a pH of 12.5, low compressive strength, low solubility, and greater radiopacity than dentine7, 18. It has been successfully employed as both apical plug in teeth presenting incomplete root formation and direct pulpal dressing in pulpotomies because similarly to CH, it induces the apical closing without promoting an inflammatory reaction16, 22, in addition to enable the immediate procedure of root canal2,11.
The aim of this study was to compare the treatment protocols (CH or MTA) of teeth with incomplete root formation and apical lesion visible radiographically. The following factors were taken into consideration: etiology of the pulpal necrosis, age, gender, size of the periapical lesion, symptomatology between appointments, and total time required for the complete closing of the apexes.
Material and methods
This study was approved by the Ethical Committee in Research of the University of Fortaleza, under protocol number 10-290.
Selection of the patients
Thirty-two patients, both genders, were identified and selected in the Dentistry course of the University of Fortaleza with need of endodontic treatment of the anterior teeth with incomplete root formation, pulpal necrosis and apical lesion, in the period between 2000 and 2010. Of 32 patients, it was possible to contact and follow-up 28 patients. The data regarding to the endodontic treatments were extracted from the individual files of the patients. In 13 patients, after the use of the CH paste for 14 days, MTA plugs were executed. In the other 15 teeth, the apexification was carried out every month with CH paste.
The diagnosis of pulpal necrosis was determined through the dental history, clinical examination, pulpal sensitivity, in addition to the periapical radiographs from which it was seen the presence of apical lesion, an essential fact for the precise diagnosis several times associated with the darkening of the crown13.
Treatment methods
As apexification techniques, the pulpal chamber was accessed and a conservative biomechanical preparation was executed by respecting the thin walls of the root canals and 1 mm short of the radiographic apex, with the aid of standardized hand instruments. The irrigation was carried out with biocompatible solutions (saline and chlorhexidine), followed by the intracanal medication with CH paste associated with a viscous vehicle filling all pulp cavity.
After the initial appointment, the treatment protocols were different, as follows:
• Protocol 1 – Execution of monthly changes of intracanal medication aiming to renew the stimulus for the formation of the hard tissue. After the radiographic proof of the complete repair of the apical lesion and formation of the apical barrier of hard tissue, the filling procedures were executed;
• Protocol 2 – It comprises the construction of an apical plug with MTA after intracanal medication with CH for 14 days, and next, the filling procedures were executed and ended normally at the second appointment or at the moment in which the clinical normality was reached (lack of signs and symptoms contraindicating it).
Success was considered when the clinical normality and radiographic (partial or total) repair of the apical lesion. Based on the history and previous radiographic images, data were gathered and analyzed regarding to the clinical variables: (i) etiology of the pulpal necrosis, (ii) age, (iii) gender, (iv) initial size of the periapical lesion (longer axis in mm), (v) symptomatology between the appointments and (vi) total time for the complete closing of the apex.
Statistical analysis of the results
All results obtained were tabulated and statistically analyzed through BioEstat version 5.0 software (Instituto de Desenvolvimento Sustentável Mamirauá, Tefé, AM, Brazil) for Windows, by using ANOVA and t tests, with level of significance of p ≤ 0.05.
Results
Twenty-eight patients were analyzed, resulting in 11 central incisors and 17 lateral incisors. The group of patients was composed by 24 male subjects and four female subjects. It is highlighted that the gender did not influence on the clinical variables studied. Tooth trauma accounts for pulpal necrosis in all the cases studied. All teeth showed periapical lesions visible radiographically; seven patients reported clinical symptomatology (pain and swelling) between the appointments and for that reason, there was an extra urgency appointment. There was no need of retreatment or surgical interventional in none of the cases studied. Table I showed the mean of the following variables: age (years), size of the periapical lesion l (mm) and time (months) of the apical closing of all the cases analyzed, according with the different treatment protocols.
Table II compares the values of three variables studied between the cases with or without clinical symptomatology between the appointments. Differences were not noted between the protocols studied regarding to the time required for the apexification process and the sizes of the lesions (p = 0.1582). Regardless of the protocol studied, the presence of the symptomatology between the appointments indicated a longer time for the formation of the apical barrier (p = 0.0003).
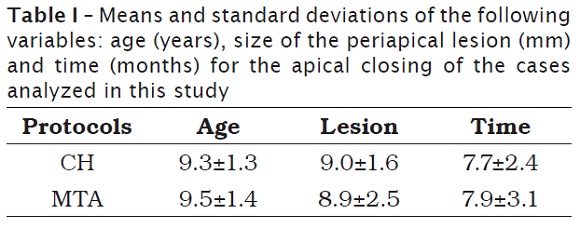
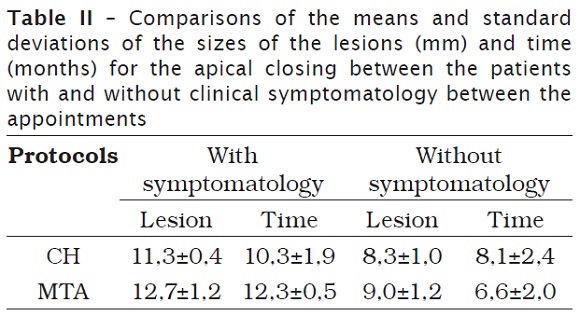
Table II demonstrated that although there were not statistically significant differences between the protocols (p = 0.1582), the apical barrier was obtained faster with MTA in the cases of teeth without symptomatology and with CH in the cases with symptomatology.
The symptomatology between appointments was noted only in teeth showing apical lesions with diameters greater than 11 mm. The age and the gender of the patients did not influence on the results. It is worth noting that the difficulty of scheduling and the failures in the radiographic documentation during the execution of the treatments were problems seen during the analysis of the files. There was only clinical failure in one case because of the relapse of trauma and occurrence of root fracture.
Discussion
The evaluation performed in this present study is in agreement with other studies1, 13, 15, in which the maxillary anterior teeth of male young adults have been most common involved in traumas, with more than 85%.
Apexification was defined as the development of an apical barrier of hard tissue which enables the ending of the endodontic treatment without requiring the surgical intervention1, 14. In teeth with incomplete or open apexes, the biological sealing occurs through the deposition of a mineralized tissue similar to cementum varying in structure and thickness10, 11, 20. The occurrence or not of this process of induced formation of the root apex depends sensibly on the operative technique, the degree of root formation already present and the intensity of the infectious process installed5, 14, 17, 19.
The treatment protocols of teeth with incomplete root formation is based on the execution of maneuvers aiming to the induction of the biological sealing22 through the use of substances of high pH, such as CH19 and currently, MTA7, 11.
The impossibility of obturation of the teeth with incomplete root formation guides the necessity of stimulating the continuation of the root development, filling the root canal temporal with medicaments9, 10, 15, 19-21 or Portland cement7, 18, to obtain the anatomical conditions that allows to perform the adequate filling, definitively8.
The results of this present study demonstrated a high rate of success with the treatment of teeth with incomplete root formation, regardless of the protocol used, which has been demonstrated by the literature10,19. However, caution should be taken in affirming that the clinical success of these cases when the adequate protocol is employed is of 100%, because the greatest etiologic agent of pulpal necrosis is tooth trauma, which also causes vertical and horizontal root fractures. This can hinder the clinical success and in several times they are not detectable. Thus, some cases can result in tooth extraction. This fact was verified in one of the cases of this study treated with CH. In this study, clinical success was considered as the total or partial radiographic repair of the apical lesion had been achieved. Notwithstanding, the tooth must be restored, in function and with no painful symptomatology or presence of fistula. Otherwise, the tooth was considered as failure16. The option for the apexification technique with changing of CH paste is a treatment that lasts for months, until the verification of the apical formation of hard tissue closing the root apex19, consequently the tooth is more vulnerable to coronal infiltration and fractures. The use of MTA as apical plug enabled the earlier obturation and restoration of the tooth8 and with high success rate6, 7, 13.
Because of the anatomic features of the teeth with incomplete root formation, the removal of both the necrotic tissues and local infection is more difficult with the use of the instrumentation, which should be executed the most conservative as possible because of the fragility of the root walls, making difficult the removal of the stimulus causing the inflammatory reaction4. This fact justifies the use of the intracanal medication for a period from seven to 15 days, aiming to stabilize the apical tissues (inflammatory process) and help the fight for the remnant infection3,8.
Some studies found a correlation between the size of the apical lesion with the presence of clinical symptomatology between the appointments9,15 and that the occurrence of flare-up between the appointments causes an increase of five months in the time required for the apical closing15,23. The results of the present study demonstrated the occurrence of symptomatology in 25% of the patients studied, corroborating the findings of the literature, in addition to take a longer time for the repair.
CH was used as intracanal medication based on the features of the substances used in Endodontics14. Several formulations containing CH have been already tested and there is no evidence of advantages of one formulation over another1,21. It is known that the association of CH with antiseptic chemical agents, such as chlorhexidine, increases the antibacterial action of the medication even more23.
The amount of time for the CH medication changing is variable: after six months14, when there is the presence of clinical symptoms1, when the decreasing of the paste is radiographically noted5 or when there is only the formation of the apical barrier19. However, all reach the clinical success and agree with the fact that the CH must be filling temporal the root canal for a period not shorter than 14 days.
In the teeth in which CH was used, the protocol of changing was at every month aiming to renew the stimulus in the periapical tissues22. In this group, after a mean period of eight months, the apical barrier of hard tissue started to be radiographically visualized and/or clinically verified with the aid of paper points during the root canal drying.
The difference between the size of the lesion and the time required for the apical closing seems to be logical because the cases exhibiting the largest lesions showed the greatest amount of tissue to be reorganized until the deposition of mineralized tissue on the root apex. Caution was taken not to misdiagnosis pathological radiolucent areas with radiolucent areas related to the incomplete root formation Evaluation of the surrounding and contralateral teeth were carried out to avoid this type of error23.
It was not necessary the complete regeneration of the periapical lesion to result in apexification, regardless of the type of protocol used. In many cases, the apexification occurred prior to the bone regeneration. Some very extensive radiolucent areas can take longer periods to regenerate completely.
Differences in the success rates were not verified between the protocols applied, indicating that the advantages in the treatment with the apical plug should be taken into consideration because they enable the earlier definitive restoration of the tooth, preventing the occurrence of fractures and/or the clinical failure. Therefore, MTA is a safer alternative for apical closing in traumatized teeth22.
Notwithstanding, it is worth noting that the dentist must be capable of executing such procedure so that the apical plug be restricted to the apical third and reach the proper sealing.
Conclusion
According to the results, it can be concluded:
• The treatment of teeht with incomplete root formation and necrotic pulp with MTA as apical plug exhibits the same clinical results of CH, with the advantage of shorter clinical time;
• Tooth trauma is the main etiology for the pulpal necrosis of the maxillary anterior teeth with incomplete root formation; The symptomatology between appointments has positive correlation with the size of the apical lesion;
• All cases presented clinical and radiographic success within a period shorter than eight months.
References
1. Andreasen JO, Andreasen FM, Andersson L. Textbook and color atlas for traumatic injuries to the teeth. 4. ed. São Paulo: Blackwell Publishing; 2006. [ Links ]
2. Castro A, Oliveira D, Diniz L, Eulália A, Paulillo L, Pereira G. Avaliação da utilização de MTA como plug apical em dentes com ápice aberto. Rev Bras Odontol. 2011 Jan/Jun;68(1):59-63. [ Links ]
3. Chueh L, Ho Y, Kuo T, Lai W, Chen Y, Chiang C. Regenerative endodontic treatment for necrotic immature permanent teeth. J Endod. 2009 Feb;35(2):160-4. [ Links ]
4. Cooke C, Rowbotham TC. Root canal therapy in nonvital teeth with open apices. British Dent J. 1960;108:147-50. [ Links ]
5. Cvek M. Prognosis of luxated non-vital maxillary incisors treated with calcium hydroxide and filled with gutta-percha. A retrospective clinical study. Endod Dent Traumatol. 1992 Apr;8(2):45-55. [ Links ]
6. Damle SG, Bhattal H, Loomba A. Apexification of anterior teeth: a comparative evaluation of mineral trioxide aggregate and calcium hydroxide paste. J Clin Pediatr. 2012 Sep;36(3):263-8. [ Links ]
7. De Deus G, Coutinho Filho T. The use of white Portland cement as an apical plug in a tooth with a necrotic pulp and wide-open apex: a case report. Int Endod J. 2007 Aug;40(8):653-60. [ Links ]
8. Desai S, Chandler N. The restoration of permanent immature anterior teeth, root filled using MTA: a review. J Dent. 2010;37:652-7. [ Links ]
9. Frank AL. Therapy for the divergent pulpless tooth by continued apical formation. J Amer Dent Assoc. 1966;72:87-93. [ Links ]
10. Goldstein S, Sedaghat-Zandi A, Greenberg M, Friedman S. Apexification & apexogenesis. N Y State Dent J. 1999;65(5):23-5. [ Links ]
11. Gomes-Filho JE, Watanabe S, Bernabé PFE, Costa MTM. A mineral trioxide aggregate sealer stimulated mineralization. J Endod. 2009 Feb;35(2):256-60. [ Links ]
12. Jeeruphan T, Jantarat J, Yanpiset K, Suwannapan L, Khewsawai P, Hargreaves KM. Mahidol study 1: comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods: a retrospective study. J Endod. 2012 Oct;38(10):1330-6. [ Links ]
13. Kvinnsland SR, Bardsen A, Fristad I. Apexogenesis after initial root canal treatment of an immature maxillary incisor – a case report. Int Endod J. 2010 Jan;43(1):76-83.
14. Leonardo MR. Endodontia: tratamento de canais radiculares – princípios técnicos e biológicos. 1. ed. São Paulo: Artes Médicas; 2005.
15. Maniglia-Ferreira C, Gurgel-Filho ED, Fröner IC, Moraes IG, De Deus G, Coutinho-Filho T. Avaliação clínica e radiográfica da apicificação em dentes traumatizados. Stoma. 2004;73:51-6. [ Links ]
16. Mente J, Hage N, Pfefferle T, Koch MJ, Dreyhaupt J, Staehle HJ et al. Mineral trioxide aggregate apical plugs in teeth with open apical foramina: a retrospective analysis of treatment outcome. J Endod. 2009;35(10):1354-8. [ Links ]
17. Morse DR, O’larnic J, Yesilsoy C. Apexification: review of the literature. Quint Int. 1990;21(7):589-98.
18. Ribeiro AD, Duarte MAH, Matsumoto MA, Marques MEA, Salvadori DMF. Biocompatibility in vitro tests of mineral trioxide aggregate and regular and white Portland cements. J Endod. 2005 Aug;31(8):605-7. [ Links ]
19. Sheehy EC, Roberts GJ. Use of calcium hydroxide for apical barrier formation and healing in non-vital immature permanent teeth: a review. British Dent J. 1997 Oct;183:241-6. [ Links ]
20. Tziafas D, Molyvdas I. The tissue reactions after capping of dog teeth with calcium hydroxide experimentally crammed into the pulp space. Oral Surg Oral Med Oral Pathol. 1988 May;65(5):604-8. [ Links ]
21. Tronstad L, Andreasen JO, Hasselgreen G, Kristerson L, Riis L. pH changes in dental tissue after root canal filling with calcium hydroxide. J Endod. 1981;7(1):17-21. [ Links ]
22. Trope M. Treatment of the immature toth with a non-vital pulp and apical periodontitis. Dent Clin N Am. 2010;54:313-24. [ Links ]
23. Walton RE, Torabinejad M. Principles and practice of endodontics. 2. ed. Philadelphia: WB Saunders Company; 1996. [ Links ]
 Corresponding author:
Corresponding author:
Cláudio Maniglia-Ferreira
Rua Bento Albuquerque, n. 685, apto. 1.102
CEP 60192-060 – Fortaleza – CE – Brasil
E-mail: maniglia@unifor.br
Received for publication: September 28, 2012
Accepted for publication: November 12, 2012













