Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.10 no.4 Joinville Out./Dez. 2013
ORIGINAL RESEARCH ARTICLE
The relationship of a clinical protocol and emergency treatment success of dental trauma running head: clinical protocol in dental trauma
Susimara Braga de Almeida I; Denise Piotto Leonardi II; Flávia Sens Fagundes Tomazinho II; Beatriz Serrato Coelho II; Allan Fernando Giovanini II; Eduardo Pizzato II; Flares Baratto-Filho II
I Department of Dentistry, University of Joinville – Joinville – SC – Brazil
II Department of Dentistry, Positivo University – Curitiba – PR – Brazil
ABSTRACT
Introduction and Objective: The aim of this study was to investigate whether the sequelae arising from dental trauma in permanent teeth were influenced by the use or non-use of a clinical protocol, in emergency care treatment facilities in the city of Joinville/SC, Brazil. Material and methods: From 2008 to 2010, a total of 70 dental records were reviewed and evaluated 6 months after the completion of treatment. In addition to the data relating to gender, age, etiology, most affected teeth, and most prevalent traumas, the individuals were divided into 2 groups to compare the sequelae observed following either the use or non-use of a clinical protocol for dental trauma treatment. Results: There was a greater incidence of male patients, particularly in the age-range of 8 to 15 years. Falls were the most frequent cause of trauma. The total success rate of the emergency care was of 78.57%. In the group in which the protocol was used, the success rate reached 88.89% compared to 60.0% in the group in which the protocol was not used. Conclusion: The use of a clinical protocol positively influenced the sequelae arising after treatment for dental trauma.
Keywords: prevention; tooth injury; dento-alveolar trauma.
Introduction
Dental trauma in permanent teeth can be considered a public health problem, and it can cause esthetic, psychological, and social problems in the patient, necessitating multidisciplinary treatment 6,14,15,17. After dental caries, accidents involving dental trauma are the most frequent cause of tooth loss, and a common cause of patients seeking emergency care services. Several studies on the epidemiology and prevalence of dental trauma have been conducted, and it has been suggested that where present, negligence or a lack of knowledge among the dentists performing the emergency care can compromise the treatment prognosis 4,8,9,17.
The complexity of dental trauma is variable and depends on the involvement of several tissues of different hardness, such as enamel, dentin, cementum, pulp, and periodontium; consequently, their repair is different 9. The sequelae resulting from dental trauma should be followed up at short- and long-term intervals; depending on the degree of complexity of the trauma, it may result in root resorptions, pulp necrosis, tooth mobility, and/or root canal calcification, as well as tooth loss 4,12,16.
In cases of dental trauma in which either a partial or total rupture of the neurovascular bundle occurs, the mechanisms of revascularization and reinnervation may initiate the accelerated deposition of hard tissue along with root canal walls resulting in root canal calcification; if there is a revascularization failure, pulp necrosis may occur. When the process of root resorption takes place, it is normally progressive and eventually results in tooth loss 11.
Clinical protocols are treatment guidelines based on scientific evidence, and their use is recommended to optimize treatment quality, materials used, and treatment time 1. The emergency care protocol used in this study has been well described by International Association for Dental Traumatology (IADT) 8, and it was reviewed by Flores et al. 5. With regard to cases of enamel–dentin fractures, the protocol recommends that dentin be protected with glass ionomer cement, or the fragment must be bonded. In such cases, radiographs should be taken, to detect possible root fractures or damage to other teeth, and the teeth should be followed up from 6-8 weeks to up to 1 year. In enamel–dentin–pulp fractures, pulp vitality should be confirmed, and a periapical radiograph should be taken to determine the stage of root formation. Treatment options in these cases include direct pulp capping, pulpotomy, or pulpectomy. In crown-root fractures, immediate treatment options are pulp capping, pulpotomy, or pulpectomy, followed by provisional bonding of the fragment or its removal, until a definitive treatment has been decided. When tooth extrusion occurs, tooth repositioning should be performed immediately, by applying light pressure on the alveolus, followed by flexible splinting for 2 weeks. Pulp status should be monitored for 4 weeks to up to 5 years. Lateral luxation demands tooth repositioning and splinting for 4 weeks, as well as pulp status control. When intrusive luxation happens and displacement of the tooth apex is complete, immediate tooth repositioning should be performed followed by pulpectomy; when tooth apex displacement is incomplete, spontaneous repositioning may occur, thus demanding preservation. Avulsed permanent teeth should be kept immersed in milk, saline solution, or saliva for no more than 60 min prior to repositioning of the tooth into the alveolus, followed by semi-rigid splinting for 2 weeks, both in cases of closed or open apex. Another recommendation is to hold the tooth by the crown, avoiding touching the root surface. Antibiotics and antitetanic serum drugs are required in cases where the tooth has touched the ground, and endodontic therapy should be initiated 7–10 days after replantation. If tooth replantation is performed after more than 60 min of extraoral time, it is necessary to clean the necrosed periodontal ligament and to perform endodontic therapy outside the mouth. Further, the tooth should be immersed into a 2% sodium fluoride solution for 20 min, followed by flexible splinting for 4 weeks 18.
The aim of this study was to investigate the relationships between the success and/or failure of emergency treatments administered to patients with traumatic injury to the teeth, and variables including the use or non-use of a clinical protocol, and the level of education, and the professional experience at an emergency care treatment facility in the city of Joinville/SC, Brazil.
Material and methods
This was a retrospective study conducted via analysis of the files of patients with a history of dental trauma treated at the public health services of the city of Joinville (SC, Brazil), from January 15, 2008 to January 15, 2010, and followed up for 6 months after the completion of emergency treatment. The study was approved by the ethical committee of Positivo University. The city of Joinville has 170 years and was mainly colonized by Germans. Currently, it is the biggest city in the state of Santa Catarina, with a total population of 1,094,570 inhabitants with the 13° highest Human Development Index of Brazil (0.857). From 440 patients that attended during the aforementioned period, 100 had suffered dental trauma, and of these, 70 returned for follow-up. The data from these 70 patients were organized with regard to age, gender, etiology, and type of and most frequent trauma. The teeth assigned for epidemiological study were then divided into 2 groups based on the use of standardized or non-standardized protocols. Group I (GI) comprised 25 patients whose initial emergency treatment was provided by professionals at the Basic Units of Health of the city of Joinville, the Emergency Care Offices of the south and north regions, or the São José Municipal Hospital, who did not use a standardized clinical protocol at that time. Group II (GII) comprised 45 patients who received emergency treatment at the Center for Dental Specialties (CDE II), using a clinical protocol suggested by the International Association of Dental Traumatology (IADT/2010) 8.
At the second stage, 6 months after the completion of treatment, patients were requested back for follow-up to identify possible sequelae. During the follow-up appointment, clinical and radiographic aspects of the patient data were evaluated. Success was defined as the lack of clinical or radiographic signs, and failure as the presence of clinical and/or radiographic signs indicating pulp necrosis, root resorption, root canal calcification, or tooth loss. Additionally, a questionnaire was administered to 140 professionals to determine their level of knowledge about dental trauma. The questions were related to both their level of education and their level of professional experience at the time of the first treatment.
Results
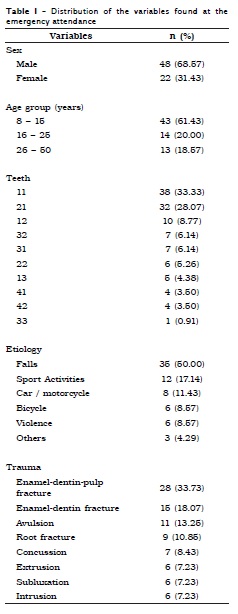
During the emergency attendance, 114 traumatized teeth were treated, in 70 patients, an occurrence rate of more than one traumatized tooth per patient. Of the 70 patients, 48 (68.57%) were male and 22 (31.43%) were female. The age group most affected by trauma was 8 to 15 years (61.43%), followed by 16 to 25 years (20.0%) and then 26 to 50 years (18.57%). The most frequently affected teeth were the permanent maxillary central incisors (61.40%). The most common cause was falls (50.0%), followed by sport activities (17.14%). The most frequent type of trauma was enamel–dentin–pulp fracture (33.73%), followed by enamel-dentin fracture (18.07%) and dental avulsion (13.25%) (table I).
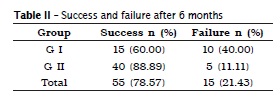
The total success rate was 78.57%; the success rate of group II was 88.89% compared to 60.0% for group I. Table II shows data obtained during the follow-up of the 70 patients in the study.
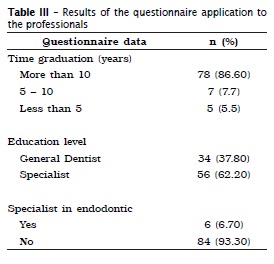
One hundred and forty (140) professionals received the questionnaire and 90 completed and returned it (a return rate of 64.3%). Of the 78 professionals (86.6%) had graduated more than 10 years prior to the study, 7 (7.7%) between 5 and 10 years prior to, and 5 (5.5%) had graduated less than 5 years prior to the study. Concerning their professional experience, 34 (37.8%) were general dentists, and 56 (62.2%) were specialists, in one of several areas. Of the 56 specialists, only 6 (6.7%) were endodontists. Table III shows the data obtained from the questionnaire.
Discussion
Dental trauma imposes an abrupt alteration on the quality of life of the affected individuals, not only in a physical but also in a psychological and social sense. This study evidenced this fact by confirming that the most affected teeth were the maxillary central incisors (61.4%), which corroborated the findings of Marcenes et al. 10, followed by the maxillary lateral incisors 11. With regard to the most frequent trauma types, a predominance of enamel–dentin–pulp fractures was observed (33.73%), which is similar to the results reported by Celenk et al. 3. In several cases, this condition requires that complex treatment be performed within the public health net 17. Unlike in the studies reported by Souza Filho et al. 18, and Sakai et al. 16, in this study enamel–dentin fractures were the second most common trauma type (18.07%). Among the cases involving the periodontium, avulsion was the most frequently observed trauma type 18.
Although the literature includes many studies on dental trauma epidemiology, in most regions there have been few studies reporting the application of a standardized clinical protocol for emergency treatment, and its relationship with the success rate after the completion of treatment 2. In the treatment of GII patients, where the standardized clinical protocol was employed, there were less sequelae than in GI patients, which mainly included cases of avulsion in which there was the need for tooth splinting and adequate guidelines for the patients regarding the need for periodical follow-up appointments for clinical and radiographic evaluations. The level of success reached in GII was 88.89%, versus 60.0% in GI, confirming the importance of the technical knowledge of the professional to the accuracy of diagnosis at the time of the initial emergency care, as well as the use of an adequate clinical protocol, validated in the scientific literature 1.
With regard to the knowledge of the professionals, most of them were specialists (62.2%); however, evidently they lacked appropriate clinical experience in the context of emergency treatment, because in the group I they did not apply a standardized clinical protocol when treating traumatized patients, which results in a doubtful prognosis, as confirmed by previous studies 13. On the other hand, the CDE II (GII) allocates emergency treatment to specialists in endodontics, which make the treatment faster owing to both the use of a protocol, and the experience of the professionals, as confirmed by Hu et al. 7, who observed a relative lack of knowledge in general dentists regarding dental trauma, as compared to that of endodontists.
The prevalence and treatment of dental trauma has been studied in Brazil as well as worldwide, and the significance of these studies has been demonstrated by epidemiologic data relating to dental trauma in permanent teeth in several places around the world 2,10,14,15. This study showed that application of a clinical protocol in the city of Joinville/SC, Brazil, enhanced the success rate of dental trauma treatment. The use of a standardized updated clinical protocol positively influenced the success rate of dental trauma, in this study. With regard to the dentists, the time since graduation and the level of dental education did not affect the prognosis of dental trauma.
References
1. Andersson L, Andreasen JO. Important considerations for designing and reporting epidemiologic and clinical studies in dental traumatology. Dent Traumatol. 2011;27:269-74. [ Links ]
2. Cavalcanti AL, Bezerra PK, de Alencar CR, Moura C. Dental injuries in 7 - to 12-years old Brazilian children. Dent Traumatol. 2009;25:198-202.
3. Celenk S, Sezgin B, Ayna B, Atakul F. Causes of dental fractures in the early permanent dentition: a retrospective study. J Endod. 2002;28:208-10.
4. De Rossi M, De Rossi A, Queiroz AM, Nelson Filho P Management of a complex dentoalveolar trauma: a case report. Braz Dent J. 2009;20:259-62.
5. Flores MT, Andersson L, Andreasen JO, Bakland LK, Malmgren B, Barnett F et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries. II. Avulsion of permanent teeth. Dent Traumatol. 2007;23:130-6.
6 . Glendor U, Jonsson D, Halling A, Lindqvist K. Direct and indirect costs of dental trauma in Sweden: a 2-year prospective study of children and adolescents. Community Dent Oral Epidemiol. 2001;29:150-60.
7. Hu LW, Prisco CR, Bombana AC Knowledge of Brazilian general dentists and endodontists about the emergency management of dento-alveolar trauma. Dent Traumatol. 2006;22:113-7.
8. IADT. The dental trauma guide: your tool to evidence based traumatology. 2010. Available from: URL:http://www.iadt.dentaltraumaguide.org.
9. Losso EM, Tavares MCR, Bertoli FMP, Baratto-Filho F. Dentoalveolar trauma in the primary dentition. RSBO. 2011;8:e1-18.
10. Marcenes W, Alessi ON, Traebert J. Causes and prevalence of traumatic injuries to the permanent incisors of school children aged 12 years in Jaraguá do Sul, Brazil. Int Dent J. 2000;50:87-92.
11. Majorana A, Bardellini E, Conti G, Keller E, Pasini S. Root resorption in dental trauma: 45 cases followed for 5 years. Dent Traumatol. 2003;19:262-5.
12. McCabe PS, Dummer PM. Pulp canal obliteration: an endodontic diagnosis and treatment challenge. Int Endod J. 2012;45:177-97.
13. Pedrini D, Panzarini SR, Poi WR, Sundeld ML, Tiveron AR. Dentists' level of knowledge of the treatment plans for periodontal ligament injuries after dentoalveolar trauma. Braz Oral Res. 2011;25:307-13.
14. Ramos-Jorge ML, Bosco VL, Peres MA, Nunes AC. The impact of treatment of dental trauma on the quality of life of adolescents – a case-control study in southern Brazil. Dent Traumatol. 2007;23:114-9.
15. Ramos-Jorge ML, Peres MA, Traebert J, Ghisi CZ, de Paiva SM, Pordeus IA et al. Incidence of dental trauma among adolescents: a prospective cohort study. Dent Traumatol. 2008;24:159-63.
16. Sakai VT, Magalhães AC, Pessan JP, Silva SM, Machado MA. Urgency treatment profile of 0 to15 year-old children assisted at urgency dental service from Bauru Dental School, University of São Paulo. J Appl Oral Sci. 2005;13:340-4.
17. Sharma D, Garg S, Sheoran N, Swami S, Singh G. Multidisciplinary approach to the rehabilitation of a tooth with two trauma episodes: systematic review and report of a case. Dent Traumatol. 2011;27:321-6.
18. Souza-Filho FJ, Soares AJ, Gomes BPFA, Zaia AA, Ferraz CCR, de Almeida JFA. Avaliação das injúrias dentárias observadas no centro de trauma dental da Faculdade de Odontologia de Piracicaba – Unicamp. RFO. 2009;14:111-6.
 Corresponding author:
Corresponding author:
Flares Baratto-Filho
Mestrado em Odontologia, Universidade Positivo
Rua Professor Pedro Viriato Parigot de Souza, n. 5.300, Campo Comprido
CEP 81280-330 – Curitiba – PR – Brasil
E-mail: fbaratto1@gmail.com
Received for publication: July 22, 2013
Accepted for publication: August 14, 2013













