Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.11 no.1 Joinville Jan./Mar. 2014
ORIGINAL RESEARCH ARTICLE
Immunoexpression of BMP-2 protein on bone repair of critical size defects treated with autogenous macerated adipose tissue
Clayton Luiz Gorny JuniorI; Allan Fernando GiovaniniI; Juliana VieiraI; João Cézar ZielakI; Felipe Rychuv SantosI; Carmen Lucia Mueller StorrerI; Tatiana Miranda DeliberadorI
I Program of Professional Master Course in Clinical Dentistry, Positivo University – Curitiba – PR – Brazil
ABSTRACT
Introduction: The adipose tissue is an important reservoir of adult stem cells which have capacity of differentiating in osteoblasts with potential implication in reaching bone regeneration. The evaluation of the osteoblastic differentiation can be verified through immunohistochemical markers such as bone morphogenetic protein- 2 (BMP-2). Objective: To evaluate the immunoexpression of BMP-2 protein on the bone repairing of critical size defects (CSD) surgically created in rat calvaria and treated by autogenous macerated adipose tissue. Material and methods: Forty male rats had a CSD measuring 5 mm created on their calvaria. The animals were randomly divided into two groups: group C (control) and group AT (macerated adipose tissue grafting). In group C, the defect was filled with only blood clot. In group AT, the defect was filled with autogenous macerated adipose tissue. The groups were subdivided into two subgroups (n = 10) for euthanasia at 7 and 90 post-operative days. Histological and immunohistochemical analyses were carried out. Data were submitted to descriptive statistics (mode). Results: In group AT, both at 7 and 90 post-operative days, the main healing type was the presence of dense conjunctive tissue exhibiting bundles of collagen fibers disposed in beams permeating the remaining adipose tissue with rare heterotopic bone formation associated to fibrosis and different types of tissue necrosis. In group C, the repair was achieved by the formation of bundles of collagen fibers oriented parallelly to the surface of the wound at the two post-surgical periods. The immune-staining of BMP-2 was present only in group C (7 and 90 post-operative days). Conclusion: Within the limits of this present study, it can be concluded that the adipose tissue grafting did not favor bone neoformation in critical size defects and BMP-2 signaling was not observed.
Keywords: adipose tissue; calvaria; bone regeneration.
Introduction
The repair of extensive bone defects, caused by either traumas or pathologies, constituted a great problem for both Medicine and Dentistry. Despite of the great potential of repair by bone tissue, in some situations, according to the proportion of defects, the regeneration cannot be complete because the defect can be invaded by the surrounding conjunctive tissue which has a proliferation and cellular migration speed faster than those of bone tissue. Thus, the use of bone grafting can collaborate with the repair process. To achieve better results, the graft should preferentially osteogenic, osteoinductive and osteoconductive 6.
Tissue bioengineering is a new branch of Science aiming to investigate and integrate techniques of tissue regeneration thorugh new biomaterials including natural markers (growth factors) and tissue and cellular components (mesenchymal stem cells). Thus, the search for new materials helping the bone healing process have found different ways from those of the use of autogenous and xenogenous bones; bioceramics and bioglasses, raising great interest in the research with adipose tissue as a reservoir of adult stem cells, generating good results. Mesenchymal stem cells have the ability to differentiate in osteoblasts with potential implications for the engineering of human bone tissue 11. The stem cells coming from the adipose tissue can be an important source of progenitor mesenchymal stem cells which can be employed in tissue engineering for bone repairing 8.
Currently, Zou et al. 13 verified that stromal cells (CD 34+) derived from the adipose tissue has the potential of osteogenic differentiation both in vitro and in vivo, being considered as a promising cellular therapy for the healing of bone defects. The adult unilocular subcutaneous adipose cells have the potential in vitro to redifferentiate in osteoblast (transdifferentiation). This transdifferentiation capacity can hypothetically favor bone repairing procedures 3.
The presence of osteoblasts is an important requisite in the effectiveness and success of the bone repairing. This evaluation of osteoblastic differentiation is commonly evaluated through different protein markers, among them bone morphogenetic protein-2 (BMP-2).
Currently, there are little studies evaluating whether the adipose tissue is really a safe option to reach bone repairing. For this reason, studies on animals can clarify the quality and type of bone healing when adipose tissue grafting is used. The aim of this study was to evaluate the immunoexpression of BMP-2 protein on bone repairing of critical size bone defects surgically created in rat calvaria, treated with macerated adipose tissue grafting.
Material and methods
This present study was submitted and approved by the Ethical Committee in Research of Positivo University, Curitiba (PR), under protocol no. 019/2009. Forty male rats (Rattus norvegicus, albinus, Wistar), aged from about 5 to 6 months, weighing from 400 to 600 grams were selected. The animals were randomly divided into two groups: group C (control) and group AT (macerated adipose tissue). The animals had good health conditions. They were kept at every 4 inside a box in the vivarium of Positive University and received solid food and mineral water ad libitum.
Anesthetic protocol
To conduct the surgical and experimental procedures, the animals were individually placed inside a campane and submitted to inhaling anesthesia with oxygen and isoflurane (Cristália, Itapira, SP, Brazil) and then anesthetized by intramuscular injection at the posterior part of the thigh with 2.3 g of xylazine (0.52 mg/kg) (Vetbrands, Paulínia, SP, Brazil) and 1.16 g ketamine (1.04 mg/kg) (Vetbrands, Paulínia, SP, Brazil).
Surgical procedures
After anesthesia, all animals were submitted to trichotomy on the calvaria; the animals of group AT also received trichotomy on the abdominal area (to collect the adipose tissue).
Next, antisepsis was performed and a U-shaped incision was executed with the aid of a size 15c scalpel blade to access the calvarium area to raise a total flap towards the posterior direction.
A critical size defect (CSD) measuring 5 mm in diameter, trans-osseous 10, was created with the aid a trephine bur coupled to a counter-angle handpiece for implant (20:1, Kavo, Joinville, SC, Brazil), under copious irrigation with sterile saline solution. The defect reached a portion of the sagittal suture. The removal of the bone block was carefully executed with the aid of spatulas to avoid the meninges rupture.
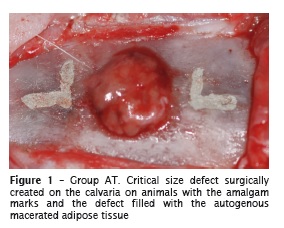
With the aid of a millimetric probe (PCPUNC 15, Hu-Friedy, Chicago, IL, USA) and a number 701 conical trunk carbide drill coupled to a straight handpiece was used to create two L-shape marks: 2 mm towards anterior and 2 mm towards posterior of the margins of the surgical defect. The long axis of each L was located onto an imaginary longitudinal line that divided the surgical defect by half. The other marks were filled with dental amalgam (Permite – SDI, Victoria, Australia) both to identify the middle of the original surgical defect during laboratorial processing and to locate its original bone margins during histological analysis (figure 1).
In group C, the surgical defect was filled with blood clot. In group AT, the defect was filled with macerated adipose tissue (figure 1). To obtain autogenous adipose tissue, an incision was performed with the aid of a size 15 scalpel blade, parallelly to the right posterior limbs onto the abdominal area with size of about 1 cm. The adipose tissue of the exposed area was carefully removed with the aid of scissors and tweezers and then macerated with size 15c scalpel blade through random cuts into different directions and immediately grafted into the surgical defect.
The soft tissues were then repositioned and sutured with silk thread 4-0, (Ethicon, Johnson & Johnson, São José dos Campos, SP, Brazil) to obtain a primary closure of the wound both in the donor (abdominal area) and receptor (calvaria) sites.
To control post-operative pain, the animals received morphine sulphate (3 mg/kg) (União Química, Jabaqua ra, SP, Bra zi l), throug h intramuscular injection, at the ending of the surgery. Analgesia was kept with 20 drops of paracetamol (200 mg/kg) diluted into 400 ml of water placed into the drinking fountain for three days.
The groups were divided into subgroups (n = 10), for euthanasia at 7 and 90 post-operative days. The animals were positioned in a gas chamber (CO2) and maintained for 10 minutes which was the time amount required to the complete euthanasia.
Tissue processing
The area of the original surgical defect and the surrounding tissues were removed in block. The pieces were fixed into 10% neutral formaldehyde, washed in running water and decalcified in 20% formic acid. Then, each piece was hemi-sectioned at the center parallelly to the sagittal suture by using the long axis of each L-shaped amalgam mark. Thus, it was possible to determine precisely the limits of the original surgical defect for histological and immunohistochemical analyses. The pieces were processed and included into paraffin. Next, serial longitudinal cuts measuring 3 μm in thickness were executed, initiating at the center of the original surgical defect. The cuts were stained by hematoxylin and eosin (HE) for light microscopy analyses.
Histological analysis
Two histological cuts representing the center of the original surgical defect of each animal were selected for histological analysis. All analyses were conducted by a single operator previously trained. Qualitative histological analysis was carried out by optical microscope (021/3 Quimis, Diadema, SP, Brazil), and the following parameters were assessed: the closure of the bone defect; the type of the neoformed bone; the characteristics of conjunctive tissue; the presence of osteoid matrix; the presence of chronic and acute inflammatory infiltrate; the progression of the repairing type present in the defect created surgically; and the thickness of the neoformed tissues compared with the original bone of calvaria. The closure of the defect was considered as complete when all its extension was filled by neoformed bone tissue. Also, the presence of remnants of macerated adipose tissue graft was assessed.
Immunohistochemical analysis
Two histological cuts representing the center of the original surgical defect of each animal were selected for immunohistochemical analysis. All analyses were conducted by a single operator previously trained. Immunohistochemical antiperoxidase analysis through BMP-2 antibody was carried out. The immunoexpression of the protein was obtained through streptavidin-biotin-immunoperoxidase.
The images for each field were obtained by light microscopy at x400 magnification, under fixed light focus. The images visualized on a TV screen coupled to a computed system were digitized by camera system (SDC-310 Samsung, Corrêa) coupled to the light microscope (021/3 Quimis, Diadema, SP, Brazil). The manual counting of the nucleus expressing immune-staining was executed for the protein studied.
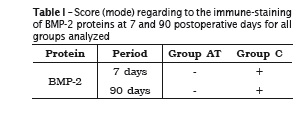
To evaluate the data of the immunohistochemical analysis (quantitative analysis), it was employed a semi-quantitative score, ranging from: "-" for the lack of staining to 10% of immunopositivity; "+" for 10-25%; "++" for 25-50%; "+++" for 50-75% and "++++" for more than 75%. The semi-quantitative immunohistochemical analysis was chosen because BMP-2 protein was expressed both in the cells and extracellular matrix.
Statistical analysis
Data was submitted to descriptive statistics (mode). Mode is the value representing the greatest number of observations, that is, the most frequent value or values. The mode is not necessarily one, rather than mean and median. It is especially useful when the values or observation are not numerical, since the mean and median cannot be well defined.
Results
Histological analysis
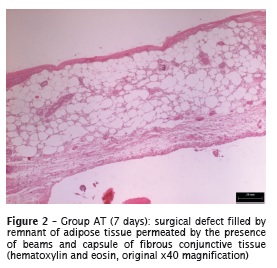
Group AT: 7 post-surgical days
At this period, there was not the completely closure of the wound. Mostly, the extension of the defect was occupied by remnants of adipose tissue graft permeated by the presence of beams and capsule of dense fibrous conjunctive tissue (figure 2), which was also permeated by intense presence of chronic inflammatory infiltrate predominantly with lymphocytes and plasmocytes. In the body of the defect, it was also observed the sound architecture of the anuclear adipose tissue, suggesting ischemic/coagulative necrosis karyolysis. It was not verified any bone neoformation in none of the specimens analyzed.
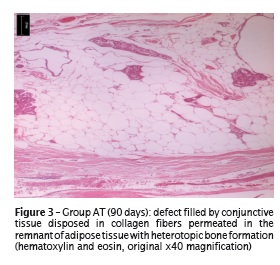
Group AT: 90 postoperative days
It was not verified the complete closure of the bone defect. The reparative histology showed the presence of the dense conjunctive tissue exhibiting bundles of collagen fibers disposed in beams permeated in the remnant adipose tissue and presence of heterotopic bone formation associated with fibrosis (figure 3).
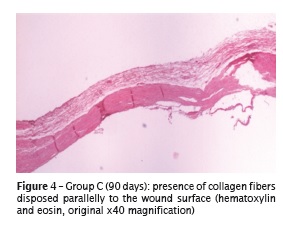
Group C: 7 and 90 postoperative days
The microscopic features at these periods did not show the closure of the bone defect. All healing area was composed by dense conjunctive tissue with bundles of collagen fibers parallelly to the surface of the wound (figure 4), permeated by intense chronic lymphoplasmocytic inflammatory process at 7 postoperative days. A small amount of neoformed bone tissue was seen at the defect margins at 90 postoperative days.
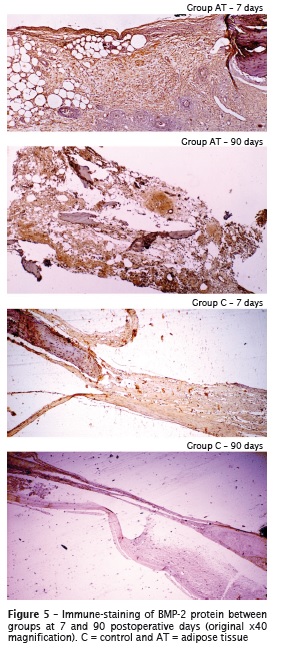
Qualitative immunohistochemical analysis
At both experimental periods, all specimens treated with adipose tissue (groups AT), did not exhibited the presence of BMP-2 protein. This result coincides with the lack of bone neoformation in this group. In group C, the immune-staining occurred at the margins of the defect, in areas containing the bone remaining (figure 5).
Quantitative immunohistochemical analysis
The results of quantitative immunohistochemical analysis are seen in table I.
Discussion
The aim of this present study was to evaluate the immunoexpression of BMP-2 protein on the bone repairing of critical size defects surgically created in rat calvaria, treated with macerated adipose tissue. In this study, it could be observe that the macerated adipose tissue hindered the bone repair. This result is similar to those found recently by Zanicotti et al. 12, Matsubara et al. 5 and Oliveira et al. 7. Zanicotti et al. 12 and Matsubara et al. 5 evaluated the use of non-processed adipose tissue in the treatment of peri-implantar bone defects. According to these authors, the adipose tissue seems to prevent the bone formation around the implant. Oliveira et al. 7 evaluated the influence of macerated adipose tissue on the bone repairing of bone defects created surgically on rabbit calvaria. The results demonstrated that macerated adipose tissue grafting did not favor positively the amount of bone neoformation.
The negative result of the adipose tissue in the bone repairing was evident in this present study because there was no immune-staining of BMP-2 protein, which evaluates the osteoblastic di f ferent iat ion and has been considered as osteogenesis modulators. BMP-2 was seen in group C at small amount at 7 and 90 postoperative days, showing that there exists the presence of osteoblastic cells. In this sense, it can be said that the adipose tissue formed a physical necrotic barrier impeding the bone neoformation. Moreover, in group AT, there was either ischemic or microcystic necrosis. These different necrosis types favored the negative response of bone neoformation.
The transdifferentiation of mature adipocytes into osteoblasts is already documented in literature, both in in vivo and in vitro studies, confirming that adipocytes can be good candidates for tissue engineering protocols aiming to bone tissue development 3. Notwithstanding, in this present study, this transdifferentiation process could not be proved.
The transplant of adipose tissue to ectopic site has the self-capacity of heterotopic mineralization 4. Areas of heterotopic mineralization were observed in some specimens of groups AT. It is important to emphasize that these areas cannot be considered as osteoid tissue. The rationale behind this presence is that all necrotic fat is caused by the saponification which attracts calcium salts 9.
Studies have shown that the adipose tissue can secrete proteins so-called adipokine, and the stem cells derived from this tissue are "tripotent", with potential capacity of adipogenic, chondrogenic and osteogenic differentiation 1,2,14. Notwithstanding, in this present study, the use of autogenous macerated adipose tissue favored the necrotic rather than osteogenic process.
Conclusion
Within the limits of this present study, the macerated adipose tissue grafting did not favor bone neoformation in critical size defects by the suppression of BMP-2 protein signaling.
References
1. Fruhbeck G, Gomez-Ambrosi J, Muruzabal FJ, Burrell MA. The adipocyte: a model for integration of endocrine and metabolic signaling in energy metabolism regulation. Am J Physiol Endocrinol Metab. 2001 Jun;280(6):E827-47. [ Links ]
2. Gimble JM, Katz AJ, Bunnell BA. Adiposederived stem cells for regenerative medicine. Circ Res. 2007 May 11;100(9):1249-60.
3. Justesen J, Pedersen SB, Stenderup K, Kassem M. Subcutaneous adipocytes can differentiate into bone-forming cells in vitro and in vivo. Tissue Eng. 2004 Mar-Apr;10(3-4):381-91.
4. Kaplan FS, Glaser DL, Hebela N, Shore EM. Heterotopic ossification. J Am Acad Orthop Surg. 2004 Mar-Apr;12(2):116-25.
5. Matsubara FB, Zanicotti DG, Zielak JC, Giovanini AF, Gonzaga CC, de Andrade Urban C. et al. Nonprocessed adipose tissue graft in the treatment of dehiscence bone defects in rabbit tibiae: a pilot study. Implant Dent. 2012 Jun;21(3):236-41.
6. Misch CE, Dietsh F. Bone-grafting materials in implant dent istry. Implant Dent . 1993 Fall;2(3):158-67.
7. Oliveira LD, Giovanini AF, Abuabara A, Klug LG, Gonzaga CC, Zielak JC, et al. Fragmented adipose tissue graft for bone healing: histological and histometric study in rabbits calvaria. Med Oral Patol Oral Cir Bucal. 2013 May 1;18(3):510-5.
8. Qu CQ, Zhang GH, Zhang LJ, Yang GS. Osteogenic and adipogenic potential of porcine adipose mesenchymal stem cells. In Vitro Cell Dev Biol Anim. 2007 Feb;43(2):95-100.
9. Requena L. Normal subcutaneous fat, necrosis of adipocytes and classification of the panniculitides. Semin Cutan Med Surg. 2007 Jun;26(2):66-70.
10. Schmitz JP, Hollinger JO. The critical size defect as an experimental model for craniomandibulofacial nonunions. Clin Orthop Relat Res. 1986 Apr;(205):299-308.
11. Weinzierl K, Hemprich A, Frerich B. Bone engineering with adipose tissue derived stromal cells. J Craniomaxillofac Surg. 2006 Dec;34(8):466-71.
12. Zanicotti D, Brugin Matsubara F, Zielak JC, Giovanini AF, de Andrade Urban C, Miranda Deliberador T. J Oral Implantol. 2011 Nov 21.
13. Zou J, Wang G, Geng D, Zhu X, Gan M, Yang H. A novel cell-based therapy in segmental bone defect: using adipose derived stromal cells. J Surg Res. 2011 Jun 1;168(1):76-81.
14. Zuk PA, Zhu M, Mizuno H, Huang J, Futrell JW, Katz AJ et al. Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng. 2001 Apr;7(2):211-28.
 Corresponding author:
Corresponding author:
Tatiana Miranda Deliberador
Mestrado em Odontologia, Universidade Positivo
Rua Professor Pedro Viriato Parigot de Sousa, n. 5.300 – Campo Comprido
CEP 81280-330 – Curitiba – PR – Brasil
E-mail: tdeliberador@gmail.com
Received for publication: October 12, 2013
Accepted for publication: November 20, 2013













