Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.11 no.1 Joinville Jan./Mar. 2014
CASE REPORT ARTICLE
Masseteric cysticercosis: an uncommon appearance diagnosed on ultrasound
Vinod Vijay ChanderI; Sridevi KoduriI; Atul KaushikI; Manpreet KalraII; Renu TanwarI; Sukeerat MannI
I Department of Oral Medicine & Radiology, S.G.T. Dental College, Hospital and Research Institute – Gurgaon – Haryana – India
II Department of Oral Pathology, S.G.T. Dental College, Hospital and Research Institute – Gurgaon – Haryana – India
ABSTRACT
Introduction: Cysticercosis occurs when man is infested by the larvae of Taenia solium. Cysticercosis involving the maxillofacial region is not only an uncommon event, but also represents a difficulty in clinical diagnosis. Objective: The present manuscript highlights masseteric cysticercosis as a differential diagnosis of chronic maxillofacial swellings and the role of high resolution sonography as an important noninvasive and non-ionizing imaging modality. Case report: We present a case of masseteric cysticercosis in an eight year old Indian boy, its clinical features, the imaging modalities required and adequate management of the case. Conclusion: Cysticercosis should always be a part of the differential diagnosis of maxillofacial swellings. A thorough case history, clinical examination, proper investigations and conservative treatment forms the mainstay for management of affected patients.
Keywords: masseter cysicercosis; ultrasonography; nonsurgical management.
Introduction
Cysticercosis is an infect ion caused by cysticercus (Gr. kystis: bladder + kerkosi: tail), a larval form of Taenia species. Among various species, the larval form of Taenia Solium i.e., cysticercus cellulosae infest human beings 1. The location of cysticercosis in the order of frequency is central nervous system, subcutaneous tissue, striated muscle, vitreous humor of the eye and rarely other tissues 2. Cystcerci in muscles generally do not cause symptoms, however oral and maxillofacial region is not a frequent site of occurrence for cysticercosis despite the presence of abundance of muscular tissue. This article presents a case of cysticercosis involving the masseter as a facial swelling, diagnosed with high-resolution ultrasonography and managed conservatively.
Case report
An 8-year-old boy reported to the Department of Oral Medicine & Radiology, SGT Dental College & Hospital, Gurgaon with a complaint of swelling in his left cheek since two years. There was a history of intermittent reduction in size of swelling followed by medication by a local practitioner. There was also associated occasional fever and irritability. Medical and dental history revealed that this was the first visit to a dental office and patients' father reported history of weight loss and reduced appetite since last 2 years. Although the patient was not a vegetarian, there was no history of consumption of pork and the family history was non-contributory.
On general examination, he was conscious and coherent with normal gait and was poorly built. Signs of pallor were appreciated in palpebral conjunctiva and nail bed. His body was febrile with temperature raised to 37ºC. His height was 1.21 m and he was underweight by 4 kg.
Extraoral examinat ion revea led facia l asymmetry due to the swelling in left lower third of face. On palpation the dome shaped swelling was tender, firm and non-fluctuant measuring 3.5 cm superoinferiorly 4.0 cm anteroposteriorly. On clenching, the swelling was slightly bulged and hence suggested masseter involvement (figure 1). Left submandibular and preauricular nodes were palpable, one on each side, oval, firm, tender and freely movable.

Intraoral examination revealed a healthy mixed dentition phase without any carious lesion or periodontal pathology. A provisional diagnosis of juvenile fibroma was given and differential diagnoses of fibroma, cysticercosis, intramuscular hemangioma and intramuscular lipoma were considered. For subsequent invest igat ions, informed consent from the patient's parents and approval from ethical committee of the institute were taken.
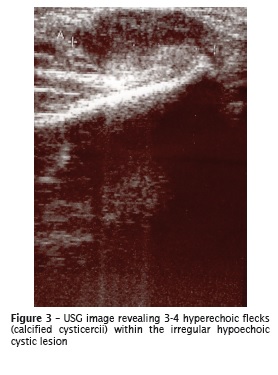
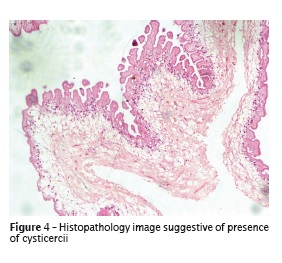
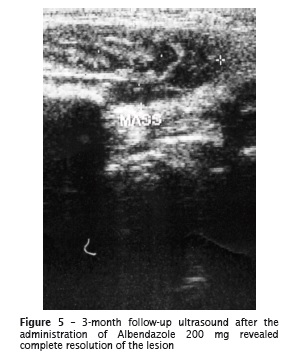
The panoramic radiograph was unremarkable (figure 2) and the pat ient was referred for ultrasonography (USG). USG was performed with a Voluson 730 scanner (GE Healthcare) using 12 Mhz linear transducer. Left masseter revealed a mixed lesion with characteristic 3-4 hyperechoic f lecks surrounded by an irregular hypoechoic pat tern (figure 3) sug gest ive of cysticercosis. Enlarged lymph nodes measuring 2-6 mm were noted. Incisional biopsy of the lesion was performed which confirmed the diagnosis of left masseteric cysticercosis with subacute inflammation (figure 4). The patient was managed conservatively with 200 mg Albendazole for 28 days. A follow-up ultrasound was done after 15 days which revealed reduction in size of the lesion and a third follow-up ultrasound was done after 3 months which revealed complete resolution of the lesion (figure 5).

Discussion
Cysticercosis in humans is a parasit ic infestation caused by the larval stage of the pork tape worm (Taenia Solium), cysticercus cellulosae. It results from the ingestion of the tape worm eggs through either fecally contaminated food and water as well as self-contamination by ref lux of the proglattid from the intestine or contaminated hands 3-5. The oncospheres develop from the eggs, penetrate into the intestinal wall and via lymphatic or vascular circulation and reach various tissues where larvae develop and become the cysticercior "bladder worm" a fluid filled cyst 3. The mode of entry of nematode in the present case reported could be attributed to the ingestion of contaminated food/water. The larvae can remain viable at this stage for as long as ten years in humans. Living larvae evade immune recognition and do not elicit inf lammation. When the larva dies, it induces a vigorous granulomatous inf lammatory response that produces symptoms, depending on the anatomic location. Cysticercosis can affect various organs including brain, spinal cord, orbit, muscle and heart.
Oral and maxillofacial region is not a frequent site of occurrence for cysticercosis despite the presence of abundant muscular tissue. The age of incidence varies from young children to older adults with equal gender predilection. The common sites of involvement included tongue, lips and buccal mucosa 6. The clinical features and differential diagnosis depend on the number and location of cysticerci as well as the extent of associated inflammatory response or scarring. Neurological manifestations, known as neurocysticercosis, are most common and may manifest as seizures, hydrocephalus and signs of raised intracranial tension 7.
Muscular cysticercosis may clinically present in three dist inct types: myalgic, mass-like, pseudotumor or abscess-like as well as the rare pseudohypertrophic type. During the death of the larva, there is leakage of fluid from the cyst. The resultant acute inflammation may cause local pain and myalgia. Alternatively, degeneration of the cyst may result in intermittent leakage of fluid, eliciting a chronic inflammatory response, with collection of fluid around the cyst leading to a mass-like type as seen in our case. Alternatively, the cyst retracts, its capsule thickens and the scolex calcifies 8.
Ultrasonography can be effectively used to diagnose the cases of soft tissue cysticercosis besides various other methods such as: radiologic imaging, serology, computed tomography, magnetic resonance imaging 9, and fine needle aspiration cytology 4. There are only few reports of the ultrasound features of muscular cysticercosis 10-12. Four different sonographic appearances in cysticercosis have been described by Vijayaraghvan 10. On ultrasound, cysticercosis can appear as the cysticercus cyst with an inflammatory mass around it, as a result of the death of the larva. The second type can be seen an irregular cyst with very minimal fluid on one side, indicating the leakage of fluid. The eccentric echogenic protrusion from the wall due to the scolex is not seen within the cyst. It may be due to escape of the scolex outside the cyst or partial collapse of the cyst. The third appearance is a large irregular collection of exudative fluid within the muscle with the typical cysticercus cyst containing the scolex, situated eccentrically within the collection. The fourth sonographic appearance as seen in the present case reported here is that of calcified cysticercosis. It appears as multiple elliptical calcifications in soft tissue similar to the pathognomonic millet seed shaped elliptical calcifications in soft tissues described on plain radiography. These four appearances on high resolution ultrasonic are pathognomonic of cysticercosis and a definitive diagnosis can be made with great confidence 10.
Surgical removal is indicated for localized lesions that cause obvious symptoms, however medical management with antihelminthetics such as either praziquantel or albendazole has been recommended for neurocysticercosis and subcutaneous cysticercosis 12,13. The case reported has been managed conservatively only with albendazole. Notwithstanding, preventive measures are also important including proper sanitation, good personal hygiene, thorough cooking of pork and all vegetables along with early detection and complete removal of the worm.
Conclusion
Cysticercosis should always be a part of the differential diagnosis of maxillofacial swellings. High-resolution, non-invasive and non-ionizing ultrasound plays an important role in diagnosing soft tissue cysticercosis. However, histopathology is still the gold standard for confirmatory diagnosis. Although surgical removal is indicated for localized lesions, conservative medical management can also be considered along with the preventive measures.
References
1. Asrani A, Morani A. Primary sonographic diagnosis of disseminated muscular cysticercosis. J Ultrasound Med. 2004;23:1245-8. [ Links ]
2. Elias FM, Martins MT, Foronda R, Jorge WA, Araujo NC. Oral cysticercosis: case report & review of literature. Rev Inst Med Trop. 2005;47(2):95-8.
3. Jacobs RA. Infectious diseases: protozoal and helminthic. In: Tierney LM, Mephee SJ, Papadakes MAS (eds). Continuous medical diagnosis and treatment. 45th ed. New York: McGraw-Hill; 2006. p. 1463-536.
4. Richards Jr. F, Schantz PM. Laboratory diagnosis of cysticercosis. Clin Lab Med. 1991;11:1011-28.
5. Romero Deleon E, Aguirra A. Oral cysticercosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:572-7.
6. Saran RK, Rattan V, Rajwanshi A, Nijkawan V, Gupta SK. Cysticercosis of the oral cavity: report of five cases and a review of literature. Int J Paediat Dent. 1998;8:273-8.
7. Schmidt DKT, Jordaan HF, Schneider JW. Cerebral and subcutaneous cysticercosis treated with albendazole. Int J Dermatol. 1995;34:574-9.
8. Scully RE, Mark EJ, McNeely WF. Case records of the Massachusetts General Hospital Weekly clinicopathological exercises, case 26, 1994. N Engl J Med. 1994;330:1887.
9. Sidhu R, Nada R, Palta A, Mohan H, Suri S. Maxillofacial cysticercosis: uncommon appearance of a common disease. J Ul trasound Med. 2002;21:199-202.
10. Sivapathasundharam B, Gururaj N. Mycotic infections of the oral cavity. In: Rajendran R, Sivapathasundharam B. Shafer, hine, levy. Shafers textbook of oral pathology. 5th ed. India: Elsevier; 2006.
11. Timosca G, Gavrilita L. Cysticercosis of the maxillofacial region. A clinicopathological study of five cases. Oral Surg Oral Med Oral Pathol. 1974;37:390-400.
12. Vijayraghavan SB. Sonographic appearences in cysticercosis. J Ultrasound Med. 2004;23:423-7.
13. White AC, Wella PF. Cestodes. In: Kasper DL, Braunwald E, Fauci AS, Hansea SL, Lango DL, James JL. Harrisons principles of internal medicine. 16th ed. New York: McGraw Hill; 2004. p. 1272-6.
 Corresponding author:
Corresponding author:
Sridevi Koduri
Department of Oral Medicine & Radiology
S.G.T. Dental College, Hospital and Research Institute
Gurgaon – Haryana – India
E-mail: drsrident@gmail.com
Received for publication: April 18, 2013
Accepted for publication: August 1, 2013













