Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.11 no.2 Joinville Abr./Jun. 2014
ORIGINAL RESEARCH ARTICLE
Evaluation of oral hygiene index, monitoring and oral hygiene instruction in visually impaired people
Jackyeli Windmuller I; Rafaela Araujo Mendes I; Sheila de Carvalho Stroppa I; Juliana Yassue Barbosa da Silva I
I School of Dentistry, Positivo University – Curitiba – PR – Brazil
ABSTRACT
Introduction: Eyesight can be considered a major human interaction promoter in motor, perceptual and mental activities and its loss can cause social environment changes. Objective: To evaluate and determine Simplified Oral Hygiene Index (OHI-S) in visually impaired individuals, as well as to provide information to promote oral health, to verify the effectiveness of educational activities for index change and to promote the social inclusion of visually impaired people. Material and methods: Study population was constituted by 28 visually impaired people of both genders, aged from 14 to 75 years old, residents and students at the Parana Institute for the Blind (IPC), Curitiba (PR, Brazil). The study was conducted in three stages. At first, the participants individually answered a questionnaire, performed tooth brushing and then the disclosure of oral biofilm was made, as well as the evaluation of Simplified Oral Hygiene Index, oral hygiene instruction and supervised toothbrushing. The second step was performed after seven days and the third after thirty days to reassess the Simplified Oral Hygiene Index to check whether there would a change in their values. Participants were divided into two groups according to Simplified Oral Hygiene Index: those who had only bacterial plaque and those who had plaque and calculus. Results: At the first day, patients with plaque and calculus had initial OHI-S mean of 2.3 (regular), 2.1 (regular) after seven days, and 2.4 (regular) after one month. Patients with only plaque at the first day had an average OHI-S of 0.71 (regular), 0.74 (regular) after seven days, and 0.78 (regular) after one month. Conclusion: Within this context, it is possible to understand that it is necessary to implement frequent supervised toothbrushing, oral instruction and motivation activities to promote wellness and health for these patients.
Keywords: oral hygiene index; visually impaired people; Dentistry.
Introduction
According the last research conducted by the Brazilian Institute of Geography and Statistics (IBGE), proved by the Brazilian Census of 2010, visual impairment is the most frequent impairment among all types reaching the Brazilian population. Currently, in Brazil, 18.8% of population had visual impairment 5.
Although the number of visual impaired people is representative of Brazilian population few studies in literature have evaluated the oral health quality in this individual group. Gradually, this situation has been changing through professionals aiming to include these individuals within the society, inserting them in programs of health attention and creating a differentiated service according to the difficulties of each person 6.
A visually impaired person needs a health professional licensed to stimulate the other sensory senses, such as touch, taste and hearing, so that the communication between the professional and patient is positive and the patient does not exhibit social relationship difficulties 3,11.
Dental care oriented to individuals with special needs, particularly those with visual impairments, is still precarious in Brazil. Visually impaired people have shown oral health problems foreshadowed by factors as lack of motivation, difficult of proper toothbrushing for plaque control and scarce professional guidance turned to this population type 9.
To achieve treatment success and routinely proper oral hygiene, precaution in the instruction, perseverance in teaching the techniques, and the project of health promotion directed to the blind patient, should be accomplished in a controlled manner by the caregivers and/or relatives in addition to the patient's compliance 1,3,6,14.
Both the compliance and motivation of the patients are indispensable to achieve significant improvement in oral health. Moreover, the dental professional is essential in oral health promotion, providing oral health improvement and quality of life. Therefore, currently, the Dentistry leaves curative profile and comes towards preventive profile 7,9.
The Brazilian federal laws no. 10.048, from November 8 of 2000, and no. 10.098, from December 19 of 2000, which establish general guidelines and basic criteria for accessibility promotion for people with disabilities or reduced mobility, claims that visual impairment is considered blindness when visual accuracy is equal or smaller than 0.05º (degrees) at the best eye, with the best optical correction. On the other hand, is considered as poor eyesight when the visual accuracy is between 0.3º and 0.05º at the best eye with the best optical correction 4.
According to the study of Cericato and Fernandes 7, people with poor neuropsychomotor capacity difficultly accept that other people help them in performing oral hygiene, and many times, they are not capable of performing all by themselves. It was also verified that the visual impaired person presents oral hygiene impairment causing some problems in tooth dentition and tooth loss. By starting the treatment at childhood, with proper and specialized treatment, the visual impaired person can perform her/himself hygiene and take care of her/himself oral health. Notwithstanding, it is known that prevention of both caries and periodontal disorders are toothbrushing and oral hygiene performed by the visual impaired individual. Thus, it can be concluded that the most effective technique for removing plaque and preventing oral diseases is proper toothbrushing and flossing 9.
In this context, the aim of this pilot study was to assess the Simplified Oral Hygiene Index (OHIS) and promote oral health educative activities as oral hygiene instruction and individually supervised toothbrushing in a group of visual impaired people for further verifying the effectiveness of these educative activities to change OHI-S. Moreover, the study also aimed to promote the social inclusion of the visual impaired individual not only by reeducation but also providing wellness and health.
Material and methods
Twenty-eight individuals of both genders, with visually impairment or poor eyesight, residents and/or enrolled at the Parana Institute for the Blind (IPC) participated in this pilot research. This institute is civil society organization located at Curitiba, Paraná, Brazil, created in 1939, which elaborated and develops its actions aiming at contributing with the social formation of blind and poor sight people.
The individuals received instruction about the research by reading aloud the Free and Clarified Consent Form. This term was signed by either the signature or fingerprint of each person who voluntarily accepted to participate in the study. Additionally, a person without visual impairment witnessed the reading of the term to assure that the read content matched that written within the document.
This study was conducted at three stages. At the first stage, the participants were invited to answer a questionnaire comprising questions on general and oral health and on habits such as smoking, oral health routine, previous dental treatments, among others. Because of the special characteristics of this study population, the questionnaire was individually applied by the responsible researchers integrally reading the questions and options and after recording the response reported by the subject. Next, the person performed toothbrushing with 1.500 ppm (parts per million) fluoride toothpaste and toothbrush with small head and soft bristles provided by the researches. Posteriorly, the disclosure of the biofilm was accomplished with the aid of disclosing solution and cotton swabs. Then, OHI-S was assessed 10. This index was measured through numbers from degree 0 to degree 3, as follows: degree 0 – absence of plaque or calculus; degree 1 – presence of plaque or calculus on up to 1/3 of tooth surface, degree 2 – presence of plaque or calculus on up to 2/3 of tooth surface; and degree 3 – presence of plaque or calculus on more than 2/3 of tooth surface. The qualitative criteria of this index range from 0 to 6 when debris and calculus sum can be classified as: excellent (0.0), good (0.1-1.2), regular (1.3-3.0) and weak (3.1-6.0). When only the bacterial plaque sum is counted, the classification is as follows: good (0.0 to 0.6), regular (0.7 to 1.8) and poor (1.9 to 3.0). Then, each patient was instructed to perform oral hygiene and supervised toothbrushing was carried out.
According to Rovida et al. 12, plaque indexes are useful and important for clinical evaluation of biofilm, both in researches for evaluation of products and in dental clinics, for monitoring patients, and for activities of hygiene instruction and toothbrushing techniques.
The second stage of the study was performed seven days after the first, after the oral hygiene instruction and OHI-S was again evaluated and analyzed whether there is or there is not an improvement in the index value.
The third stage was executed 30 days after the first one, and OHI-S was again evaluated to verify whether it changed. Bass modified toothbrushing technique was used for instructing the patients and further modifications could be executed because of the motor impairments of each patient.
Data regarding to gender, age, OHI-S values were recorded and tabulated in Microsoft Office Excel 2007 software, for posterior descriptive analysis.
This present study was submitted and approved by the Ethical Committee in Research of Positivo University under protocol number 269.928/2013.
Results
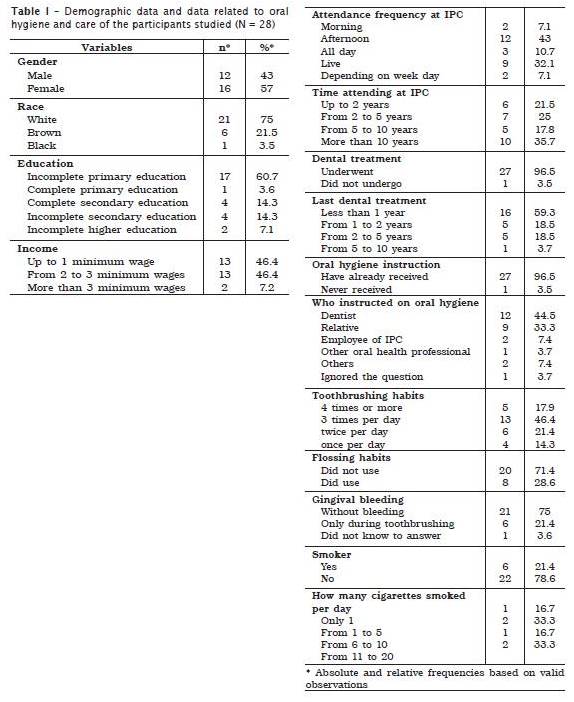
Table 1 displays the distribution of demographic data related to oral hygiene and care habits of the participants in absolute (N) and percentage (%) numbers.
Of the 28 individuals, 57% (16) were female and 43% (12) male. The age ranged from 14 to 75 years-old, with mean of 36.5 years. Twelve (43%) patients attended the institute at afternoon, nine (32.1%) lived at IPC, three stayed all day (10.7%), two attended at morning (7.1%), while the attendance frequency of two patients (7.1%) varied according to the week day.
Twenty-one patients were white (75%), six were brown (21.5%) and one was black (3.5%1).
Concerning to education level, 60.7% (17) had incomplete primary school, 14.3% (4) complete secondary school, 14.3% (4) incomplete secondary school, 7.1% (2) incomplete higher education and 3.6% (1) complete primary school. With regard to the family income, the values ranged from R$ 678.00 to R$ 3,000.00, with mean income of R$ 1,115.85.
Of all participants, 96.5% (27) reported to be submitted to dental treatment and only 3.5% (1) did not undergo any treatment. Concerning to the last dental treatment, 59.5% (16) reported it was within the past last year, 18.5% (5) from 1 to 2 years, 18.5% (5) from 2 to 5 years and 3.7% (1) from 5 to 10 years.
By asking about oral hygiene instruction, 96.5% (27) of the patients answered that they had already received some type of instruction, while 3.5% (1) never had been instructed. Of these, 96.5% affirmed that they had received instruction, 44.5% (12) claimed the instruction was given by a dentist, 33.3% (9) by a relative, 7.4% (2) by an employee of the institute, 3.7% (1) by other oral health professional, 7.4% (2) by other people and 3.7% (1) ignored the question.
Toothbrushing frequency was also questioned and the following results were observed: 46.4% (13) reported to brush three times per day, 21.4% (6) twice per day, 17.9% (5) four times or more per day and 14.3% (4) brushed only once per day.
With regard to flossing habits, 71.4% (20) of the patients reported that they did not floss, 14.3% (4) reported flossing once a day, 10.8% (3) three times per day and 3.5% (1) reported flossing twice per day.
Concerning to mouthrinses, 92.8% (26) did not use, 3.6% (1) had used fluoride mouthrinses once per day and 3.6% (1) did not know which solution, although they used it four times per day.
Twenty patients (75%) reported they did not present any gingival bleeding, six (21.4%) reported gingival bleeding occur during sometimes they performed toothbrushing and one (3.6%) did not know to answer.
Of all the participants, 78.6% (22) did not smoke and 21.4% (6) smoked. Of these latter, 33.3% (2) smoked from 1 to 5 cigarettes per day, 33.3% (2) from 11 to 20 cigarettes per day, 16.7% (1) smoked from 6 to 10 per day and 16.7% (1) answered to smoke only one cigarette per day.
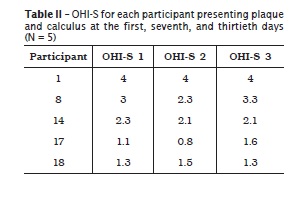
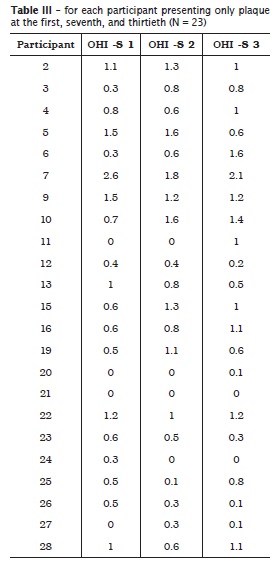
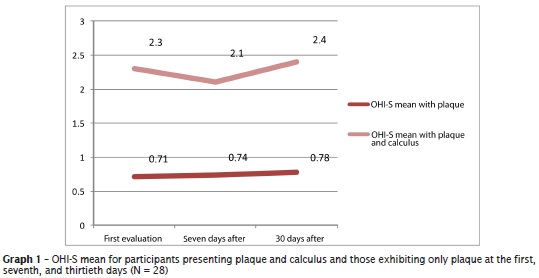
With regard to OHI-S, the mean values found at the first day before the educative activities was of 2.3, classified as regular, for the five participants evaluated with plaque and calculus index. For the 23 individuals presenting only plaque, the mean index value was of 0.71, classified as regular. Of the five participants classified with plaque and calculus index, 20% (1) showed good OHI-S, 60% (3) regular and 20% (1) weak. Of the 23 patients classified with only plaque index, 60.9% (14) exhibited good OHI-S, while 34.8% (8) showed regular OHI-S, and 4.3% (1) poor OHI-S. After the oral hygiene instruction and supervised toothbrushing, seven days after initial index evaluation, the mean was of 2.1 for plaque and calculus, classified as regular, and of 0.74 for only plaque, classified as regular. Of the five participants classified with plaque and calculus index at that period, 20% (1) showed good OHI-S, 60% (3) regular and 20% (1) weak. Of the 23 patients classified with only plaque index, 52.2% (12) exhibited good OHI-S and 47.8% (11) regular. And 30 days after the initial appointment and oral hygiene instruction, the mean of plaque and calculus index was of 2.4, classified as regular, and 0.78 for only plaque, classified as regular. Of the five participants classified with plaque and calculus index, 60% (3) showed regular OHI-S and 40% (2) weak. Of the 23 patients classified with only plaque index, 43.5% (10) exhibited good OHI-S, 52.2% (12) regular and 4.3% (1) poor.
In table 2, individual OHI-S at the first, seventh and thirtieth days can be verified for the group presenting calculus and plaque. Table 3 displays the same index values for the group exhibiting only plaque.
Graph 1 demonstrated the mean OHI-S at the first, seventh and thirtieth days, both for the participants exhibiting only plaque and those presenting plaque and calculus.
Discussion
This study showed that 96.5% (27) of the participants had been submitted to some type of dental treatment. This result was similar to that of the study of Souza Filho et al. 13. In the study of these authors, of 42 visual impaired participants, 95.2% (40) had already searched the dentist.
The toothbrushing of the individuals were evaluated through OHI-S from Green and Vermillion 10. At the first day, previously to oral hygiene instruction, the mean OHI-S for the five individuals showing plaque and calculus was of 2.3, classified as regular. After the instructions regarding to oral hygiene and supervised toothbrushing, they exhibited a discreet improvement in OHI-S mean, which decreased for 2.1, but still classified as regular. However, after a period of 30 days, mean OHI-S increased for 2.4, yet still classified as regular.
For the 23 participants showing only plaque, mean OHI-S at the first appointment was of 0.71, classified as regular. An increase of this mean OHI-S value was observed after seven days, with value of 0.74, still classified as regular. Notwithstanding, after 30 days, OHI -S was maintained as regular, because it exhibited a mean value of 0.78.
In this present study, of the 23 individuals showing plaque, 60.9% (14) had a good OHI-S, 34.8% (8) regular and 4.3% (1) poor. After seven days, 52.2% (12) exhibited good OHI-S and 47.8% (11) regular. And after 30 days, 43.5% (10) presented good OHI-S, 52.2% (12) regular and 4.3% (1) poor, demonstrating a decreasing of the number of participants having good OHI-S and increasing of those having regular OHI-S. Different values were found in the study of Cericato and Fernandes 7, in which 64.58% of the participants exhibited an inadequate toothbrushing and 35.42% showed adequate toothbrushing according to plaque control index.
In the study of Cericato and Lamha 8, 20.83% of the individuals performed toothbrushing twice a day and 70.83% more than twice a day, in agreement with this present research, which verified that 21.4% of the participants brushed their teeth twice a day and 64.3% three times or more per day.
Concerning the use of mouthrinses, 3.6% of these study participants reported they used fluoride mouthrinses, a value lower than that found by Cericato and Lamha (16.67%) 8.
According the results of the study of Cericato and Fernandes 7, it was verified that 33.33% had never received adequate oral hygiene instruction, 39.59% were instructed by a dentist, 16.67% by relatives and only 10.42% by the professor of the institution. These data disagrees from those of this present study: 44.5% were instructed by the dentist, 33.3% by a relative, 7.4% by an employee of the institution, 7.4% by others, 3.7% by other oral health professionals and 3,7% ignored the question.
Because patients with special needs have some limitations, they sometimes would be not capable of performing their own hygiene or they execute it inadequately, and the parents/guardians not only are concerned about oral health 2.
Although this present study did not evaluate oral health self-perception, it was noted that the participants living at the institution had a neglected oral hygiene self-perception. Unlikely, the participants studying at the same institution showed a more accurate self-perception, probably because the closest monitoring by the family, professor, and health professionals.
Considering the lack of scientific studies on this population of the Parana state, especially in the city of Curitiba, it is possible to use the results obtained in this present study to support further studies and stimulate the formulation of new public policies aiming to improve the instruction, stimulus, and consciousness of these patients regarding to oral health care, enabling the dentist to understand the universe of visually impaired people.
Conclusion
Based on the results obtained, it was possible to conclude that although OHI-S had shown a small reduction in the group presenting calculus and bacterial plaque seven days after oral hygiene instruction, the index value worsened after 30 days. In the group displaying only plaque, mean OHI-S value increased after seven and 30 days. It is worth emphasizing the necessity of promoting frequent activities of supervised toothbrushing, oral health instruction and motivation, providing wellness and health for visual impaired population.
Moreover, it is necessary to reconsider the State model that is capable of giving responses for the society. At a time when globalization is intense, barriers comprising prejudice and exclusion should be broken.
References
1. Abreu KCS, Perin PCP, Nunes NA, Prado VR, Constanzi S. Motivação de higiene bucal em deficientes visuais institucionalizados. Revista da Faculdade de Odontologia de Lins. 2005;17(1): 7-14. [ Links ]
2. Aguiar SMHCA, Barbieri CM, Louzada LPA, Saito TE. Eficiência de um programa para a educação e a motivação da higiene buco-dental direcionado a pacientes excepcionais com deficiência mental e disfunções motoras. Revista Faculdade de Odontologia de Lins. 2000;12(1-2):16-23.
3. Braga EC, Sinatra LS, Carvalho DR, Cruvinel VR, Miranda AF, Montenegro FLB. Intervenção odontológica domiciliar em paciente idoso cego institucionalizado: relato de caso. Revista Paulista de Odontologia. 2011;33(2):17-22.
4. Brasil. Decreto n. 5.296. Regulamenta as leis n. 10.048, de 8 de novembro de 2000, e n. 10.098, de 19 de dezembro de 2000, e dá outras providências. Diário Oficial da União; 2004.
5. Brasil. Ministério do Planejamento, Orçamento e Gestão. Instituto Brasileiro de Geografia e Estatística. Censo Demográfico 2010. Características gerais da população, religião, e pessoas com deficiências. Available from: URL:ftp://ftp.ibge.gov.br/Censos/Censo_Demografico_2010/Caracteristicas_Gerais_Religiao_Deficiencia/caracteristicas_religiao_deficiencia.pdf.
6. Carvalho ML, Silva FML, Barbosa FQ, Duarte FB, Barbosa KB, Figueiredo V et al. Deficiente? Quem? Cirurgiões dentistas ou pacientes com necessidades especiais? Revista em Extensão. 2004;4(1):65-71.
7. Cericato GO, Fernandes APS. Implicações da deficiência visual na capacidade de controle de placa bacteriana e na perda dental. Revista da Faculdade de Odontologia. 2008;13(2):17-21.
8. Cericato GO, Lamha APSF. Hábitos de saúde bucal de portadores de deficiência visual no contexto da saúde coletiva. Revista da Faculdade de Odontologia. 2012;17(2):137-44.
9. Costa FS, Neves LB, Bonow MLM, Azevedo MS, Schardosim LR. Efetividade de uma estratégia educacional em saúde bucal aplicada a crianças deficientes visuais. Revista da Faculdade de Odontologia. 2012;17(1):12-7.
10. Green JC, Vermillion JR. The simplified oral hygiene index. J Am Dent Assoc. 1964;68:7-13.
11. Povoa CA, Nicolela MT, Valle ALSL, Gomes LES, Neustein I. Prevalência de glaucoma identificada em campanha de detecção em São Paulo. Arq Bras Oftalmol. 2001;64(4):303-7.
12. Rovida TAS, Moimaz SAS, Arcieri RM, Garbin CAS, Lima DP. Controle da placa bacteriana dentária e suas formas de registro. Revista Odontológica de Araçatuba. 2010;31(2):57-62.
13. Souza Filho MD, Nogueira SDM, Martins MCC. Avaliação da saúde bucal de deficientes visuais em Teresina – PI. Arquivos de Odontologia. 2010;46(2):66-74.
14. Souza IR, Caldas CP. Atendimento domiciliário gerontológico: contribuições para o cuidado do idoso na comunidade. Revista Brasileira de Pesquisa em Saúde. 2008;21(1):61-8.
 Corresponding author:
Corresponding author:
Juliana Yassue Barbosa da Silva
Universidade Positivo
Rua Professor Pedro Viriato Parigot de Souza, n. 5.300 – Campo Comprido
CEP 81280-330 – Curitiba – PR – Brasil
E-mail: julianayassue@up.com.br
Received for publication: November 7, 2013
Accepted for publication: December 12, 2013













