Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.11 no.2 Joinville Abr./Jun. 2014
Case Report Article
Aesthetic management of molar-incisor hypomineralization
Juliana Feltrin de Souza I; Camila Maria Bullio Fragelli II; Manuel Restrepo II; Amanda Mahammad Mushashe I; Estela Maris Losso I; Leonardo Fernandes da Cunha I
I Master Program in Clinical Dentistry, Positivo University – Curitiba – PR – Brazil
II São Paulo State University, School of Dentistry of Araraquara, Department of Child Clinics – Araraquara – SP – Brazil
ABSTRACT
Introduction: Molar-incisor hypomineralization (MIH) has been challenging for clinical practice. The term refers to an enamel defect that affects permanent molars and often permanent incisors. This defect may result in high sensibility, coronal destruction of the molars, aesthetic problem when incisors are affected, which can jeopardize the child`s emotional and psychological development. Objective: The aim of this paper is to report two cases in which a conservative approach was adopted using new technologies for direct restorative treatment of incisor with MIH opacities. Case report: Patients aged 11 and 12 years-old attended to the clinics of the School of Dentistry (Sao Paulo State University – Unesp) complaining about the appearance of incisors due to the presence of opacities on the labial surface. The cases were diagnosed as MIH, presenting enamel defects on the permanent molars and incisors. Direct restorations were carried out with minimal removal of the opacities using CVD diamond tip (CVDentus, São José dos Campos, São Paulo, Brazil) coupled to an ultrasonic device (CVDentus, São José dos Campos, São Paulo, Brazil) and direct restorations with composite resin. The result of the restorative treatment was satisfactory in both cases, with children showing immediate satisfaction. Conclusion: The incisors affected by MIH should be treated to improve the child`s self-esteem and avoid negative effects on their psychology development. The aesthetic treatment of the incisors should be conservative, since the replacements of restorations are needed throughout life.
Keywords: dental enamel hypoplasia; children; aesthetics; dental aesthetics.
Introduction
The enamel alteration so-called molar-incisor hypomineralization (MIH) is currently one of the most challenging problem of pediatric dentistry clinics 23. Studies have reported a considerable prevalence in Brazilian communities ranging from 12% to 40% 6,15.
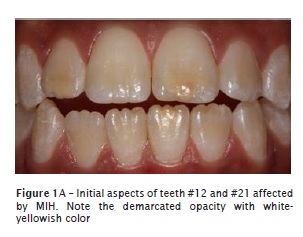
This defect affects the permanent first molars and can be associated with permanent incisors 14. The enamel affect by MIH exhibits opacities varying from white to yellow-brownish with well-defined edges of the normal enamel. Most severe cases show loss of enamel structure, favoring sensitivity and the fast development of caries lesions 11,15,18,21. The asymmetry of this alteration suggests that the ameloblasts are affected by systemic or environmental factors during amelogenesis 1,2. Among the possible causes, respiratory problems, complications at the pre-natal period, low weight at birth, metabolic calcium and phosphate disorder, and childhood diseases associated with high fever have been considered 1,3,4,13,17,19,24.
Microscopically, the affected enamel is porous, with smaller inorganic content and enamel prism disorganization and consequently the mechanical properties are reduced 7,8. The most severe cases present enamel structure loss and the masticatory forces expose the dentin favoring sensitivity and the fast development of caries lesions 10,15,21,22, a situation requiring restorative treatment.
Because of the structural alterations, teeth affected by MIH have shown difficulty of bonding to restorative materials, thus demanding recurrent treatments 12. Because the treatment of molars is challenging, the dentist frequently neglects the management of the incisors, normally affected by opacities. However, the aesthetical appearance may result in negative effects on the psychological and emotional development of the child leading to implications on social interaction 20. Therefore, the treatment of incisors affected by this hypoplasia is also a challenge for the dentist. The aim of this study was to report two clinical cases of MIH in incisors and discuss the conservative restorative management for this alteration.
Case reports
Case 1
Patient N.A.U., female, 12 years-old, has been followed-up since 9 years of age at the Pediatric Dentistry Clinics of the School of Dentistry of – Araraquara (Unesp) because of MIH. At initial evaluation, only the posterior teeth affected by MIH were included in treatment planning. During 3 years, the opacities and atypical restorations of the molars were followed-up aiming to reduce sensitivity and preserve the sound and affected tooth structure. The complaint about the incisor opacities occurred around 11 years of age, when both the child and the parents reported dissatisfaction about the opacities. Clearly, the aesthetical appearance of the anterior teeth was affecting the development of the child who was more shy and introspective at every appointment.
A conservative restorative treatment was chosen to manage the white-yellowish opacities on teeth #21, #12 and #31, after the evaluation of the emotional and psychological impact of the opacities in the child.
Conservative treatment of teeth #21 and #12 comprised a minimally invasive superficial wear on the opacities followed by the restoration with microparticle resin composite (Point 4 – Kerr).
Firstly, an interpapi l lary anesthesia in permanent canines with 3% mepivacaine was carried out followed by rubber dam isolation with the aid of clamps. The removal of the superficial portion of the opacity was obtained with the aid of CVD T1 diamond tip (CVDentus, São José dos Campos, São Paulo, Brazil). Next, phosphoric acid etching was executed and adhesive system was applied (Optibond FL, Kerr) according to the manufacturers' instructions. Shade A2 (enamel) resin composite restoration (Point 4, Kerr) was inserted at increments. Finishing and polishing procedure was accomplished with the aid of discs (Super Tray, Kerr).
The result was satisfactory for both the child and the parents.

Case 2
Patient C.G.M., male, 11 years-old, sought the Pediatric Dentistry Clinics of the School of Dentistry of Araraquara (Unesp) with his parents complaining about the lack of aesthetic of anterior teeth. At clinical examination, MIH was diagnosed in teeth #16, #26, #36 and #11. Teeth #26 and #16 had yellow-brownish opacities, without structural loss. Tooth #36 had already been restored with an atypical resin composite. It was also observed a white-yellowish opacity on tooth #11, which triggered the aesthetic complaint. According to the parents, the child dissatisfaction started after school bullying during the past 3 months.
Both the child and the parents were instructed in relation to the steps of direct restorative treatment. Although the tooth structure was sound, the child exhibited social life sequelae so that the restorative treatment was chosen. The conservative treatment comprised the superficial removal followed by aesthetic restoration of tooth #11.
Prior to restorative technique, a topical anesthesia was performed with Emla followed by rubber dam isolation with the aid of ligations. Then the superficial portion of the opacity was removed with the aid of CVD T1 diamond tip (CVDentus, São José dos Campos, São Paulo, Brazil) followed by 37% phosphoric acid etching, application of the adhesive system (Optbond S, Kerr), according with the manufacturer's instructions, and resin composite (Premisa, Kerr A1 dentin and A1 enamel shades) inserted at increments. Finishing and polishing procedures were accomplished with the aid of discs (Super Tray – Kerr).
Restorative treatment outcome was satisfactory demonstrated by the immediate satisfaction of the child.


Discussion
Dentists, especially pediatric ones have faced MIH comprising alterations ranging from demarcated opacities to enamel fracture, resulting in larges coronal destructions 21. These teeth have raised special attention because of sensitivity complaints, aesthetical involvement, and repeated treatment demands 12,16.
In literature, the treatments proposed for affected molars vary according to the severity observed. Teeth affected by opacities have been treated with the use of either fluoride varnish or sealants, while teeth exhibiting structure loss have been restored with glass ionomer cement or resin composite, crowns, or extractions followed by orthodontic treatment 16. In the cases reported herein, resin composite restoration was chosen. Respectively, microparticle and nano-hybrid composites were applied. Da Costa et al. 5 reported that resins with smaller particles, such the ones employed in the present cases, exhibited less brightness loss and superficial roughness increase. Moreover, Furuse et al. 9 also reporting a clinical case of enamel hypoplasia, affirmed that whenever possible, a more conservative approach should be opted. Considering the age of the patients and consequently the further need of replacement of these restorations, more conservative preparations were carried out. Thus, the opacity of the alteration was only reduced, but tooth structure was maintained for further replacement of the restorations.
Although the occurrence of defects on incisors is smaller than those on molars 10 and the incisor enamel rarely undergoes structural loss 21, pediatric dentists should be aware of the psychosocial impacts of the disease. The appearance of the anterior teeth may result in an unfavorable self-image for the child and jeopardize the social interaction. Dissatisfaction related to the smile is common, normally followed by school bullying and interaction with other children.
One ought to understand all MIH aspects and comprehensively consider the child to measure the impact of MIH in the child's life by comparing it to the clinical sequelae of an early restorative treatment.
The conservative management of the treatment is necessary because of the child's age and opacity extension, which frequently affects all enamel thickness. This is an early treatment, so that one should consider the pulp chamber size and the preparation must be limited to the enamel. Although the amount of wear does not provide an aesthetic restoration covering all opacity, at a conversation distance such alteration cannot be perceived.
Conclusion
In summary, the child affected by MIH should be comprehensively treated so that the emotionally and psychological development are not negativelyaffected. The aesthetical aspects of the alterations of incisors should be observed and whenever necessary treated through conservative approaches.
References
1. Alaluusua S. Aetiology of molar-incisor hypomineralisation: a systematic review. European Archives of Paediatric Dentistry. 2010;11:53-8. [ Links ]
2. Alaluusua S, Lukinmaa PL, Koskimies M, Pirinen S, Holtta P, Kallio M et al. Developmental dental defects associated with long breast feeding. European Journal of Oral Sciences. 1996;104:493-7.
3. Arrow P. Risk factors in the occurrence of enamel defects of the first permanent molars among schoolchildren in Western Australia. Community Dentistry and Oral Epidemiology. 2009;37:405-15.
4. Crombie FA, Manton DJ, Weerheijm KL, Kilpatrick NM. Molar incisor hypomineralization: a survey of members of the Australian and New Zealand Society of Paediatric Dentistry. Australian Dental Journal. 2008;53:160-6.
5. Da Costa J, Adams-Belusko A, Riley K, Ferracane JL. The effect of various dentifrices on surface roughness and gloss of resin composites. Journal Dentistry. 2010;38.
6. Da Costa-Silva CM, Jeremias F, de Souza JF, Cordeiro R de C, Santos-Pinto L, Zuanon AC. Molar incisor hypomineralization: prevalence, severity and clinical consequences in Brazilian children. International Journal of Paediatric Dentistry / British Paedodontic Society / International Association of Dentistry for Children. 2010;20: 426-34.
7. Fagrell TG, Dietz W, Jalevik B, Noren JG. Chemical, mechanical and morphological properties of hypomineralized enamel of permanent first molars. Acta Odontologica Scandinavica. 2010;68:215-22.
8. Fearne J, Anderson P, Davis GR. 3D X-ray microscopic study of the extent of variations in enamel density in first permanent molars with idiopathic enamel hypomineralisation. British Dental Journal. 2004;196:634-8/discussion 25.
9. Furuse AY, Cunha LF, Valeretto TM, Mondelli RFL, Mondelli J. Tratamentos conservadores por meio de microabrasão do esmalte. Revista Dental Press de Estética. 2007;4.
10. Jalevik B. Enamel hypomineralization in permanent first molars. A clinical, histo-morphological and biochemical study. Swedish Dental Journal Supplement. 2001;(149):1-86.
11. Jalevik B, Klingberg G. Treatment outcomes and dental anxiety in 18-year-olds with MIH, comparisons with healthy controls – a longitudinal study. International Journal of Paediatric Dentistry / British Paedodontic Society / International Association of Dentistry for Children. 2012;22: 85-91.
12. Jalevik B, Klingberg GA. Dental treatment, dental fear and behaviour management problems in children with severe enamel hypomineralization of their permanent first molars. International Journal of Paediatric Dentistry / British Paedodontic Society / International Association of Dentistry for Children. 2002;12:24-32.
13. Jalevik B, Noren JG. Enamel hypomineralization of permanent first molars: a morphological study and survey of possible aetiological factors. International Journal of Paediatric Dentistry / British Paedodontic Society / International Association of Dentistry for Children. 2000;10: 278-89.
14. Jalevik B, Odelius H, Dietz W, Noren J. Secondary ion mass spectrometry and X-ray microanalysis of hypomineralized enamel in human permanent first molars. Archives of Oral Biology. 2001;46:239-47.
15. Jeremias F, de Souza JF, Silva CM, Cordeiro R de C, Zuanon AC, Santos-Pinto L. Dental caries experience and molar-incisor hypomineralization. Acta Odontologica Scandinavica. 2013;71:870-6.
16. Lygidakis NA, Wong F, Jalevik B, Vierrou AM, Alaluusua S, Espelid I. Best clinical practice guidance for clinicians dealing with children presenting with molar-incisor-hypomineralisation (MIH): an EAPD Policy Document. European Archives of Paediatric Dentistry. 2010;11:75-81.
17. Souza JF, Costa-Silva CM, Jeremias F, Santos-Pinto L, Zuanon AC, Cordeiro RC. Molar incisor hypomineralisation: possible aetiological factors in children from urban and rural areas. European Archives of Paediatric Dentistry. 2012;13:164-70.
18. Souza JF, Jeremias F, Costa Silva CM, Santos-Pinto L, Zuanon AC, Cordeiro R de C. Hipomineralización incisivo y molar: diagnóstico diferencial. Acta Odontol Venezolana. 2011;49: 1-8.
19. Souza JF, Jeremias F, Costa-Silva CM, Santos-Pinto L, Zuanon AC, Cordeiro R de C. Aetiology of molar-incisor hypomineralisation (MIH) in Brazilian children. European Archives of Paediatric Dentistry. 2013.
20. Vargas-Ferreira F, Ardenghi TM. Developmental enamel defects and their impact on child oral health-related quality of life. Braz Oral Res. 2011;25:531-7.
21. Weerheijm KL. Molar incisor hypomineralization (MIH): clinical presentation, aetiology and management. Dental Update. 2004;31:9-12.
22. Weerheijm KL, Duggal M, Mejare I, Papagiannoulis L, Koch G, Martens LC et al. Judgement criteria for molar incisor hypomineralisation (MIH) in epidemiologic studies: a summary of the European meeting on MIH held in Athens, 2003. European Journal of Paediatric Dentistry. 2003;4:110-3.
23. Weerheijm KL, Jalevik B, Alaluusua S. Molar-incisor hypomineralisation. Caries Research. 2001;35:390-1.
24. Whatling R, Fearne JM. Molar incisor hypomineralization: a study of aetiological factors in a group of UK children. International Journal of Paediatric Dentistry / British Paedodontic Society / International Association of Dentistry for Children. 2008;18:155-62.
 Corresponding author:
Corresponding author:
Juliana Feltrin de Souza
Universidade Positivo
Rua Professor Pedro Viriato Parigot de Souza, n. 5.300 – Campo Comprido
CEP 81280-330 – Curitiba – PR – Brasil
E-mail: julianafeltrin@hotmail.com
Received for publication: September 12, 2013
Accepted for publication: November 11, 2013













