Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.11 no.3 Joinville Jul./Set. 2014
ORIGINAL RESEARCH ARTICLE
Profile of temporomandibular disorder patients submitted to dental and physiotherapeutic treatment at a private clinic
Mariana Lima Fernandes I; Lídia Audrey Rocha Valadas Marques II; Edilson Martins Rodrigues Neto I; Mara Assef Leitão Lotif II; Francisca Helvira Cavalcante Melo I; Raimunda Hermelinda Maia Macena III
I Department of Physiology and Pharmacology, Federal University of Ceará – Fortaleza – CE – Brazil
II Department of Dental Clinics, Federal University of Ceará – Fortaleza – CE – Brazil
III Department of Physiotherapy, Integrated School of Ceará – Fortaleza – CE – Brazil
ABSTRACT
Introduction: Temporomandibular disorder (TMD) is the term used in Dentistry to define the structural and disorder changes affect the physiology of the masticatory system composed of TMJ and related to musculoskeletal structures. Objective: To conduct a descriptive, transversal and documentary study aiming to determine the profile of 14 TMD patients undergoing simultaneous dental and physiotherapeutic treatment at a private practice of the city of Fortaleza-Ce. Material and methods: The following instruments for the collection of the data were employed: files registering the evaluation and evolution, findings of the radiographic examinations and forms. Data were statistically analyzed through SPSS software, version 10.0. Results: Most of the sample was composed by females aged 32 years (+/-10.60) in average, mainly complaining about chronic headache, masticatory myalgia , TMJ pain, cervicalgy, otalgia, among others. The complete sample presented, at least, one pathology associated to and/or concomitant to TMD. The radiographic findings showed TMJ alterations and tooth losses. Analgesics were the most used drugs. Conclusion: TMD is a complex syndrome, with many etiologies and symptoms, aggravating and perpetuating factors, requiring multiple and even more specialized therapeutic management attempting treatment success.
Keywords: temporomandibular joint disorders; etiology; physiotherapy.
Introduction
Temporomandibular joint (TMJ) comprises the stomatognathic system and has been classified as bilateral, interdependent, synovial, and thus enables simultaneous large mandibular around temporal bone, a fixed bone 8.
Temporomandibular disorder (TMD) is the term in Dentistry used to define structural alteration and disorders affecting masticatory system physiology, composed by TMJ and related muscle-skeletal structures 10.
TMD etiology is considered as multifactorial, that is, generally caused by the relationship among the neuromuscular, occlusal and physiopathological factors of TMJs. Infectious and inf lammatory diseases, hormonal and vitamin deficiencies may affect TMJ physiology. Also, TMD may be related to the increasing of patient's emotional stress level that may induce the increasing of muscular tonus, frequently associated with the presence of parafunctional habits, such tooth clenching, resulting in fatigue and spasm producing pain and dysfunction 8,9,10.
Among TMD characteristics signs and symptoms, articular noises and crepitus, tinnitus, headaches, mandibular movement limitations or deviations, myalgias, ear pain, sensit ivity to palpat ion, stomatognathic system pains, and in mostly severe cases luxations are seen 8,12,14.
Mainly pain can negatively inf luences on the patients' social activities thus affecting the emotional health. Accordingly, TMD etiology and symptomatology should be verified during anamnesis and require a multidisciplinary team, involving dentists, neurologists, orthopedists, otolaryngologists, physiotherapists, speech and hearing therapists, among others 1.
The aim of this study was to verify the profile of TMD patients simultaneously submitted to dental and physiotherapeutic treatment at a private practice in the city of Fortaleza (CE/Brazil).
The knowledge of TMD patients would guide Physiotherapists towards indicating therapeutic strategies considering not only the symptomatology but also the pathologic factors seen on radiographic examinations, which would greatly contribute to patient's satisfaction and conversation among the multidisciplinary team involved in the treatment of this pathology searching for more therapeutic effectiveness.
Material and methods
A descriptive, cross sectional, documentary, quantitative study was conducted. Study data were collected from TMD patients. The study sample was treated through a therapeutic approach including Dentistry and Physiotherapy simultaneously at a private practice in the city of Fortaleza (CE/Brazil). The private office team was composed of six dentists and one physiotherapist offering services of esthetic dentistry, orthodontics, TMD treatment with the association with physiotherapy.
Also, the type of drugs used by patients during TMD treatment was also researched. Moreover, we attempted to find on radiographic examinations the presence of previous and/or concomitant pathologies.
Inclusion criteria comprised both genders; presence of TMD; simultaneous dental and physiotherapeutic treatment, with at least five dental and five physiotherapeutic appointments; files of patients composed of the evolution progress and radiographic examinations. Exclusion criteria were composed by execution of just one treatment type, either dental or physiotherapeutic. Fourteen patients met the inclusion and exclusion criteria.
Data collection was obtained through analyzing the physiotherapeutic evaluation progress and radiographic examinat ions of the pat ient s (panoramic radiographs and TMJ radiographs), followed by registering the data on specific charts. Statistical analysis was performed with SPSS software version 10.0.
This study followed the ethical aspects stated by the Resolution 196/96 of Brazilian Council of Health. Firstly, the main examiner signed a term to assure that all data would be only used for scientific purposes. All office's owners signed a consent form authorizing the data collection for the study.
Results and discussion
All 14 patients were diagnosed with TMD. Table 1 shows patients' characterizes.
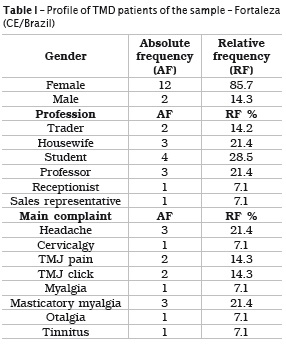
In this present study, most of patients searching treatment were females aged from 13 to 49 years (mean age of 32 years). Studies have pointed out that most TMD cases affect women at age range of 20-50 years, because women exhibits a greater TMJ ligament flexibility than men, resulting in more fragile articular disk, more vulnerable to damage 5,6.
By analyzing patient's profession, no statistically significant differences were found by Chi-square test. Conversely, some studies have reported that some activities may increase emotional stress requiring greater physical and mental effort.
Patient's main complaint is an important parameter because allowed individualized care. Most of the main complaints in this present study were headache (21.4%) and masticatory myalgia (21.4%), followed by TMJ pain (14.3%) and TMJ clicking (14.3%). Other main complaints were cervicalgy, otalgia and tinnitus.
Studies on the detection of TMDs' signs and symptoms have found: pain and sensitiveness on masticatory muscles; TMJ pain and noises; and mandibular limitations of or disturbs 6,7.
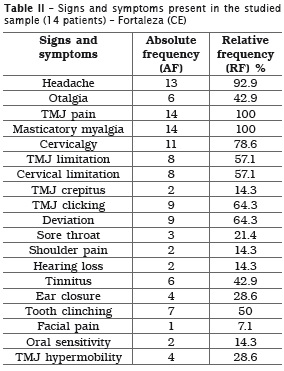
B y c omp r e h e n s i v e l y a n a l y z i n g a l l symptomatology showed in this presented study (table 2), masticatory myalgia and TMJ pain were presented in all patients; also, 92.9% of the sample had headaches.
Most of patients exhibited cervicalgy (78.6%) and some individuals showed limitation in the amplitude of cervical spine movements (57.1%), and articular and muscular pain in shoulder (14.3%). If these aforementioned areas presented muscular-skeletal imbalance, either spasms or disc displacement would be generated in the mandible, result in pain that can reach up to the cervical spine, shoulders and head. Postural dysfunction may alter other body's structures which may affect TMJ structure and functionality 6.
TMJ noises were described as crepitus and (14.3%) and clicking (64.3%). Patients exhibiting TMJ clicking had deviation of mandibular movements (64.3%). Of these, most had TMJ radiographic examinations showing symmetric mandibular condyles and articular tubercle. Chi-square test did not find statistically significant differences in the association main complaints with the radiographic findings.
Mandibular movement disturbs were limitation or hypomobility (57.1%) and hypermobility (28.8%). Articular dysfunctions may occur together with either hypermobility, that is, when the mandibular condyle surpass the articular tubercle during mandibular movements; or hypomobility, that is caused by limited mandibular opening or closure; or still with condyle asymmetry in which anterior disc displacement occurs resulting in clinical mandibular opening reduction towards the affected side 6,11.
In 21.4% of the patients, sore throat was referred together with swallowing difficulty. These patients showed limitation of cervical spine movements with calcification and/or elongation of stylohyoid ligament in the radiographic examinations. According to the literature, these findings met the description of Eagle's syndrome, which is a symptomatic complex caused by stylohyoid ligament calcification resulting in frequent sore throat and earache. This can be easily seen on radiographs 13.
Signs and symptoms of ear injury were presented as hearing loss (14.3%); feeling of ear closure (28.6%); otalgia (42.9%); and tinnitus (42.9%). Many hearing symptoms may be present in TMD, including hearing impairment, tinnitus, otalgia and dizziness. Such symptoms may be related to the close anatomical and ontogenetic relationship between middle ear and masticatory structures 9.
Half of the patients showed tooth clinching (50%). The rationale behind this finding is that some muscles have single characteristics from the context of muscular dysfunction. Both temporal and masseter muscles are closely related to headaches because of muscle contraction. This is a very common symptom in patients with muscle dysfunction, together with pain sites in the presence of parafunction due to tooth clinching. TMD is a disorder generally associated with stress, which induces the increasing of muscle tonus frequently associated with parafunctional habits, such as tooth clinching, resulting in fatigue and spasms, which result in pain and dysfunction 2,12,13.
In 14.3% of the patients, tooth sensitivity was altered. Of these, one patient (7.1%) also showed unilateral facial stabbing pain (piercing and burning), with duration of seconds. TMD patient may present severe, acute or pulsatile pain; pain with variable intensity in mandible or pre-auricular region; burning sensation on tongue and mouth; pain in face or cheek; muscle fatigue; neural piercing pain and frequent headaches. These different pain types may be related to both the receptors and tissues involved, suppressive and excitatory mechanisms of nervous system that can modulate pain perception 9.
In the analysis of the associated pathologies, TMD signs and symptoms can be verified.
TMD also have disturbs coming from a primary pathological condition of the structural and functional components of masticatory system. The harmony between structural and functional components is maintained at good health condition 4.
Direct and indirect traumas to TMJ, parafunctional habits, skeletal, oclusal, systemic/ local alterations, and psychosocial questions can be associated, altering the functional balance of the stomatognathic system towards pathological dysfunction 10.
Most of patients had oclusal problems and tooth losses, mainly pre-molars and molars. TMD etiologies may comprise: oral and maxillofacial and cervical spine traumas; oclusal interferences (posterior and anterior tooth contacts) due to inappropriate restorations, which may interfere on normal function causing bruxism and tooth clinching, etc.; among others. Factors as malocclusion, loss of overbite due to weariness or tooth losses; hypoplasic mandible; and some systemic disturbs (allergy, osteoarthritis, hormonal disturbs, neuropathy, neoplasia, polyarthritis, among others) may affect TMJ 9,11.
This present study detected that approximately 43% of the patient reported anxiety. This showed that emotional problems may lead to an excessive increasing of jaw's muscular activities, causing more problems on masseter, which can also be involved in malocclusions 15.
Studies on pain evolution have suggested that gradual development occurs with fluctuations over time, aggravated by mandibular movements and influenced by psychological factors associated to social-cultural level and the past pain experiences. Continue hypernociception may contribute to aggravate TMD because the patient becomes more depressive and sensible to psychological alterations 3,15.
The pharmacological approach of TMDs comprises analgesics indicated alone or together with drugs to treat the signs and symptoms of the associated and/or concomitant pathologies. Generally, analgesics are prescribed but self-medication is not rare. Analgesics, anti-inflammatory drugs, muscle relaxant drugs, and other drugs to stabilize the pathological conditions have been largely employed. At initial TMD phase, patients respond well to analgesics and muscular relaxants. These latter act on muscles by relieving the fatigue and trismus and decreasing the tendency towards clinching because the muscles become less spastic. Some studies have suggested the use of amitriptyline (tricyclic antidepressant) because of action on general anxiety and sedative pharmacological properties 3,4,6.
Conclusion
It can be concluded that most of patients were female aged in average 32 years (+/- 10.60). The main complaints were: TMJ pain, masticatory myalgia, headache, cervicalgy, otalgia and alteration in mandibular movements. Most of radiographic examinations showed alterations in the condyle symmetry, shape and location at maximum opening. Also, most patients showed loss of pre-molars and molars. All patients reported during anamnesis at least one past or concomitant pathology which may possible influence on TMD.
Analgesics were largely employed because pain manifests differently and is the main TMD symptom. This present studies seem to reaffirm that TMD is a complex syndrome involving primary and secondary etiologies with perpetuating and aggravating factors, large symptomatology and compromising several structures. Accordingly, multidisciplinary treatment is required attempting treatment success.
References
1. Bevilaqui-Grossi D, Chaves TC, Oliveira AS, Monteiro-Pedro V. Anamnestic index severity and signs and symptons of DTM. J Craniomand Pract. 2006;24(2):112-20. [ Links ]
2. Branco RS, Branco CS, Tesch RS, Rapoport A. A freqüência de relatos de parafunções nos subgrupos diagnósticos de DTM de acordo com os critérios diagnósticos para pesquisa em disfunções temporomandibulares (RDC/TMD). Rev Dental Press Ortodon Ortop Facial. 2008;13(2):61-9.
3. Calderon OS, Merighi ML, Oliveira LC, Camargo APA, Ramos Netto TC, Conti PCR. Effectiveness of cognitive-behavioral therapy and amitriptyline in patients with chronic temporomandibular disorders: a pilot study. B Dent J. 2011;22(5):415- 21.
4. Carrara SV, Conti PCR, Barbosa JS. Termo do 1.º Consenso em Disfunção Temporomandibular e Dor Orofacial. Dental Press J Orthod. 2010; 15(3):114-20.
5. Carvalho CM, de Lacerda JA, dos Santos Neto FP, Cangussu MC, Marques AM, Pinheiro AL. Wavelength effect in temporomandibular joint pain: a clinical experience. Lasers Med Sci. 2010;25(2):229-32.
6. Cohen WA, Servais JM, Polur I, Li Y, Xu L. Articular cartilage degeneration in the contralateral non-surgical temporomandibular joint in mice with a unilateral partial discectomy. J Oral Pathol Med. 2014;43(2):162-5.
7. Machado E, Machado P, Cunali PA, Grehs RA. Ortodontia como fator de risco para disfunções temporomandibulares: uma revisão sistemática. Dental Press J Orthod. 2010;15(6):54-5.
8. Madeira MC. Bases anatomofuncionais para a prática odontológica. 6. ed. São Paulo: Sarvier; 2008. p. 40-59.
9. Nelson SJ, Ash MM. Wheeler – Anatomia dental, fisiologia e oclusão. 9. ed. São Paulo: Elsevier; 2012. p. 120-33.
10. Okenson JP. Tratamento das desordens temporomandibulares e oclusão. 6. ed. São Paulo: Elsevier; 2008. p. 70-98.
11. Pasinato F, Souza JA, Correa ECR, Silva AMT. Temporomandibular disorder and generalized joint hypermobility: application of diagnostic criteria. Braz J Otorhinolaryngol. 2011;77(4):418-25.
12. Proffit WR, Phillips C, Turvey TA. Stability after mandibular setback: mandible-only versus 2-jaw surgery. J Oral Maxillofac Surg. 2012;70(7): 408-14.
13. Ro-Renzi G, Mastellone P, Leonardi A, Becelli R, Bonamini M, Fini G. Basicranium malformation with anterior dislocation of right styloid process causing stylalgia. J Craniofac Surg. 2005;16(1):418-20.
14. Santos TS, Piva MR, Ribeiro MH, Antunes AA, Melo AR, Silva EDO. Lasertherapy efficacy in temporomandibular disorders: control study. Braz J Otorhinolaryngol. 2010;76(3):294-9.
15. Zöger S, Svedlund J, Holgers KM. Relationship between tinnitus severity and psychiatric disorders. Psychosomatics. 2006;47(1):282-8.
 Corresponding author:
Corresponding author:
Lídia Audrey Rocha Valadas Marques
Rua Carlos Vasconcelos, 1.338 – ap. 502
CEP 60115-170 – Fortaleza – CE – Brasil
E-mail: lidiavaladas@gmail.com
Received for publication: November 7, 2013
Accepted for publication: May 14, 2014













