Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.11 no.3 Joinville Jul./Set. 2014
Literature Review Article
Systemic medication applied to endodontic treatment: a literature review
Nanete de Menezes Silva I; Domingos Alves dos Anjos Neto II
I Department of Dentistry, Tiradentes University – Aracaju – SE – Brazil
II Department of Endodontics, Tiradentes University – Aracaju – SE – Brazil
ABSTRACT
Introduction: A problem of endodontic origin is solved mainly by cleaning and disinfecting the root canal system. However, the use of medicines for systemic use is a great auxiliary in combating pain, inflammation and/or infection, making easier to treat the clinical status, that patient experiences less pain. Objective: To conduct a literature review evidencing the clinical indications of systemic medication application in endodontics, to aid the professional in achieving more effective and safer therapeutics. Literature review: There is a wide variety of drugs available on market. Consequently, the dentist is uncertain when prescribing systemic medication because a pharmacological arsenal is available. Also, the dentist frequently does not know the mechanism of action of these drugs and their interactions. Additionally to analgesics, anti-inflammatories and antibiotics, used to combat pain, inflammation and infection, respectively, dentists can still make use of anxiolytics, in cases of patients very fearful to endodontic treatment. Conclusion: It is of fundamental importance that the dentist knows about the medication type to be used in each case and whether systemic therapy is really necessary, through a comprehensive case evaluation.
Keywords: systemic medication; endodontic treatment; acute dentoalveolar abscess.
Introduction
From manufacturing to consumption, many studies are concerned about medicines worldwide. Many of them aimed medical practice, emphasizing issues regarding adverse side effects, increasing and dissemination of bacterial resistance to antibiotics, pattern of medicine prescription and influence of medicine advertising on prescription 3.
Although endodontic treatment should be view from a surgical perspective, because local therapy must be firstly instituted, many clinical situations require the use of systemic drugs to act on problems coming from the treatment sequence, such as: inflammatory reaction, pain, and infection that provide more comfort and safety to patient 5.
In medicine, many drugs display analgesic, antiinflammatory, and antimicrobial action. Depending on the clinical signs and symptoms and on the pharmacological effect desired, the professional can choose among a variety of drugs 24.
According to Leonardo and Leal (1998) 10, the cornerstone of endodontic treatment auxiliary therapy is the correct diagnosis of the pathology itself, from which and based on pharmacological knowledge, one can use the drugs available to treat the patient.
Additionally to the aforementioned pharmacological effects, one can count on anxiolytics. Such drugs act on the encephalon by modifying the psychic aspects consequently interfering on the individual's behavior 24. Anxiolytics' goal is to relive and control the unfavorable the sequence of events as anxiety and fear, promoting muscle relaxation and domain of uncoordinated movements 8.
Concerning odontalgia, classified as superficial pre- and postoperative pain, non-narcotic analgesics can be perfectly used 4.
Analgesics are administered whenever patients feel pain, such as the cases of acute dentoalveolar abscess, mainly at initial and evolution phases; and pericementitis (either of traumatic, bacterial or pharmacological origin). Concerning pulpitis, analgesics have little effect and pain would be relieved only after biopulpectomy 4.
Non-steroid anti-inflammatory drugs are the most used in Dentistry. Still according to Cruz Filho and Pécora (1997) 4, anti-inflammatory drugs are mainly indicated in pericementitis after periapical surgeries. Analgesics or anti-inflammatory drugs are unusually prescribed after pulpectomies; however, some cases in which the patient exhibits mild pain sensitivity, these drugs are required.
Importantly, the dentist firstly must assure that antibiotics are necessary. According to Siqueira Júnior (1997) 20, in approximately 60% of infection human cases, the host defenses themselves account for the process cure, without antibiotics. If fever, swelling, prostration, lymphadenitis, and acute dentoalveolar abscess is present, indicating that the infectious process is not properly controlled by the host defenses, antibiotics are required. In the absence of these signals and whether the abscess is limited, antibiotics are not necessary 2,7,22. Therefore, the aim of this study was to review the literature and discuss the use of systemic medication in Endodontics, aiming to guide the use of these drugs only when really necessary.
Literature review and discussion
This present study used the following scientific databases: Regional Library of Medicine (Bireme), Scientific Electronic Library Online (Scielo), and PubMed, Inclusion criteria comprised studies related to the subject studied – systemic medication applied to endodontics –, published between 1996 and 2013. The search used the following keywords: systemic medication, endodontic treatment, acute dentoalveolar abscess.
Anxiolytics
Anxiolytics or psycholeptics are drugs causing soothing effects, resulting in sleepiness. These drugs may act in agitation, excitability, anxiety, depression, apprehensiveness, psychosis, and neurosis state 24.
The patient showing signs of anxiety and fear is identified by either behavior or recognizing some physical signs, such as: dilated pupils, pale skin, excessive sweating, tingling of the extremities, and increasing of blood pressure and heart beating 1.
According to Haddad (2007) 8, anxiolytics are indicated in longer dental procedures, especially those performed in patients exhibiting heart diseases, diabetes, behavioral barriers and/or convulsive neurological disorders (epilepsy), and eventually in individuals with cerebral palsy and mental disabilities.
Andrade (1999) 1 pointed out other indications for anxiolytics use: 1. Whenever the signs of anxiety, apprehensiveness and fear is not controlled by verbal reassurance; 2. As pre-anesthetic medication in more invasive and traumatic dental procedures (parendodontic surgery, drainage of abscesses); 3. Immediately after accidental dental traumas; 4. Eventually, in some emergency medical cases, such as hyperventilation syndrome and myocardial infarction.
Preferably, in Dentistry, minor anxiolytics from benzodiazepine group are indicated for anxious patients with fear of dental treatment 5,24.
According to Tortamano and Armonia (2001) 24, anxiolytics can still be prescribed as auxiliary in treating pain phenomena because pain is closely related to psychic aspects.
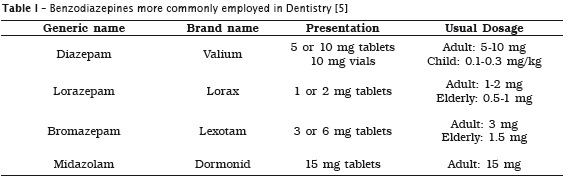
Andrade (1999) 1 emphasized among the benzodiazepine group: diazepam, lorazepam, bromazepam and cloxazolam. Haddad (2007) 8 still included in this group midazolam, which in addition to the anxiolytic effect has hypnotic action (induction to physiologic sleepiness). The authors pointed out that such drugs have the same mechanism of action, differing from only the beginning and duration of anxiolytic action.
In addition to decrease anxiety, benzodiazepines (table 1) have also other advantages, such as: decrease of basal metabolism, consequent ly delaying local anesthetic absorption and enabling a small amount of anesthetics; reduction of salivary flow and gag reflex; aid in maintain the blood pressure and glycaemia in hypertensive or diabetic patients, respectively 1. Other advantage of anxiolytics is the role in preventing emergency situations, such as lipothymy and hyperventilation syndrome, because it seems already well established that emergency cases occur much more frequently in patients with anxiety and apprehensiveness poorly controlled 12.
The use of anxiolytics is contraindicated in pregnant women (both at first and last trimesters); patients with glaucoma or myasthenia gravis; children with severe physical or mental disabilities; patients addicted to other central nervous system depressants, including chronic alcoholics; and patients with allergy to benzodiazepines 1.
The protocol use for diazepam and bromazepam is single dosage administered 1 hour before appointment, through oral route. Lorazepam should be taken 2 hours before appointment. In extremely anxious patients, the dentist can prescribe one dosage at the night before the appointment, aiming at providing a calmier sleep 1.
Analgesics
Pain has been defined as unpleasant sensorial and emotional experience associated with tissue or other type of damage. Notwithstanding, the pain is essential for the human beings because of its defensive character, acting as a warning sign of eminent or real damage to any organ or tissue. However, because human being is not adapted to this situation, which frequently becomes extremely unpleasant, pain control through specific drugs is necessary 1.
Clinically, pain is classified as superficial or deep. Superficial pain normally is well localized (needle stick, incision of soft tissues, etc.), while deep pain can irradiate, be referred to other areas (i.e., apical abscesses) and be extremely unpleasant provoking nausea, paleness, and sweating 24. According to Andrade (1999) 1, pain can occur both at pre-, trans-, and postoperative periods of invasive dental procedures in asymptomatic patients.
In Dentistry, the drugs employed in pain prevention and control includes local anesthetic solutions, and the so-called analgesic and antiinflammatory drugs 1.
Tortamano and Armonia (2001) 24 classified the analgesics in three groups: 1. Centrally acting analgesics (opioids); 2. Peripherally acting analgesics (non-opioids); 3. Anti-inf lammatory acting analgesics.
Opioid analgesics comprise morphine, codeine, meperidine, propoxyphene and dextropropoxyphene. According to Neidle and Yagiela (1989) 14, such drugs are employed exclusively for pain control in Dentistry. However, pain of dental origin frequently comes from inflammation or it is followed by this latter. Consequently, non-opioid analgesics with antiinflammatory action are the first option for dental pain relief. Opioid analgesics are particularly useful when additional pain relief is necessary. Opioid analgesics associated with aspirin, for example, are commonly employed because both central and peripheral analgesic mechanisms are involved, respectively. Among the opioid analgesics available for dental use, codeine is the drug of choice.
Generally opioids may cause physical and mental addiction, and respiratory depression. Other implications are related to possible drug interactions (with drugs prescribed by either the dentist or physician) 14,24.
Jayakodi et al. (2012) 9 affirmed that in case of pain of endodontic origin, patients should be treated with non-opioid analgesics; however, if the pain is not controlled, opioid analgesic must be used.
In an study conducted with the members of the American Association of Endodontists to determine the preference regarding analgesics use, Mickel et al. (2006) 13 proved that non-opioid drugs were more employed than opioid analgesics for most of the clinical situations.
Peripheral acting analgesics include dipyrone and p aminophenol (paracetamol). Such drugs practically do not have anti-inflammatory action 24.
Anti-inflammatory analgesics are considered as peripheral acting drugs even they also have action on central nervous system. This group comprises acetylsalicylic acid, diclofenac sodium and potassium, among others. The usual dosage for acetylsalicylic acid acts as both anti-inflammatory antipyretic drug is 30% higher than the analgesic dosage. Adverse side effects have been gastric irritation, decreased platelet adhesiveness and teratogenic effects 24.
Leonardo and Leal (1998) 10 pointed out that systemic drugs for Endodontics is restricted to the use of analgesics to provide more comfort to patient. Preferably, the dentist should prescribe either paracetamol or salicylates. Andrade (1999) 1 also recommended analgesics but warned to performed the local or total intervention of root canals. And Raldi et al. (2002) 18 suggested the use of analgesics associated with anti-inflammatory drugs, in emergency cases.
According to Andrade (1999) 1, in elderly patients, the use of either paracetamol or dipyrone is recommended for mild to moderate pain control because they do not provoke gastric irritation and interference in hemostasis. In children, the prevention in mild to moderate pain control, either paracetamol or dipyrone solutions is recommended, as drops. Similarly, these aforementioned drugs can be used in pregnant women, respecting the limit of three daily dosages, at four-hour interval, restricted by time. Cruz Filho and Pécora (1997) 4 and Tortamano and Armonia (2001) 24 emphasized that p aminophenol group (paracetamol) is the most indicated for children and pregnant women.
As the pulp is at irreversible phase, drugs are ineffective and administering analgesics is worthless. The most adequate and effective pain management is to access the root canals. As the patient is at transitional phase (from acute reversible to acute irreversible pulpitis), analgesics are effective 4,9,26. According to Lopes and Siqueira Júnior (1999) 11, analgesic/ anti-inflammatory drugs are recommended due to chair time limitation; operator's inability; periradicular pain; morphological problems; and multiple-appointment endodontic treatment.
Andrade (1999) 1 emphasized that analgesics can be administered both in cases of pulp necrosis without periapical involvement, after accessing root canal and irreversible pulpitis which mild to moderate pain is already expected and can be prevented.
Analgesics together with anti-inf lammatory drugs have been mainly indicated in cases of endodontic emergency cases such as acute pericementitis 5,18. According to Andrade (1999) 1, it is worth prescribing analgesics for postoperative pain control after canal instrumentation because the latter is an invasive intervention at greater risk of provoking pain.
In acute apical periodontitis of bacterial origin, to prescribe analgesics/anti-inflammatory drugs at 24/48 after the removal of the septic-toxic content inside root canal provides greater comfort to patient and stops the events following the acute phase 10. Lopes and Siqueira Júnior (1999) 11 recommended the use of analgesics in cases of mild postoperative pain. Severe and persistent pain treatment will depend on the situation: a) satisfactory root filling – to prescribe analgesics/anti-inflammatory drugs; b) unsatisfactory long root filling – to retreat the canal. Unsolved cases should be treated by either endodontic retreatment or periradicular surgery.
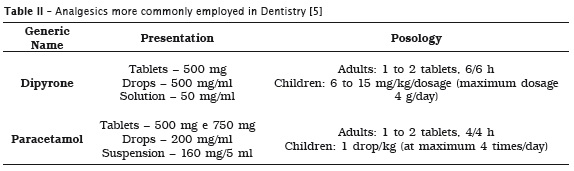
Andrade (1999) 1 pointed out that acute dentoalveolar abscess cases should be treated by dipyrone or paracetamol for pain control (table 2). According to Lopes and Siqueira Júnior (1999) 11 and Raldi et al. (2002) 18, in cases of acute periradicular cases, analgesic and antiinflammatory drugs are recommended at all phases. Cruz Filho and Pécora (1997) 4 emphasized that analgesics should be administered whenever the patient feels pain in cases of acute dentoalveolar pain, mainly at the two first phases.
Anti-inflammatory drugs
Inflammation is the body's defense response against different injury types: physical, chemical, and biological 24.
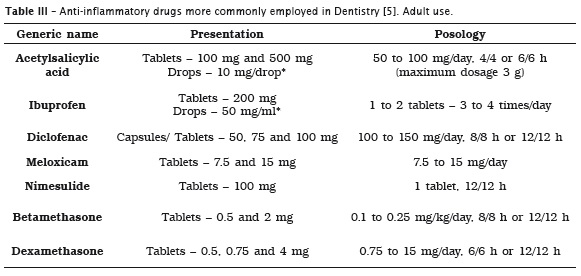
Andrade (1999) 1 divided anti-inflammatory drugs into two groups: corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs) Table 3 shows the anti-inflammatory drugs more used in Dentistry.
Both betamethasone and dexamethasone are the corticosteroids of choice for dental use, through systemic route, because they have an action power 25 times greater than that of hydrocortisone, the standard drug of corticosteroids. Moreover, betamethasone and dexamethasone exhibit longer plasmatic half-life enabling their use at single preoperative dosage. It is important to emphasize that corticosteroids employed at restrained time, even massive dosages, practically do not show side effects of clinical significance 1.
Pochapski et al. (2009) 17 observed the effect of dexamethasone as preoperative drug. By evaluating the effectiveness of single dexamethasone dosage one hour before the procedure, the authors found significant reduction in postoperative pain for 4 to 12 hours.
Still according to Andrade (1999) 1, both betamethasone and dexamethasone has been contraindicated in cases of patients presenting: fungal systemic diseases and/or herpes simplex eye infection; active or inactive tuberculosis; allergy to any of the drugs. Caution should be taken with pregnant or lactating women; diabetic, hypertensive, cardiac, and immunosuppressed patients; and patients with active peptic ulcer, Acute disseminated bacterial infection, and bronchial asthma.
NSAIDs can also be indicated as pre- and postoperative drugs in dental procedures in which severe inflammatory response is expected aiming at preventing excessive pain and swelling. Similarly, NSAIDs can be employed as adjuvants to clinical procedures for pain control in cases that acute inflammatory events are already installed, such as pericementitis, especially those from diclofenac sodium and potassium 1.
Cruz Filho and Pécora (1997) 4 indicated antiinflammatory drugs in cases of pericementitis and after periapical surgeries. In cases of pulpectomies, it is not common to prescribed analgesic/antiinf lammatory drugs, except if patient exhibits moderate pain, when anti-inflammatory drugs are employed.
In cases of pain due to endodontic treatment, especially in cases of over instrumentation or difficult instrumentation (atresic root canals, pulp calcifications), preoperative medication is advised (4 mg of betamethasone, 30 minutes before the appointment, at single dosage).
Raldi et al. (2002) 18 recommended the use of analgesic and anti-inflammatory drugs in cases of pulp pathology. Andrade (1999) 1 indicated the use of corticosteroid because they do not provoke gastric irritation and interference in hemostasis.
According to Leonardo and Leal (1998) 10, in acute apical periodontitis of bacterial origin, one should prescribe analgesics/anti-inflammatory drugs at 24/48 after the removal of the septic-toxic content inside root canal. In pericementitis with pup involvement, one should prescribe 4 mg of betamethasone or dexamethasone (at single dosage, through oral route), to instrument the root canal partially or totally, and adjust the patient's occlusion.
In pericementitis without pup involvement (i.e. oclusal trauma), one should prescribe betamethasone or dexamethasone 4 mg (at single dosage, through oral route); or ibuprofen 600 mg, or nimesulide 100 mg at every 12 hours; or meloxicam, at single dosage, for at maximum 48 hour period, after tooth occlusion adjustment 1,6.
Estrela (2004) 6 pointed out that in cases of symptomatic traumatic apical periodontitis, the absence of microorganisms is assumed, so that anti-inflammatory drugs are prescribed.
According to Andrade (1999) 1, both to prevent and control acute inflammatory responses of dental origin, treatment length of these drugs must be set at a maximum period of 48 hours. Chronic use of anti-inflammatory drugs (for more than 4 to 5 days) lacks of scientific support.
Antibiotics
Typical bacterial dental infect ion, either periodontal or periapical, is currently considered as mixed infection with involvement of aerobic, facultative anaerobic, and restricted anaerobic microorganisms. Dental infections are unlikely composed of pure cultures, that is, to be caused by a single microorganism. Accordingly, the dynamics of this infection is very complex and does not allow the establishment of standard evolution or course 1.
According to Andrade (1999) 1, antibiotics are chemically substances produced by either live microorganisms or semi-synthetic process aiming at inhibiting pathogens and eventually destroying these microorganisms. Antibiotics can be classified according to different criteria, but the most important criteria have been: 1) o biological action – bactericide (capable of destroying susceptible microorganisms) and bacteriostatic (only inhibits the growth and multiplication of susceptible microorganisms); 2) spectrum of action – antibiotics acting mainly against gram-positive bacteria (i.e., penicillins G, penicillins V, vancomycin); antibiotics acting mainly against gram-negative bacteria (i.e., aminoglycosides), antibiotics acting mainly against gram-negative and gram-positive bacteria (i.e., semisynthetic penicillins – amoxicillin, ampicillin –, cephalosporins, tetracyclines), antibiotics acting against anaerobes (i.e., penicillins, tetracyclines, metronidazole), antibiotics acting against spirochetes (i.e., penicillins, cephalosporins, erythromycin, tetracyclines), antibiotics acting against fungi (i.e., nystatin) and antibiotics acting against other microorganisms.
Siqueira Júnior (1997) 20, Soares et al. (2005) 21 and Oliveira et al. (2010) 15 pointed out the occasions in which antibiotics have to be prescribed in Endodontics: a) acute periapical abscesses with signs of systemic involvement; acute periapical abscesses in immunosuppressed patients; b) prophylaxis of infection associated with tooth avulsion; c) treatment of persistent symptomatology and/or exudation after the performance of all available options to control inter-radicular infection; d) prophylaxis against bacteremia caused by endodontic treatment in immunosuppressed patients or patients susceptible to bacterial endocarditis according the guidelines of the American Heart Association (AHA) or the recommendations of the patient's physician ; e) abscess dissemination causing diffuse tumefactions.
Acute apical abscess with localized tumefaction without systemic involvement occurring in healthy patients can be properly treated by drainage through incision and/or root canal, followed by the complete chemical-mechanical preparation of root canal and application of intracanal medication, without requiring antibiotics.
In healthy indiv iduals, the drainage of the purulent exudate enables the significant reduction of microbial irritants and inflammation chemical mediators, allowing the beginning of the healing process without antibiotics. Unlikely, in immunosuppressed patients, antibiotics should be prescribed even in case of effective drainage because systemic complication may occur even in mild infectious cases. When acute apical abscess is associated with diffuse tumefactions leading to develop cellulites with infectious process dissemination to other anatomic spaces, or when acute apical abscess exhibits evidences of systemic involvement, such as fever, malaise, regional lymphadenitis or trismus, antibiotics are necessary as adjuvant treatment to drainage because the patient's immune system is incapable of stopping the infection advance. Amoxicillin associated with clavulanic acid (three times per day) has been more effective and safer option because of the isolated bacterial profile of this lesion type 15.
According to Wannmacher and Ferreira (1999) 26, the duration of systemic therapy in abscess treatment should be until some days after the disappearance of clinical manifestations, generally, from 7 to 10 days. This period avoids relapses.
Pallasch (1996) 16 affirmed that longer antibiotic therapy does not destroy all resistant microorganisms and only selects resistant species. If professional's expertise and infection nature (orofacial infections last from 2 to 7 days) determine that the disease course will be from 3 days, then 3 days of antimicrobial therapy is enough; if 5 days are set, 5 treatment days are necessary, and so on. Accordingly, as the clinical disease evidences are practically solved, systemic therapy can be interrupted.
Vier-Pelisser et al. (2008) 25 studied which are the intracanal and systemic medications used in Brazilian School of Dentistry in emergency treatment of acute periapical abscess. By using a questionnaire to record intracanal and systemic medications, the authors concluded that antibiotics were the most used systemic medication, regardless of the abscess phase, with amoxicillin the drug of choice.
Tortamano and Antoniazzi (2007) 23 observed the effectiveness of chemical-mechanical preparation of root canals associated with the systemic use of azithromycin in acute periapical infections with systemic involvement. By conducting an open non-comparative study to evaluate the clinical evolution, antimicrobial activity and tolerability of azithromycin in 38 patients submitted to single dosage of 500 mg, for a period of 3 days, the authors deduced that azithromycin associated with chemical-mechanical preparation is a good option to treat acute periapical infections with systemic involvement thus being indicated for patients allergic to penicillin.
In cases of replantation of avulsed teeth, antibiotics favor the treatment prognosis 20. The International Association for Dental Traumatology (IADT) publ ished in 2007, a consensus on management of tooth avulsion cases in which recommended the use of doxycycline systemically administered (100 mg/day for 7 days) for these cases. Although tetracyclines have been associated with tooth pigmentation, this side effect generally is observed with dosages above 3 grams and periods longer than 10 days in children aged less than 8 years. However, doxycycline, different from other tetracyclines, does not seem to cause intrinsic tooth pigmentation. The option for young patients is penicillin V (phenoxymethylpenicillin – 40 mg/kg/day or 50.000 U/kg/day, at 6/6 hours for 7 days) 15.
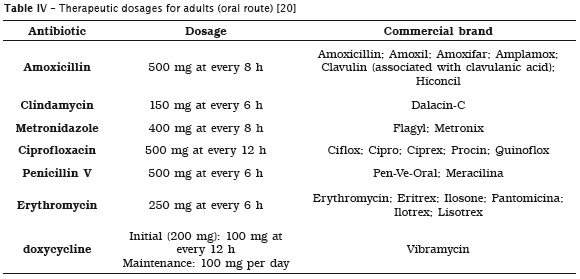
Rarely, when intracanal procedures of chemicalmechanical preparation and intracanal medication are not enough to eliminate the infection agent (which can already be closely in the periradicular tissues), antibiotics can be used to control persistent signs and symptoms, such as persistent exudate at obturation moment. Amoxicillin 875 mg, soluble tablets, at every 12 hours; amoxicillin 500 mg capsules at every 8 hours are the antibiotics of choice, as seen in table 4. Clindamycin (capsules of 300 mg, at every 8 hours) can be administered to allergic patients, but metronidazole is not indicated because frequently the microorganisms associated with these cases have been Actinomyces and Propionibacterium, generally resistant to this antimicrobial drug 15.
By detecting the resistance of bacterial genes to antibiotics in samples of acute and chronic endodontic infection, Rôças and Siqueira Júnior (2013) 19 observed that after root canal instrumentation, approximately 60% of the cases still presented bacteria, which disappeared after the use of antibiotics.
Root canal therapy is at low or negligible risk for developing bacterial endocarditis, since the main Endodontics's principle is respected: lack of periapical aggression, through instrumentation restricted to the canal. Thus, prophylactic antibiotics are not indicated. The same is indicated for intraoral anesthetic infiltration. Unlikely, intraligamentary anesthesia and endodontic procedures at risk of instrumentation beyond the foramen (i.e., apical resorptions) required antibiotic prophylactics in patients at risk of endocarditis 21.
The protocol proposed by the American Heart Association states that antibiotics must be administered one hour (oral route) or 30 minutes (intravenous route) before the procedure. The antibiotics of choice are amoxicillin 2 grams. Patients allergic to penicillin should receive clindamycin 600 mg 15.
It is very important emphasizing that in acute orofacial infections, the common reason of antibiotic failure is attributed to lack of infection source elimination. The dentist should be aware of direct clinical intervention attempting to eliminate the infectious foci, because in cases of endodontic infections, systemic treatment is worthless without the association of the local treatment of the disease 1.
Conclusion
In Endodontics practice, systemic medication is occasionally indicated as adjuvant to treatment by acting on pain, inf lammation and infection control, thus providing greater comfort and more security to patient.
It is extremely important that the dentist know the drug type to be used in each case and whether systemic therapy is really required, by carefully analyzing the clinical signs and symptoms.
Other important factor is to observe carefully the treatment time with such medications, mainly for antibiotics, because indiscriminate antibiotic use is the main cause of bacterial resistance. Thus, caution is necessary when using these medications, by respecting the results of well-controlled studies that show the best options for clinical use of such drugs.
References
1. Andrade ED. Terapêutica medicamentosa em Odontologia. São Paulo: Artes Médicas Sul; 1999. 188 p. [ Links ]
2. Baumgartner JC, Xia T. Antibiotic susceptibility of bacteria associated with endodontic abscesses. Journal of Endodontics. 2003;29(1):44-7.
3. Castilho LS, Paixão HH, Perini E. Prescrição de medicamentos de uso sistêmico por cirurgiõesdentistas, clínicos gerais. Rev Saúde Pública. 1999 Jun;33(3):287-94.
4. Cruz Filho AM, Pécora JD. Terapêutica – antibióticos/analgésicos/antiinflamatórios. 1997 [cited 2013 Mar 20]. Available from: <www.forp. usp.br>.
5. Cunha GL. Medicação sistêmica na prática endodôntica. Estação Científica; 2007. 6. Estrela C. Ciência Endodôntica. São Paulo: Artes Médicas; 2004.
7. Fazakerley MW, McGowan P, Hardy P, Martin MV. A comparative study of cephradine, amoxycillin and phenoxymethylpenicillin in the treatment of acute dentoalveolar infection. Br Dent J. 1993;174:359-63.
8. Haddad AS. Odontologia para pacientes com necessidades especiais. 1. ed. São Paulo: Santos; 2007. p. 476-83.
9. Jayakodi H, Kailasam S, Kumaravadivel K, Thangavelu B, Mathew S. Cl inical and pharmacological management of endodontic flareup. J Pharm Bioallied Sci. 2012 Aug;4(2):294-8.
10. Leonardo MR, Leal JM. Endodont ia: tratamento de canais radiculares. 3. ed. São Paulo: Panamericana; 1998.
11. Lopes HP, Siqueira Júnior JF. Endodontia – biologia e técnica. 2. ed. Rio de Janeiro: Medsi; 1999. p. 539-48.
12. Malamed S. Medical emergencies in the dental office. 4. ed. Saint Louis: Mosby; 1993. p. 10-49.
13. Mickel AK, Wright AP, Chogle S, Jones JJ, Kantorovich I, Curd F. An analysis of current analgesic preferences for endodontic pain management. J Endod. 2006 Dec;32(12):1146-54.
14. Neidle EA, Yagiela JA. Farmacologia e terapêutica para dentistas. 3. ed. Rio de Janeiro: Guanabara Koogan; 1989. p. 222-34.
15. Oliveira JCM, Dias LA, Uzeda M. Antibióticos sistêmicos em endodontia: novos conceitos. Rev Bras Odontol. 2010 Jul/Dec;67(2):247-54.
16. Pallasch TJ. Pharmacokinetic principles of antimicrobial therapy. Periodontology. 1996;10:5- 11.
17. Pochapski MT, Santos FA, Andrade ED, Sidney GB. Effect of pretreatment dexamethasone on postendodontic pain. Oral Surg Oral Med Oral Pathol Oral Radio Endod. 2009 Nov;108(5):790-5.
18. Raldi DP, Oliveira RB, Lage-Marques JL. Medicação sistêmica como coadjuvante do tratamento endodôntico. Rev APCD. 2002 Sep/ Oct;56(5):59-62.
19. Rôças IN, Siqueira Júnior JF. Detection of antibiotics resistence genes in samples from acute and chronic endodontic infections and after treatment. Arch Oral Biol. 2013 Mar; 58(2):1123-8.
20. Siqueira Júnior JF. Tratamento das infecções endodônticas. Rio de Janeiro: Medsi; 1997. 196 p.
21. Soares RG, Salles AA, Irala LED, Limongi O. Antibioticoterapia sistêmica em endodontia: quando empregar? Stomatos. 2005 Jul/Dec;11(21):33-40.
22. Souza-Filho FJ, Gomes BPFA, Ferraz CCR, Teixeira FB, Zaia AA. Drenagem de abscessos periapicais. In: Endodontia – trauma, odontologia. APCD, Ed. Artes Médicas; 2002.
23. Tortamano IP, Antoniazzi JH. Infecções periapicais agudas com envolvimento sistêmico – preparo químico-cirúrgico de canais radiculares associado ao uso sistêmico da azitromicina (avaliação clínica, microbiológica e tolerabilidade). Rev Inst Ciênc Saúde. 2007;25(3):263-9.
24. Tortamano N, Armonia PL. Guia terapêutico odontológico. 14. ed. São Paulo: Santos; 2001.
25. Vier-Pelisser FV, Garbin RP, So MVR, Marca C, Pelliser A. Medicações intracanal e sistêmica preconizadas nas faculdades de Odontologia brasileiras para o tratamento de urgência do abscesso periapical agudo. Rev Odonto Ciênc. 2008;23(3):278-82.
26. Wannmacher L, Ferreira MBC. Farmacologia clínica para dentistas. 2. ed. Rio de Janeiro: Guanabara Koogan; 1999.
 Corresponding author:
Corresponding author:
Nanete de Menezes Silva
Avenida Murilo Dantas, 1.155 – Bloco Bacamarteiros – ap. 502 – Farolândia
CEP 49032-490 – Aracaju – SE – Brasil
E-mail: nanete_msilva@hotmail.com
Received for publication: August 26, 2013
Accepted for publication: February 3, 2014













