Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.11 no.3 Joinville Jul./Set. 2014
Case Report Article
Prader-Willi Syndrome: clinical case report
Marta Elisa Gadens I; Octávio Augusto Kowalski I; Gilmar José Begnini II; Maria Fernanda Torres III; João Armando Brancher II; Andréa Paula Fregoneze I
I Department of Dentistry, Pontifical Catholic University – Curitiba – PR – Brazil
II Department of Dentistry, Positivo University – Curitiba – PR – Brazil
III Department of Anatomy, Federal University of Paraná – Curitiba – PR – Brazil
ABSTRACT
Introduction: Prader-Willi syndrome (PWS) is a neurobehavioral genetic disease whose cause is failure on chromosome 15. It is considered the primary genetic cause of obesity, since it is characterized by hyperphagia. Although the scientific literature will produce articles on Prader-Willi syndrome, few reported oral conditions of these patients. Objective: This study aimed to describe the oral health status of a patient diagnosed with PWS. Case report: A boy aged 10 years-old, leucoderma, attended the Discipline of Dentistry for Special Care Patients, Pontifical Catholic University of Paraná (PUCPR), with all the inherent PWS characteristics such as hyperphagia and obesity. Clinical, radiographic and laboratory tests were performed to verify the oral health conditions which showed the presence of biofilm accumulation, gingivitis and a high DMFT index. It was necessary to adequate oral environment through extractions, restorations, and prophylactic therapy. Conclusion: Considering the information obtained, it was concluded that the motivation to maintain oral health should be constant for this patient and involve family, since hyperphagia, which is a determinant for obesity, decisively contributes to the evolution of oral diseases.
Keywords: Prader- Willi Syndrome; Dentistry for special patients; oral health.
Introduction
Prader-Willi syndrome (PWS), described by Prader, Labhart and Willi in 1956, is considered a neurobehavioral disease currently indicated as one of the most frequent cause of chromosome microdeletions 9. PWS is the most common phenotype of genetic obesity. Additionally, Prader-Willi and Angelman syndromes are the main recognized human diseases determined by mechanisms of genomic imprinting, that is, a genetic phenomenon in which certain genes are expressed by only one allele 7. In this case, deletion of the proximal portion of the long arm of the paternal chromosome 15 (15 q11-13) or, more rarely translocation of chromosome 15 occurs 8. The prevalence is of approximately 1 for each 15,000 births on both genders 6.
PWS is characterized by two clinical phases. At first phase, the symptoms are neonatal hypotonia, difficulties to be fed, lethargy, weak cry and hyporeflexia. At second phase, starting from six months of age, a gradual improvement of hypotonia, hyperphagia, weight gain and obesity occur 7,15. Obesity is the major cause of the morbidity and mortality increasing among patients exhibiting the syndrome 3. Clinical features comprised also respiratory problems during sleep, mild to severe mental retardation learning disability and short stature 7,13,15.
The syndrome diagnosis is clinical based on physical and behavioral data which can be confirmed by the analysis of chromosome 15 segment (q11-q13) through methylation or in situ hybridization 10.
With regard to oral health of PWS individuals, few studies have been conducted. Some authors reported an increasing in carious teeth and salivary f low reduction 4,13, in addition to enamel hypoplasia 5,6. Although scientific literature is reporting on PWS, little studies focus on oral health conditions of these individuals. Therefore, the aim of this study was to describe the oral condition of a PWS individual treated at the Pontifical Catholic University of Paraná (PUCPR).
Clinical case report
This study was conducted on a leucoderma male patient born by normal delivery. Pre- and post-natal tests were normal indicating a healthy fetus/newborn. Until 6 months of age, the infant was formula-fed exclusively, period after which he started to be fed by solid food. The patient was diagnosed with PWS at three years-old by the medical team of the Clinical Hospital of the Federal University of Parana (UFPR), due to the presence of muscle hypotonia, delay in common psychomotor development phases, difficulty in sucking/swallowing, weak cry, and somnolence.
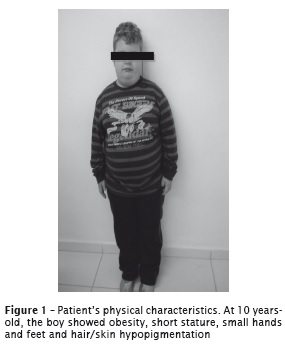
At 10 years-old, the patient started dental treatment at the Discipline for Special Care Patients (PUCPR). At anamnesis, marked physical alterations of the syndrome were noted, such as: myopia, strabismus, obesity, short stature (figure 1), maxillary lip and labial commissures facing down, small hands, and hypopigmentation of the hair, skin and eyes. The patient's mother reported during anamnesis that her pregnancy was uneventful and no other cases have been seen in the family. The mother still informed that her son had episodes of nervousness and anxiety due to dietary restrictions. The patient has been treated by a multidisciplinary team composed by nutritionist, psychologist, and endocrinologist.
During his free time, the patient liked to play videogame, listen to music and sing. During current medical history, patient exhibited cognitive deficiency characterized by learning difficulties, mainly related to writing. During past dental history, the mother reported that his first dental appointment was at seven years-old, at school, and the behavior was satisfactory.
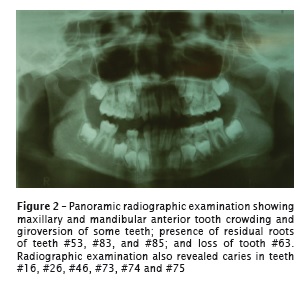
Intraoral cl inical examinat ion revealed significant biofilm accumulation, gingivitis, dry mouth and angular cheilitis. Occlusion examination evidenced ogival palate, anterior crowding, and Class II malocclusion. Panoramic and periapical radiographic examination indicated delay in tooth eruption and tooth crowding at maxillary and mandibular anterior teeth (figure 2).
Discussion
In this present study, a boy aged 10 years-old was diagnosed with PWS and treated at PUCPR's dental clinic. The clinical characteristics of this syndrome reported in the literature, such as: neonatal hypotonia, difficulties in feeding, lethargy weak cry, hyporeflexia, hyperphagia, and obesity 7,11,15, were confirmed by the patient's mother during anamnesis. Short stature, small hands and feet, skin/hair/retina hypopigmentation, thin lips, labial commissures facing down, myopia, and strabismus also described in prior studies were also observed 4,13,14.
Randomized clinical trials have demonstrated the favorable effect of growth hormone (GH) reposition to reduce fat mass and increase lean body mass, complementing nutritional guidance. Not with standing, GH seems not to have significant effect on controlling hyperphagia in these patients 13.
Corroborating Cortés et al. 7, Olczak- Kowalczyk et al. 13, and Vargas et al. 15, the patient of this case report showed learning disorder related to writing; but with mild cognitive deficiency. PWS patients also presented bone mineralization decrease, fact explaining the high osteoporosis incidence associated with the syndrome 5.
According to the patient's mother, episodes of irritability were rare, mainly related to dietary restrict ion. Prior studies also reported this situation 1,11. Generally, this study's patient had a sociable and friendly behavior with all multidisciplinary team.
The peculiar facial characteristics of PWS patients were also observed in this case report: almond eyes, thin maxillary lips, labial commissures facing down, and dysmorphic face. Among the oral manifestations reported by Carvalho et al. 5,6, this case report found the presence of caries, enamel hypoplasia, and malocclusion. On the other hand, ogival palate, delay in tooth eruption, supernumerary teeth, microdontia, micrognathia, taurodontism and candidiasis were not seen.
Hyperphagia, the most important PWS feature 7, can explain the high rate of carious teeth observed in this patient who exhibited a DMTF index greater than that of children at same age. Six teeth had caries, three were residual roots and one tooth was lost. The treatment executed comprised the extractions of teeth #53, #83 and #85; resin composite restorations of teeth #16, #26, #46, and #74; and light-cured glass ionomer cement restoration of teeth #73 and #75. Next, preventive measures were instituted with sealants on many teeth and fluoride varnish application.
Other important factor contributing to oral health deterioration is salivary flow decrease 4,13, a feature clinically observed through dry mucosae. To evaluate the amount of produced saliva, we used the method proposed by Navazesh et al. 12 and Banderas-Tarabay 2. The produced volume was very low, characterizing hyposalivation.
The next step was to instruct the family to adopt measures promoting oral health maintenance. The relatives were instructed regarding to proper oral hygiene, to make them also responsible by the treatment. The patient still continued being followed-up at the Discipline of Dentistry for Special Care Patients of the institution to preserve oral health.
Conclusion
Based on the information obtained after clinical and radiographic examination, it can be concluded that both PWS patient and the family should be constantly motivated to maintain oral health, because hyperphagia which is determinant for obesity, decisively contributed to increase DMTF index. Additionally, hyposalivation can contribute to develop bacterial biofilm and gingivitis.
References
1. Almeida MQ, Cercato C, Rascovski A, Goldbaum TS, Figueiredo DA, Matsuda M et al. Results of biliopancreatic diversion in two patients with Prader-Willi syndrome. Obes Surg. 2005 Jun- Jul;15(6):901-4. [ Links ]
2. Banderas-Tarabay JA. Flujo y concentration de proteínas en saliva total humana. Salud Publica Mex. 1997;39(5):433-41.
3. Braghet to I , Rodr íguez A, Debandi A, Brunet L, Papapietro K, Pineda P et al. Prader- Willi Syndrome (PWS) associated to morbid obesity: surgical treatment. Rev Med Chil. 2003 Apr;131(4):427-31.
4. Caldas Júnior AF, Rodrigues VMS, Caldas KU, Barros JAP, Cabral AMC, Souza MF. Síndrome de Prader-Willi: relato de caso. Rev Cir Traumatol Buco-Maxilo-Fac. 2006 Jan-Mar;6(1):37-42.
5. Carvalho DF, Cercato C, Almeida MQ, Mancini MC, Halpern A. Therapeutical approach of obesity in Prader-Willi Syndrome. Arq Bras Endocrinol Metabol. 2007 Aug;51(6):913-9.
6. Carvalho DR, Trad CS, Pina Neto JM. Atypical presentation of Prader-Willi Syndrome with Klinefelter (XXY Kartype) and craniosynostosis. Arq Neuropsiquiatr. 2006 Jun;64(2A):303-5.
7. Cortés MF, Alliende RMA, Barrios RA, Curotto LB, Santa María VL, Barraza OX et al. Clinical, genetic and molecular features in 45 patients with Prader-Willi syndrome. Rev Med Chile. 2005 Jan;133(1):33-41.
8. Damiani D. Growth hormone usage in Prader- Willi syndrome. Arq Bras Endocrinol Metabol. 2008 Jul;52(5):833-8.
9. González LC, Villa CG, Cárdenas AC. Prader Willi Syndrome: saliva quantification and culture in 10 patients. Med Oral Patol Oral Cir Bucal. 2008 Dec;13(12):773-7.
10. Hartley SL, Maclean Jr WE, Butler MG, Zarcone J, Thompson T. Maladaptive behaviors and risk factors among the genetic subtypes of Prader-Willi syndrome. Am J Med Genet A. 2005 Jul;136(2):140-5.
11. Mesquita MLG, Brunoni D, Pina Neto JM, Kim CA, Melo MHS, Teixeira MCTV. Fenótipo comportamental de crianças e adolescentes com síndrome de Prader-Willi. Rev Paul Pediatr. 2010 Mar;28(1):63-9.
12. Navazesh M, Mulligan RA, Kipnis V, Denny PA, Denny PC. Comparison of whole saliva flow rates and mucin concentrations in healthy Caucasian young and aged adults. J Dent Res. 1992 Jun;71(6):1275-8.
13. Olczak-Kowalczyk D, Witt A, Gozdowski D, Ginalska-Malinowska M. Oral mucosa in children with Prader-Willi syndrome. J Oral Pathol Med. 2011 Nov;40(10):778-84.
14. Santos VM, Henrique de Paula F, Osterne EM, Nery NS, Turra TZ. Morbid obesity in an adolescent with Prader-Willi syndrome. Rev Med Chil. 2009 Feb;137(2):264-8.
15. Vargas NR, Pérez TM, Garcia RM, Luaces VC, Guerrero LG. Síndrome de Prader-Willi. Presentación clínica de los pacientes y revision de la literature. Rev Cubana Pediatr. 2006 Mar;78(1).
 Corresponding author:
Corresponding author:
Andréa Paula Fregoneze
Avenida Manoel Ribas, 750 – ap. 303 – Mercês
CEP 80510-020 – Curitiba – PR
E-mail: afregoneze@gmail.com
Received for publication: December 1, 2013
Accepted for publication: December 13, 2013













