Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.11 no.4 Joinville Out./Dez. 2014
Case Report Article
Intraosseous mucoepidermoid carcinoma of the mandible – a rare case report
Shailaja Sankireddy I; Atul Kaushik I; Vinod Vijaychander I; Asha Latha gannepalli II; Bhargavi Krishna Ayinampudi II; Sridevi Koduri I
I Department of Oral Medicine and Radiology, SGT Dental College and Hospital, Gurgaon
II Department of Oral Pathology, Panineeya Dental College and Hospital, Hyderabad
ABSTRACT
Introduction: Mucoepidermoid carcinoma (MEC) is the most common salivary gland malignancy. The majority of these tumors arises in the parotid and minor salivary glands but may rarely develop intraosseously. Primary intraosseous mucoepidermoid carcinoma (PIOC) of the jaw bones is an extremely rare malignant salivary gland tumor. Very few cases have been reported in the literature to date. Case report: The current manuscript highlights clinical and radiographic features of a rare case of PIOC in a 32 year old Indian female patient. Conclusion: All the dental practitioners should be aware of the protean features of central MEC. These lesions should be included in the differential diagnosis of unilocular and multilocular radiolucent lesions of the jaws. An early and accurate diagnosis is important so that the neoplastic transformation must be identified and treated effectively.
Keywords: primary intraosseous mucoepidermoid carcinoma; salivary gland; mandible.
Introduction
MEC is the most commonly occur r ing malignant salivary gland neoplasm comprising 2.8% -15% of all salivary gland tumors 2. Aberrant salivary gland neoplasms arising within the jaws as primary central bony lesions are extremely rare comprising 2%-4.3% of all MEC reported 4,8.
In 1945, Stewart and associates described the mucous secreting and epidermal cellular component of mucoepidermoid carcinoma, thus establishing it as a distinct pathological entity 7. Bhasker in 1963 reported 2 cases and analyzed the criteria for their central origin, histology and pathogenesis 1. In 1991, after a systematic review of its histology and degree of differentiation, the World Health Organization (WHO) classification recommended that the term "mucoepidermoid tumor" be changed to "mucoepidermoid carcinoma" 11. Waldron and Mustoe suggested that intraosseous MEC be included in primary intraosseous carcinoma of jaw as type 4 13.
Classification of PIOC
• Type 1: PIOC ex odontogenic cyst;
• Type 2a: Malignant ameloblastoma;
• Type 2b: Ameloblastic carcinoma arising de novo, ex ameloblastoma or ex odontogenic cyst;
• Type 3: PIOC arising de novo: (a) keratinizing type; (b) non-keratinizing type;
• Type 4: Intraosseous MEC.
The current literature search reveals that PIOC are very rare neoplasms and only few cases have been reported in literature 5,6. The current manuscript highlights features of a rare case of PIOC in a 32 year old Indian female patient.
Case report
A 32 year old female patient reported to the Department of Oral Medicine and Radiology with the complaint of a painful swelling on left side of mandible for the last 1 month. The swelling was accompanied by fever and pain. The patient also complained of difficulty in mastication and deglutition.
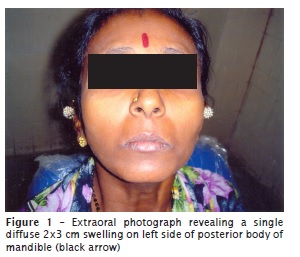
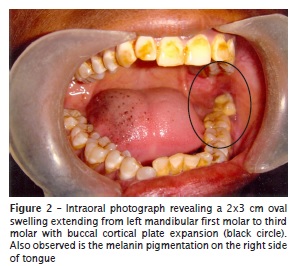
Extraoral examination revealed a single diffuse 2x3 cm swelling on left side of posterior body of mandible which was tender and firm in consistency (figure 1). Left submandibular lymph nodes were palpable, tender, firm and not freely movable. Intraoral examination revealed a 2x3 cm oval swelling extending from left mandibular first molar to third molar with buccal cortical plate expansion (figure 2). Pulp vitality testing revealed that tooth #36 was vital, but teeth #37 and #38 did not elicit any response. There was grade-one mobility of tooth #38 and grade-three mobility of tooth #37. The mucosa overlying the swelling was slightly bluish in color.
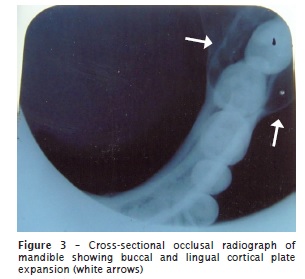
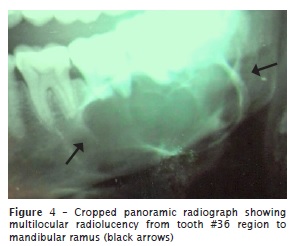
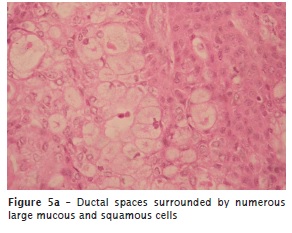
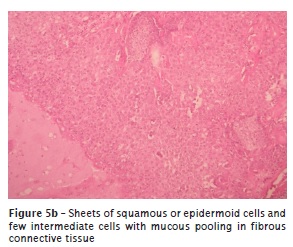
Cross-sectional occlusal radiograph of mandible revealed buccal and lingual cortical plate expansion (figure 3). Panoramic radiograph showed multilocular radiolucency from tooth #36 area to the mandibular ramus. Root resorption of teeth #36, #37 and #38 and thinning of inferior border of mandible was observed (figure 4). A bone biopsy specimen was taken in the Department of Oral and Maxillofacial Surgery and the histopathology revealed pseudo-cystic and ductal mucin pooled spaces lined by mucous cells and squamous or epidermoid cells. Few areas showed islands and sheets of epidermoid cells, intermediate cells with minimal cellular atypia, and few mitotic figures. The mucous extravasation was observed in fibrous connective tissue stroma, suggesting the diagnosis of low grade MEC (figure 5a and 5b). The patient was advised to undergo a pre-operative cone beam computed tomography scan for mandible, but the patient was not willing for it.
The patient was educated about the necessity of early treatment and was referred to an oncology center for management of MEC.
Discussion
PIOC are very rare neoplasms of salivary gland origin, first described by Lepp in 1939 9. Central MEC affects females twice more frequently than males and involves the mandible twice more often than the maxilla 4. The most common site of occurrence is the premolar-molar-angle region of the mandible. It has been reported in all ages ranging from 1 to 78 years, with the majority of cases occurring in the 4th and 5th decades of life 9. The main symptoms are swelling and pain with trismus, paresthesia and tooth mobility being noted occasionally 3.
Regarding its pathogenesis four possible origins have been described which include entrapment of retro molar mucous glands within the mandible, which subsequently undergo neoplastic transformation; developmentally induced embryonic remnants of the sub-maxillary gland within the mandible; neoplastic transformation of the mucous secreting cells commonly found in the pluripotent epithelial lining of dentigerous cysts associated with impacted third molars; and 4) neoplastic transformation and invasion from the lining of the maxillary sinus 12.
Several authors have suggested criteria required for diagnosing a lesion as a central MEC, independent of whether it arises from an odontogenic cyst or tumor 3,5,9.
1. Intact cortical plates (However, cortical perforation does not exclude PIOC (type 4);
2. Radiographic evidence of bony destruction, with poorly defined permeative margins;
3. Exclusion of another primary lesion in neighbouring salivary glands or other tissues mimicking the histological architecture of salivary gland tumours;
4. Exclusion of an odontogenic tumour or a metastatic lesion;
5. Histopathological confirmation;
6. Detectable intracellular mucin.
Radiographic examination is important to know the diagnosis, categorization as a central lesion and the extent of the lesion with involvement or encroachment of adjacent vital structures. Brookstone and Huvos suggested a three-grade classification for intraosseous MEC 3. Grade 1, without expansion and rupture of cortical plate; grade 2, with expansion but without rupture of cortical plate; grade 3, with rupture of cortical plates or presence of regional metastasis. The case presented here showed buccal cortical plate expansion and could be imputed as grade 2 disease.
Most central mucoepidermoid carcinomas are low grade and exhibit a good survival rate. In a review of 64 patients, Brookstone and Huvos observed 40% recurrences after conservative surgical modalities such as curettage, enucleation, marsupialisation and marginal resection with or without adjuvant therapy, whereas in the group treated by radical methods such as segmental resection with/without treatment of associated neck and/ or adjuvant therapy only 4% recurred 3. This suggests that radical resection offers the best chance of tumor eradication and prevention of local recurrence and late distant metastasis. Adjuvant radiotherapy is recommended for high-grade tumors.
Conclusion
Central MEC should always be included in the differential diagnosis of unilocular and multilocular lesions such as dentigerous cyst, odontogenic keratocyst, ameloblastoma adenomatoid odontogenic tumor, ameloblastic fibroma, central odontogenic fibroma, glandular odontogenic cyst, desmoplastic fibroma, squamous cell carcinoma arising in a dentigerous cyst and a metastatic lesion to the jaw. The clinical significance of malignant tumors arising from odontogenic cysts or de novo should never be underestimated as illustrated by the present case. This emphasizes the importance of radical surgery, adjuvant treatment and a careful histopathological evaluation of all excised tissue so that such neoplastic transformation may be identified and treated effectively.
References
1. Bhaskar SN. Central mucoepidermoid tumors of the mandible. Report of 2 cases. Cancer. 1963;16:721-6. [ Links ]
2. Brad J, Ines V. Central mucoepidermoid carcinoma with an atypical radiographic appearance. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e51-3.
3. Brookstone MS, Huvos AG. Central salivary gland tumors of the maxilla and mandible: a clinicopathologic study of 11 cases with an analysis of the literature. J Oral Maxillofac Surg. 1992;50:229-36.
4. Chan KC, Pharoah M, Lee L, Weinreb I, Perez-Ordonez B. Intraosseous mucoepidermoid carcinoma: a review of the diagnostic imaging features of four jaw cases. Dentomaxillofacial Radiology. 2013;42:20110162.
5. Darling MR, Ciavarro C, Daley TD. Pericoronal radiolucency in the posterior mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:139-43.
6. De Mello-Filho FV, Brigato RR, Mamede RC, Ricz HM, Saggioro FP, Xavier SP. Central mucoepidermoid carcinoma: report of 2 cases. Br J Oral Maxillofac Surg. 2008;46:239-41.
7. Deepti S, Thara S, Ramdas K, Manoj P. Central mucoepidermoid carcinoma of mandible – a case report and review of the literature. World Journal of Surgical Oncology. 2003;1:1.
8. Ellis GL, Auclair PL. Central (primary intraosseous) mucoepidermoid carcinoma. In: Silverberg SG, Sobin LH, eds. AFIP atlas of tumor pathology, series IV: tumors of the salivary glands. Washington, DC: Armed Forces Institute of Pathology; 2008. p. 193-6.
9. Pires FR, Paes de Almeida O, Lopes MA, Elias da Cruz Perez D, Kowalski LP. Central mucoepidermoid carcinoma of the mandible: report of four cases with long term follow up. Int J Oral Maxillofac Surg. 2003;32:378-82.
10. Raut DL, Khedkar SA. Primary intraosseous mucoepidermoid carcinoma of the maxilla: a case report and review of literature. Dentomaxillofacial Radiology. 2009;38:163-8.
11. Seifert G, Sobin LH. Histological typing of salivary gland tumours. International classification of tumours. New York: Springer-Verlag; 1991.
12. Shafer WG, Hine MK, Levy BM. Text book of oral pathology. Philadelphia: WB Saunders; 1974. p. 225-31.
13. Thomas G, Pandey M, Mathew A, Abraham EK, Francis A, Somanathan T et al. Primary intraosseous carcinoma of the jaw. Report of two new cases and pooled analysis of world literature. International Journal of Oral and Maxillofacial Surgery. 2001;30:349-55.
 Corresponding author:
Corresponding author:
Shailaja Sankireddy
Department of Oral Medicine and Radiology
SGT Dental College and Hospital
Gurgaon – Haryana – India
E-mail: drsrshailaja@gmail.com
Received for publication: August 8, 2013
Accepted for publication: May 14, 2014













