Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.12 no.1 Joinville Jan./Mar. 2015
Original Research Article
Shear bond strength of brackets bonded with nanofilled flowable resins
Danielle Rodrigues MoraisI; Alexa Helena Köhler MorescaI; Estela Maris LossoI; Alexandre MoroI; Ricardo Cesar MorescaI; Gisele Maria CorrerI
I Graduate Program in Dentistry, Positivo University – Curitiba – PR – Brazil
ABSTRACT
Introduction and Objective : To evaluate the shear bond strength of brackets fixed with different materials (two light-cured nanofilled low-viscosity resins – Transbond Supreme LV and Flow Tain LV and two light-cured traditional resins – Transbond XT and Transbond Plus Color Change) after 10 min and 24 h, and to evaluate the type of failure. Material and methods : Eighty bovine incisors were selected and randomly divided into groups (n = 10) according to the material and fixation period. The brackets were bonded following the manufacturer's instructions and stored in deionized water at 37oC for 10 min or 24 h. After, the specimens were submitted to shear bond strength test at 0.5 mm/min and evaluated for adhesive remnant index (ARI). The data were submitted to Kruskal Wallis and Wilcoxon tests (p < 0.05) and the ARI scores to Chi-Square test. Results: There was a significant difference among the materials (p < 0.05) (after 10 min – Transbond XT > Transbond Plus Color Change > Transbond Supreme LV = Flow Tain LV and after 24 h – Transbond XT > Transbond Plus Color Change = Transbond Supreme LV = Flow Tain LV). There was no significant difference in resistance values between 10 min and 24 h, except for Transbond Plus Color Change. Most groups showed adhesive remaining adhered to the enamel (scores 2 and 3) without statistical significant difference (p > 0.05). Conclusion: The light-cured traditional resins showed higher resistance than the nanofilled materials. The period of fixation had no influence on the resistance for different materials, except for Transbond Plus Color Change.
Keywords: orthodontics; shear strength; orthodontic brackets.
Introduction
The success of the orthodontic treatment, among other factors, is greatly influence by accurate bracket positioning and long-term retention of these accessories3. Failures during bracket bonding can disrupt and delay the treatment, increase the cost, and hinder a correct finalization of the case. Frequent bracket rebonding can also cause damage to the enamel structure28.
The use of light-cure resins in bracket bonding can be considered a standard clinical practice24. Advances in the bonding materials had occurred over the years, especially in their composition, aiming to share the efficient adhesion to the individual needs of the orthodontic patients. Several materials are available for bracket bonding, such as resin-modified glass-ionomers, resin composites, orthodontic adhesives, flowable resins and more recently introduced nanofilled materials1,11,13,18,27.
The nanotechnology significantly contributed to the biomedical field, allowing the development of materials and structures with much reduced size: 0.1 to 100 nanometers. In Dentistry, the nanofilled resin composites show improved physical and mechanical properties, with higher fracture resistance and bond strength to enamel2,5,15,17,27.
Many clinicians have been applied flowable resins in Orthodontics1,19,24. These resins have some advantages such as no stickiness and fluid injectability9, because of their characteristics such as reduced filler content, increased diluents monomers or altered rheology. However, these characteristics may reduce the mechanical properties of these materials23. There are still few studies available that evaluate the bonding properties of these materials,1,13,24,26 with contradictory reports on the shear bond strength9,19,26.
Combining the advantages of a flowable resin and the nanotechnology, a nanofilled low-viscosity light-cured adhesive was introduced by 3M Unitek, Transbond Supreme LV. The adhesive contains a dimethacrylate polymer that modifies the rheology, allowing the material to flow under pressure, yet hold its shape after placement until light cured6. This characteristic is beneficial since the material will not slump, run, or drift from the bracket base prior to placement in the patient's mouth. Also, this material is a nanofilled resin that shows a reduction on filler size and increase on filler content (nanoclusters), allowing better mechanical properties17. However, little is known about the bonding characteristics of this material.
Another important factor is the post-fixation time that can influence the brackets bond strength and is important for the installation of the arches or accessories in the oral cavity. Thus, the aim of the present study was to evaluate the shear bond strength (SBS) of brackets fixed with different materials (two light-cured nanofilled low viscosity resins – Transbond Supreme LV and Flow Tain LV and two light-cured traditional resins – Transbond XT (control) and Transbond Plus Color Change) after 10 minutes and 24 hours. The hypothesis of this study was that there will be no difference in the SBS values among the nanofilled and traditional resins and there will be no influence of post-fixation time on SBS.
Material and methods
A total of 80 sound-extracted bovine incisors were stored in a 0.5 Chloramine T solution at 4oC for a maximum of 1 month after extraction. Teeth were randomly assigned into 8 groups (n = 10) according to the material (Transbond XT – 3M/Unitek, Transbond Plus Color Change – 3M/ Unitek, Transbond Supreme LV – 3M/Unitek and Flow Tain LV – Relience) and the post-fixation time (10 minutes or 24 hours).
The roots of the teeth were cut and discarded and the fragments of the middle third of the crowns were cut. The fragments were flattened and embedded into PVC tubes (Tigre S.A. Tubos e Conexões, Castro, PR, Brazil) using acrylic resin (Vipi Flash, Pirassununga, SP, Brazil).
For the bonding technique, the buccal enamel surface of each fragment was cleaned with fluoridefree pumice slurry, etched with 37% phosphoric acid gel (Etch-37, Bisco, Schaumburg, Ill) for 30 seconds, rinsed for 15 seconds, and dried with oilfree and moisture-free air for 20 seconds until the enamel had a faintly white appearance. After, the different materials (Transbond XT, Transbond Plus Color Change, Transbond Supreme LV and Flow Tain LV) were applied following the manufacturer's instructions on the mesh pad of individual metallic brackets (Mini Dyna-Lock "Roth" .022 - 3M/Unitek, Monrovia, CA, USA) that were positioned on the enamel surface of the specimens and pressed firmly with a Hollenback carver to expel the excess adhesive. Each bracket was subjected to a 300-g compressive force using a force gauge (Correx Co, Berne, Switzerland) for 10 seconds, after which excess bonding resin was removed using a sharp scaler. Each specimen was was light-cured for 20 seconds from the occlusal edge and 20 seconds from the gingival bracket edge, with a light-curing unit (XL300, 3M/Unitek, Dental Products), with a light intensity of 1000 mW/cm2 measured with a built-in radiometer, which was calibrated every 10 minutes to ensure consistent light intensity.
The specimens were then immersed in deionized water and maintained in a oven at 37oC during 10 minutes or 24 hours, and the a shear bond strength (SBS) test was performed.
The shear bond strength test was conducted in a universal testing machine (Model 4411, Instron Corp, Canton, Mass., USA). A mounting jig was used to align the bracket-composite-enamel interface parallel to the testing devise. A chisel-edge plunger was applied the shear load at a crosshead speed of 0.5 mm/min until failure. Bond strength values were calculated in MPa. After debonding, each specimen was examined under a stereomicroscope (Olimpus SZX9, São Paulo, SP, Brazil) to identify the location of the bond failure. The residual composite remaining on the premolar was assessed by using the adhesive remnant index (ARI), where each specimen was scored according to the amount of material remaining on the enamel surface as follows: 0 – no adhesive remaining, 1 – less than 50% of the adhesive remaining, 2 – more than 50% of the adhesive remaining, and 3 – all adhesive remaining with a distinct impression of the bracket base.
SBS data were submitted to Kruskal Wallis and Wilcoxon tests (p < 0.05). The ARI was analyzed for percentage and frequency of fracture type and submitted to Chi-Square test. Significance for all statistical tests was predetermined at p > 0.05. All of the statistical analyses were performed using BioEstat 5.0.
Results
Shear Bond Strengths
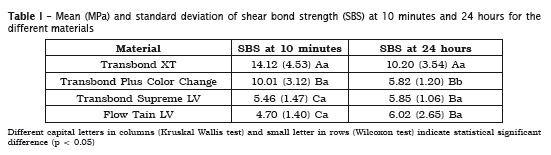
Mean bond strengths and standard deviations for each group are given in table I. Data were analyzed using Kruskal Wallis test (for comparisons among the materials in each period) and Wilcoxon test (for comparisons between 10 min and 24 hours for each material) (p < 0.05). There was a statistical significant difference among the materials at 10 min and 24 hours (p < 0.05). At 10 minutes, Transbond XT > Transbond Plus Color Change > Transbond Supreme LV = Flow Tain LV. At 24 hours, Transbond XT > Transbond Plus Color Change = Transbond Supreme LV = Flow Tain LV. The light-cured traditional materials (Transbond XT and Transbond Plus Color Change) showed the highest values compared with the nanofilled materials (Transbond Supreme LV and Flow Tain LV).
There was no statistical significant difference between 10 minutes and 24 hours except for Transbond Plus Color Change.
Adhesive Remnant Index
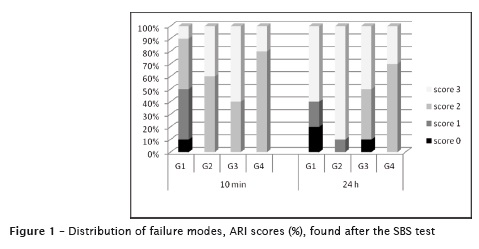
The distribution of failure modes, as expressed by ARI scores (%), is given in figure 1. According to statistical analysis (Chi-Square analysis) of the ARI scores, all of the test groups exhibited similar bracket failure modes (p > 0.05). Regardless of the bond material, bond failure occurred partly at the bracket-adhesive (resin) interface but mainly within the adhesive (resin) (score 1, 2 and 3). Enamel fractures were not observed in any of the specimens tested.
Discussion
Orthodontics has sought reliable bonding materials that are able to withstand the chewing forces and the forces generated during movement in orthodontic treatment and, do not cause any damage to the enamel after removal of the orthodontic bracket.
The minimum shear bond strength of an adhesive should be between 5.9 and 7.9 MPa to be considered adequate for clinical needs, and at least 4.9 MPa for laboratory studies20,21. When the results of this study were compared with these reference values, it was found that all materials evaluated comply with these values, considering both periods.
Besides the bond strength the bonding materials used in orthodontics should also have other features as good consistency, avoiding the displacement after positioning brackets or excesses that interfere with the thickness of the base resin, and appropriate working time.
Aiming to improve the materials characteristics, incorporating new technologies and improving their properties, the industry often develops new products for bracket bonding. One of the latest introduced features was the use of nanofilled resins. These resins that present smaller and uniformly distributed filler particles, might present greater cohesive strength to penetrate into the etched enamel and also in the bracket base resin, increasing the bond strength2,10,17. However, the results of this study showed a significant statistical difference between nanofilled low viscosity resins and traditional resins, with the nanofilled materials showing lower shear bond strength results than traditional resins. Thus, the hypothesis that there will be no differences among the materials could not be validated.
Designed for bracket bonding, Transbond XT is easily handle, which reduces working time; therefore, it has been widely used in clinical routine and also in laboratory studies as control group5,8,12,22,28,29. Studies have shown similar SBS values of this material compared with nano-hybrid composite resin, photo- and chemical-cured resins and glass ionomer cements used for bracket bonding5,7,8,12,22,28,29. However, in this study, Transbond XT showed higher SBS values than the other materials. Despite the reduction in the resistance of 27.75% after 24 hours, there was no statistical difference between the two periods, which is in accordance with other studies5,8,28.
Regarding the nanofilled resins, it was observed that both evaluated materials (Transbond Supreme LV and Flow Tain LV) had similar results, showing lower SBS values than traditional resins in both periods, except from Transbond Plus Color Change at 24 hours. Other study also found lower SBS values for nanofilled materials5, however, the authors justified the results based on the higher viscosity of the nanofilled composite resin. However, the nanofilled materials used in this study present low viscosity and supposedly should present better infiltration in both etched enamel and in bracket base. Other studies found similar SBS values of nanofilled materials compared to traditional ones13,27.
The Transbond Plus Color Change showed intermediate SBS values at 10 min, lower than Transbond XT and higher than nanofilled materials22. This material was the only one that showed significant difference in SBS values at 10 min and 24 hours, with a decrease of 41.86% in the resistance. This resin is a material characterized by its color change after curing, which facilitate the removal of excesses. According to the manufacturer, it releases fluoride and has hydrophilic characteristics, thus allowing its use on wet surfaces or contaminated by saliva. According to Tzou and Darrell25, the hydrophilic nature of this resin allows diffusion of fluorine through photoactivation crosslinked matrix in aqueous medium. That characteristic could be related to the reduction in bond strength after storage in water.
Another important feature to be observed in bonding materials is the type of failure after bracket removal. A failure in the adhesive-enamel interface (score 0) could result in a greater risk for tooth enamel damage4,14. In this study no specimen from all groups received an adhesive remnant index score of 0, indicating a minimal risk for enamel fractures. An adhesive remnant score of 3, failure at the bracket-adhesive interface was the most frequent score for all groups.
At 10 minutes, Transbond XT showed a predominance of scores 1 and 2. For the other materials there was a predominance of scores 2 and 3 (failure at the interface resin/bracket). At 24 hours, all the materials showed a predominance of failure at the bracket-adhesive interface (scores 2 and 3)8,22. This can be explained by the confinement of the resin between the mesh of the bracket, causing tensions that weaken this area.
Regarding the post-fixation time, there was no statistical significant difference between 10 minutes and 24 hours tests, except for Transbond Plus Color Change, as observed in other study21. Thus, the hypothesis that it would be no influence of postfixation time on SBS values could partially be validated. However, other studies have found greater SBS values for groups tested after 24 hours7,16. This could be related to the materials selected in other studies, e.g., glass-ionomer cements and resin-modified glass-ionomer cements that reach its final resistance after 24 hours. In this study, only resin based materials (light or chemically-cured) were used, demonstrating that after 10 minutes the polymerization of the materials allowed the material to reach an adequate resistance to be tested.
For the Orthodontist, it is important to know the materials properties, since these materials must maintain orthodontic accessories firmly adhered to the teeth during the treatment. As shown in this study, many materials of different properties and characteristics can be used for bracket bonding. However, Transbond XT seems to present some advantages, as it showed higher bond strength and predominance of score 1 type of failure, which would facilitate the removal of the resin remains from enamel surface after brackets removal.
Conclusion
Based on the results of this study, it can be concluded that:
• The light-cured traditional resins showed higher resistance than the nanofilled materials;
• The period of fixation had no inf luence on the resistance for different materials, except for Transbond Plus Color Change;
• There was a predominance of failure between the bonding material and the bracket base for all materials in both periods.
References
1. Albaladejo A, Montero J, Gómez de Diego R, López-Valverde A. Effect of adhesive application prior to bracket bonding with flowable composites. Angle Orthod. 2011;81:716-20. [ Links ]
2. Andrade MV, Oliveira LGF, Filho PFM, Silva CHV. Tendências das resinas compostas nanoparticuladas. Int J Dent. 2009;8(2):153-7.
3. Birdsall J, Hunt NP, Sabbah W, Moseley HC. Accuracy of positioning three types of self-ligating brackets compared with a conventionally ligating bracket. J Ortho. 2012;30(1):34-42.
4. Bishara S, Truelove T. Comparisons of different debonding techniques for ceramic brackets: an in vitro study. Am J Orthod Dentofacial Orthop. 1990;98:145-53.
5. Bishara SE, Ajlouni R, Soliman MM, Oonsombat C, Faffon JF, Warren J. Evaluation of a new nanofilled restorative material for bonding orthodontic brackets. World J Orthod. 2007;8(1):8-12.
6. Cinader DK, James DS. Transbond™ supreme LV low viscosity light cure adhesive: suitable for indirect bonding. Orthodontic Perspectives. Exploring Treatment Options. 2009;16:1.
7. Correr Sobrinho L, Correr GM, Consani S, Sinhoreti MA, Consani RL. Influence of postfixation time on shear bond strength of brackets fixed with different materials. Pesqui Odontol Bras. 2002;16:43-9.
8. Correr Sobrinho L, Consani S, Sinhoreti MAC, Correr GM, Consani RLX. Avaliação da resistência ao cisalhamento na colagem de bráquetes, utilizando diferentes materiais. Rev ABO Nac. 2001;9(2):157-62.
9. D'Attilio M, Traini T, Di Iorio D, Varvara G, Festa F, Tecco S. Shear bond strength, bond failure, and scanning electron microscopy analysis of a new flowable composite for orthodontic use. Angle Orthod. 2005;75:410-5.
10. Eliades T. Orthodontic materials research and applications: part 1. Current status and projected future developments in bonding and adhesives. Am J Orthod Dentofacial Orthop. 2006;130:445-51.
11. Fonseca DDD, Costa DPTS, Cimões R, Beatrice LCS, Araújo ACS. Adesivos para colagem de bráquetes ortodônticos. RGO 2010;58:95-102.
12. Giannini C, Fransciscone PAS. Resistência à remoção de braquetes ortodônticos sob ação de diferentes cargas contínuas. Rev Dental Press Ortodon Ortop Facial. 2008;13(3):50-9.
13. Goracci C, Margvelashvili M, Giovannetti A, Vichi A, Ferrari M. Shear bond strength of orthodontic brackets bonded with a new selfadhering flowable resin composite. Clin Oral Investig. 2012;27. [Epub ahead of print].
14. Habibi M, Nik TH, Hooshmand T. Comparison of the debonding characteristics of metal and ceramic orthodontic brackets to enamel: an invitro study. Am J Orthod Dentofacial Orthop. 2007;132:675-9.
15. Jandt KD, Sigusch BW. Future perspective of resin-based materials. Dent Mater. 2009;25: 1001-6.
16. Minick GT, Oesterle LJ, Newman SM, Shellhart WC. Bracket bond strengths of new adhesive systems. Am J Orthod Dentofacial Orthop. 2009;135:771-6.
17. Mitra SB, Wu D, Holmes BN. An application of nanotechnology in advanced dental materials. J Am Dent Assoc. 2003;134:1382-90.
18. Passalini P, Fidalgo TKS, Caldeira EM, Gleiser R, Nojima MCG, Maia LC. Mechanical properties of one and two-step fluoridated orthodontic resins submitted to different pH cycling regimes. Braz Oral Res. 2010;24(2):197-203.
19. Pick B, Rosa V, Azeredo TR, Cruz Filho EA, Miranda Jr WG. Are flowable resin-based composites a reliable material for metal orthodontic bracket bonding? J Contemp Dent Pract. 2010;11:17-24.
20. Reynolds IR, Von Fraunhofer JA. Direct bonding in orthodontics: a comparison of attachments. Br J Orthod. 1977;4:65-9.
21. Romano FL, Tavares SW, Ramalli EL, Magnani MBBA, Nouer DF. Análise in vitro da resistência ao cisalhamento de braquetes metálicos colados em incisivos bovinos e humanos. Rev Dental Press Ortodon Ortop Facial. 2004;9(6):63-9.
22. Romano FL, Correr AB, Correr Sobrinho L, Magnani MBBA, Siqueira VCV. Shear bond strength of metallic brackets bonded with a new orthodontic composite. Braz J Oral Sci. 2009;8(2):76-80.
23. Salerno M, Derchi G, Thorat S, Ceseracciu L, Ruffilli R, Barone AC. Surface morphology and mechanical properties of new-generation flowable resin composites for dental restoration. Dent Mater. 2011;27:1221-8.
24. Soo-Byung P, Woo-Sung SON, Ching-Chang KO, García-Godoy F, Mi-Gyoung P, Hyung-II KIM et al. Influence of flowable resins on the shear bond strength of orthodontic brackets. Dent Mater J. 2009;28:730-4.
25. Tzou S, Darrell J. Transbond plus color change adhesive: on-demand convenience with fluoride release, moisture tolerance and color change features. Orthodontic Perspective XIV. 2007;1:21-3.
26. Uysal T, Sari Z, Demir A. Are the flowable composites suitable for orthodontic bracket bonding? Angle Orthod. 2004;74:697-702.
27. Uysal T, Yagci A, Uysal B, Akdogan G. Are nano-composites and nano-ionomers suitable for orthodontic bracket bonding? Eur J Orthod. 2010;32:78-82.
28. Valletta R, Prisco D, Santis R, Ambrósio L, Martina R. Evaluation of the debonding strength of orthodontic brackets using three different bonding systems. Eur J Orthod. 2007;29:571-7.
29. Vicente A, Toledano M, Bravo LA, Romeo A, La Higuera B, Osório R. Effect of water contamination on the shear bond strength of five orthodontic adhesives. Med Oral Patol Oral Cir Bucal. 2010;15(5):820-6.
 Corresponding author:
Corresponding author:
Gisele Maria Correr
Graduate Program in Dentistry – Positivo University
Rua Pedro Viriato Parigot de Souza, n. 5.300 – Campo Comprido
CEP 81280-330 – Curitiba – PR – Brazil
E-mail: giselenolasco@up.com.br
Received for publication: May 13, 2014
Accepted for publication: October 22, 2014













