Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.12 no.2 Joinville Abr./Jun. 2015
Original Research Article
Determination of final occlusal vertical dimension by cephalometric analysis
Eduardo Christiano Caregnatto MoraisI; Bárbara Pick OrnaghiII; Ana Paula SponchiadoI; João César ZielakI; Rogério Goulart da CostaIII; Marcio José Fraxino BindoIV; Edson Alves de CamposV
I Master Program in Clinical Dentistry, Positivo University – Curitiba – PR – Brazil
II Prosthodontics, Positivo University – Curitiba – PR – Brazil
III Prosthodontics, Federal Institute for Education, Science and Technology of Paraná – Curitiba – PR – Brazil
IV Prosthodontics, Federal University of Paraná – Curitiba – PR – Brazil
V Operative Dentistry, São Paulo State University – Araraquara – SP – Brazil
ABSTRACT
Introduction: Most of techniques for determining the occlusal vertical dimension (OVD) of edentulous patients are based on soft tissues references, which lead to measurement discrepancies. Objective: To propose a method to obtain the OVD of edentulous patients during the confection of complete dentures considering the lower facial height established by Ricketts (LFHr) or the lower facial height obtained from cephalometric analysis of dentulous patients (LFHd). Material and methods: The OVD of 11 edentulous patients was determined by the association of 3 clinical methods. On each patient's bite plates a metallic ball was fixed and the patient was submitted to lateral radiographic to obtain the lower facial height (LFHe) from cephalometric analysis. Additionally, from 40 lateral cephalograms of dentulous patients the LFHd was obtained. After that, the distance between metallic balls (DMB, in mm) was calculated to verify the linear difference when LFHe was changed to LFHd or LFHr, which provided the amount of wax to be added or removed from the bite plates, establishing a new method of OVD determination. LFHe, LFHd and LFHr values were submitted to t e z statistical tests and DMB differences were analyzed by Student's t-test (α=0.05). Results: LFHr (47.0±4.0o a) was statistically higher than LFHd (44.9±5.6o b) and LFHe (43.5±3.5o b). There was statistical difference on linear discrepancies calculated between the LFHe and LFHd (1.7±4.1mm a) or LFHr (4.2±4.1mm b). Conclusion: The use of the cephalometric analysis showed to be a useful auxiliary tool in determining the intermaxillary relationship. However, this method must be associated with different clinical methods of OVD determination and it is recommended that regional references are used to calculate the linear discrepancies.
Keywords: vertical dimension; cephalometry; denture; prosthodontics; jaw relation record.
Introduction
The oral rehabilitation of edentulous patient can sometimes be impaired by the fact that all of the references used to determine the position, shape and size of the artificial teeth are essentially extra oral, such as the face contour and profile, the line between pupils, and the height of the lower facial third 20. Linear measurements, as the occlusal vertical dimension (OVD), and angular measurements, as the lower facial height (LFH), are defined based on these references.
Due to this difficulty in establishing the correct OVD for edentulous patients, many researchers developed different techniques based on muscular posture positions 21, 22, 31, facial esthetics 20, oral function 25, 28, craniometry 8, 19, cephalometry 5, 9 10, 27, 30 and electromyography 12, 14. The most used techniques for the OVD determination are those recommended by Willis (1930), by Niswonger (1934) and by Silverman (1952) 22, 28, 32. The Willis technique is based on the fact that when the patient is at maximum habitual intercuspation (MHI) with the correct OVD, the distance between the corner of the eye and the labial commissure must be equal to the distance between the base of the mentum and the base of the nose 32. During the oral rehabilitation with complete denture, at jaws relation record, this reference is determined using the Willis gauge to define the distance between the upper and lower jaws when the bite plates are in touch.
Based in clinical observations, Niswonger noticed that from the postural vertical dimension (PVD), the distance between the bases of the mentum and the nose while swallowing was 3.16 mm, ranging from 0.79 to 8.69 mm 22. Thereby, for OVD determination it would be necessary to obtain the patient's PVD and subtract the distance determined by Niswonger, named as freeway space (FS). Moreover, a phonetic method was established by Silverman, who verified that the position of the mandible during the pronunciation of sibilant sounds coincide with the OVD position, determining then a physiological method to obtain the OVD 28.
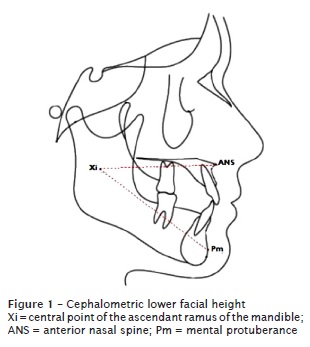
Since all of these techniques are based on soft tissues references, leading to a high incidence of measurement discrepancies generated by operators, the association of different techniques to determine the correct patient's OVD has been recommended 6. The cephalometric analysis allows the evaluation of bone growth alterations and the results of prosthodontics rehabilitations, i.e. it permits to verify the occlusal plane orientation, the curve of Spee, the anterior teeth position and the incisal guidance 7, 16, 23, 29. Different analyses were proposed for cephalometric tracings 15, 18, 26. The Ricketts analysis established that the LFH, an angular value, corresponds to the OVD 26. The LFH is composed by two lines, which connect the following cephalometric points (figure 1): (i) the central point of the ascendant ramus of the mandible (Xi) and the anterior nasal spine (ANS); and (ii) Xi and the mental protuberance (Pm). Thus, the lower facial height determines the distance between maxilla and mandible when the patient's teeth are in contact.
Recently, a research with 60 lateral radiographies of complete dentulous patients between 20 and 29 years-old established cephalometric indicators for OVD, in which the authors affirmed that the obtained data could be extrapolated to the general populations with 95% of accuracy 30. Based on that, this study sought to propose an auxiliary method of OVD determination for edentulous patients during the fabrication of complete dentures, considering the lower facial height established by Ricketts (LFHr) and by a regional population reference obtained from an archive of 40 dentulous patients (LFHd).
Material and methods
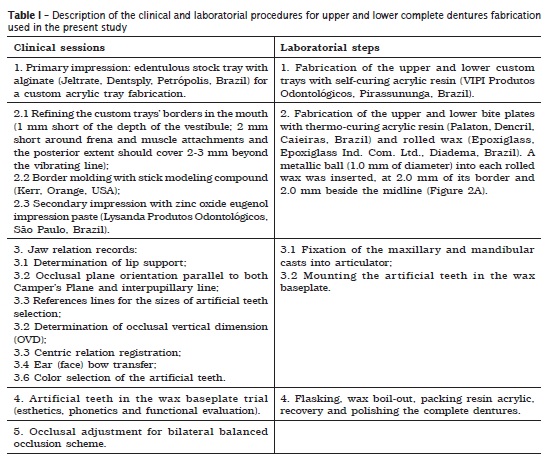
The present study was approved by the Research Ethics Committee (protocol number: 109/2008) of the Positivo University (Curitiba, Brazil) following the guidelines of the Brazilian National Health Vigilance Agency and the Brazilian National Nuclear Energy Committee. Eleven female edentulous patients, between 44 and 67 years old, with no symptoms related to any joint or muscular dysfunction, were submitted to prosthetic treatment with upper and lower complete dentures. The complete dentures fabrication followed the conventional protocol described in table I, which were composed by five clinical sessions and four laboratorial steps 24.
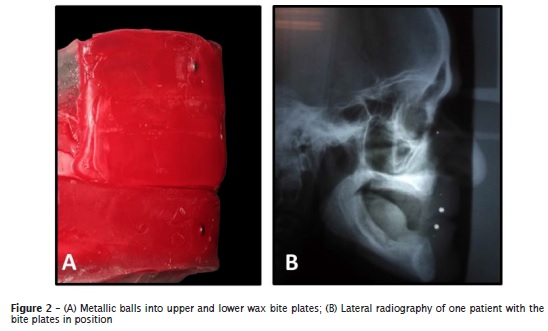
For a preliminary OVD determination, the association of three clinical methods was used: facial measurement with Willis gauge 32, postural jaw position minus 2-4 mm (FS) 3 and phonetic test 28. Both superior and inferior bite plates of each patient received a metallic ball at the midline front area (figure 2A). Wearing these plates, the patients were submitted to a lateral radiography (figure 2B) (Rotograph Plus, Villa Sistemi Medicali, Buccinasco, Italy) and the films were processed automatically (TEC X 6A, Tecmagem AS, Curitiba, Brazil). Cephalometric tracings were done with the aid of a computer program (OrtoManager, SoftManager, Curitiba, Brazil) in order to obtain the lower facial height for this edentulous group (LFHe).
Lateral cephalograms from the Posit ivo University's archive (Curit iba, Brazil) of 40 patients with Ricketts analysis were selected. Females, with 20 years or older, less than five missing posterior teeth, with no symptoms related to any joint or muscular dysfunction and who had not been treated previously by orthodont ics were the included exams. The average of all LFH was calculated to determine the dentulous regional population lower facial height (LFHd).
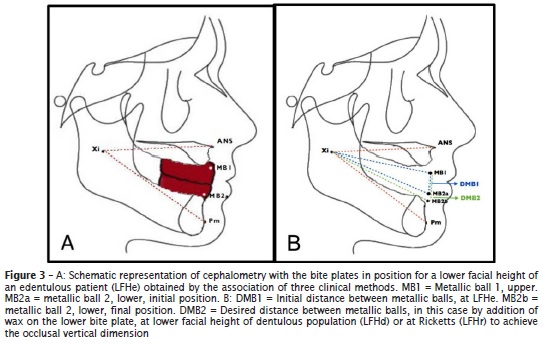
From the cephalometric tracing of LFHe group (Figure 3), the distance between the inserted metallic balls (DMB) was recorded (DMB1). New DBM measurements were found simulating the LFHd and LFHr conditions for each edentulous patient (DMB2). Linear DBM discrepancies at LFHd and LFHr were calculated. The result with the lowest linear discrepancy was suggested for the final DBM. Addition or removal of wax from the inferior bite plates were done to match the final DBM, and finally to achieve the ultimate OVD (figure 3).
The angular discrepancy among LFHe, LFHd and LFHr data was analyzed using the t and z statistical tests. The linear (DBM) discrepancy values were analyzed using the Student's t-test. All statistical tests were done at a 5% significance level.
Results
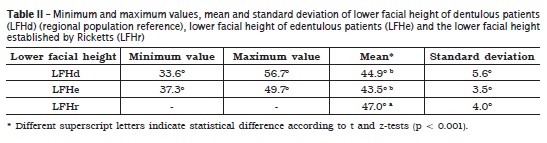
The table II shows the minimum and maximum values, the mean and the standard deviation of LFHd, LFHe and LFHr. There was no statistical difference between the LFHd and LFHe means (p = 0.426). However, the LFHr was statistically different from LFHe and LFHd (p < 0.001).
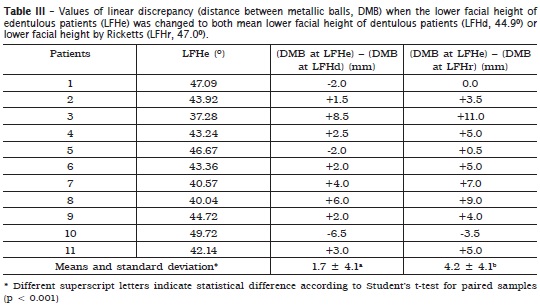
The mean DMB at LFHe was 18.8 ± 6.2 mm. The l inea r discrepancies ca lculated between the LFHe and LFHd or LFHr were 1.7 ± 4.1a mm or 4.2 ± 4.1b mm, respectively, which were statistically different (p < 0.001) (table III).
Discussion
It has been proposed that OVD alterations must be done gradually in order to establish a new mandibular position in which the patient develop the functions normally 17. A high OVD decrease might cause displacement of the mandible condyle and articular disk, clicks and articulation pain, whereas the accentuate OVD increase could generate phonetic and occlusal interferences by invasion of the FS 1, 2, 9, 11, 17. Therefore, specific population references should be obtained to be used as a basis for the dental treatment planning of each patient. Also, individual factors such as physiology, genetics and appearance, should be taken into account 11.
The angle that determines the lower facial height in Ricketts analysis determines an upper and a lower references that established of a vertical line when the teeth are in occlusion, named OVD. The literature considers this angle as one of the most scientific reference for calculating the OVD 7, 23. However, it should be complemented by other clinical methods, such as facial measurement with Willis gauge, 2-4 mm less than postural jaw position (FS) and the phonetic test 7.
In a previous study, a standard LFH of 44.5º ± 4.8 was established for females of 18 years old 13. This value was different from that established by Rickets (47.0o ± 4.0), which determines the standard for Caucasian children of different ages and both genders 26. These observations corroborate with the fact that the global standards should be moderately used or individualized standards for a specific geographic region should be determined to align the rehabilitation treatment according to the patients' own environment 13, 30. For this reason, the present study also considered the LFHd to accomplish clinical results with local considerations.
No complaints were made by the rehabilitated edentulous patients, regarding signs or symptoms related to articulation problems or OVD alterations. The metallic balls added into each bite plate created two new radiographic points that could be analyzed in cephalometry. The absence of statistical difference between LFHd and LFHe means was related to the fact that the selection of the patients of both groups showed a similar craniofacial profile.
In the present study, LFHe was statistically di f ferent from LFHr. The same was found previously, in which the LFH obtained after the rehabilitation (45.0º ± 6.7) was also lower than LFHr 9. Probably, the reason is that vertical and sagittal maxillomandibular relationship changes occur in patients wearing dentures for an extensive period 9.
The placement of metallic balls into each rolled wax allowed for the clinical measuring of the distance between them, facilitating the adaptation of a desired intermaxillary relation, using LFHd and/or LHFr as parameter. For example, during a second bite plate registration one subject that first presented the LFHe as 42.1° and the DMB as 12.0 mm, in order to match to LFHd (44.9°), the new DMB was achieved with the lowest linear discrepancy, without the need of a new lateral radiograph. Table III shows that the LFHd reference was used as the LFH parameter for OVD determination of 8 patients, and the LFHr reference value was used only for 3 individuals. Therefore, these results support the fact that the measures of a specific population can be relevant to the OVD reestablishing.
Conclusion
The use of the cephalometric analysis showed to be an important auxiliary method for jaw relation record during rehabilitative treatment using complete dentures, due to the bone bases references which allowed for a more precise determination of OVD. However, this method must be associated to different clinical methods, and the use of regional population reference is recommended to calculate the linear discrepancies in the determination of the ultimate OVD.
References
1. Abduo J, Lyons K. Clinical considerations for increasing occlusal vertical dimension: a review. Aust Dent J. 2012 Mar;57(1):2-10. [ Links ]
2. Abduo J. Safety of increasing vertical dimension of occlusion: a systematic review. Quintessence Int. 2012 May;43(5):369-80.
3. Ackermann F. Le mechanisme des machoires: naturelles et artificielles. Paris: Masson; 1953.
4. Atwood D. A critique of research of the rest posit ion of the mandible. J Prosthet Dent. 1966;16:848-54.
5. Bassi F, Rizzat t i A, Schierano G, Pret i G. Evaluation of the utility of cephalometric parameters in constructing complete denture. Part II: placement of anterior teeth. J Oral Rehabil. 2001 Apr;28(4):349-53.
6. Carossa S, Catapano S, Scotti R, Preti G. The unreliability of facial measurements in the determination of the vertical dimension of occlusion in edentulous patients. J Oral Rehabil. 1990;17:287-90.
7. Chaconas SJ, Gonidis D. A cephalometric technique for prosthodont ic diagnosis and t reatment planning. J Prosthet Dent. 1986 Nov;56(5):567-74.
8. Chou TM, Moore DJ, Young Jr L, Glaros AG. A diagnostic craniometric method for determining occlusal vertical dimension. J Prosthet Dent. 1994 Jun;71(6):568-74.
9. Çiftçi Y, Kocadereli I, Canay S, Senyilmaz P. Cephalometric evaluation of maxillomandibular relationships in patients wearing complete dentures: a pilot study. Angle Orthod. 2005 Sep;75(5):821-5.
10. Domitti S, Donsani S. Regressive formula to determine vertical dimension in the edentulous. Aust Dent J. 1978;23:196-8.
11. Edwards CL, Richards MW, Billy EJ, Neilans LC. Using computerized cephalometrics to analyze the vertical dimension of occlusion. Int J Prosthodont. 1993 Jul-Aug;6(4):371-6.
12. Feldman S, Leupold R, Staling L. Rest vertical dimension determined by electromyography with biofeedback as compared to conventional methods. J Prosthet Dent. 1978;40:216-9.
13. Feo PS, Interlandi S, Martins DR, Almeida RR. Cephalometric study of thickness and height of the soft tissue in the lower face. Estomatol Cult. 1971 Jul-Dec;5(2):178-85.
14. Gross M, Nissan J, Ormianer Z, Dvori S, Shifman A. The effect of increasing occlusal vertical dimension on face height. Int J Prosthodont. 2002;15:353-7.
15. Jacobson A. The "Wits" appraisal of jaw disharmony. Am J Orthod. 1995;67(2):125-38.
16. L'Estrange P, Vig P. A comparative study of the oclusal plane in dentulous and edentulous subjects. J Prosthet Dent. 1975;33:495-503.
17. Mays KA. Reestablishing occlusal vertical dimension using a diagnostic treatment prosthesis in the edentulous patient: a clinical report. J Prosthodont. 2003 Mar;12(1):30-6.
18. McNamara JA. A method of cephalometric evaluation. Am J Orthod. 1984;86(6):449-69.
19. Misch C. Clinical indications for altering vertical dimension of occlusion. Objective vs subjective methods for determining vertical dimension of occlusion. Quintessence Int. 2000;31:280-2.
20. Mohindra NK, Bulman JS. The effect of increasing vertical dimension of occlusion on facial aesthetics. Br Dent J. 2002 Feb 9;192(3):164-8.
21. Nairn R. Interrelated factors in complete denture construction. J Prosthet Dent. 1965;15:19-24.
22. Niswonger M. The rest position of the mandible in centric relation. JADA. 1934;21(9):1527-82.
23. Orthl ieb JD, Laurent M, Laplanche O. Cephalometric estimation of vertical dimension of occlusion. J Oral Rehabil. 2000 Sep;27(9):802-7.
24. Paffenbarger GC, Woelfel JB, Sweeney WT. Resins and technics used in constructing dentures. Dent Clin North Am. 1965 Mar;23:251-62.
25. Pound E. The vertical dimension of speech: the pi lot of occlusion. J Cal i f Dent Assoc. 1978;6:42-7.
26. Ricketts R. Planning treatment on the basis of facial pattern and an estimate of its growth. Angle Orthod. 1957;27:14-37.
27. Rodriguez Gonzalez MA, Casado Llompart JR, Ballina Peruyera A. Cephalometric analysis: study and use in the diagnosis and treatment of the completely edentulous. Rev Esp Estomatol. 1985 Jul-Aug;33(4): 249-62.
28. Silverman M. The speaking method in measuring vertical dimension. J Prosthet Dent. 1952;85:427-31.
29. Strajnic L, Sinobad DS. Application of cephalometric analysis for determination of vertical dimension of occlusion – a literature review. Med Pregl. 2012 May- Jun;65(5-6):217-22.
30. Strajnic L, Stanisic-Sinobad D, Markovic D, Stojanovic L. Cephalometric indicators of the vertical dimension of occlusion. Coll Antropol. 2008 Jun;32(2):535-41.
31. Toolson L, Smith D. Clinical measurement and evaluation of vertical dimension. J Prosthet Dent. 1982;47:236-41.
32. Willis F. Esthetics of full denture construction. JADA. 1930;17(4):636-41.
 Correspondence:
Correspondence:
Bárbara Pick Ornaghi
Rua Emiliano Perneta, 466 – sala 605 – Centro
CEP 80420-080 – Curitiba – PR – Brasil
E-mail: barbara@pick.com.br
Received for publication: February 2, 2015
Accepted: February 23, 2015













