Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.12 no.2 Joinville Abr./Jun. 2015
Original Research Article
Headaches and pain referred to the teeth: frequency and potential neurophysiologic mechanisms
Omar Franklin MolinaI; Bruno Ricardo Huber SimiãoII; Marcio Yukio HassumiIII; Rise Consolação Iuata RankIV; Fausto Félix da Silva JuniorV; Adilson Alves de CarvalhoVI
I School of Dentistry (Orofacial Pain), UNIRG University Center – Gurupi – TO – Brazil
II School of Dentistry (Prosthodontics), UNIRG University Center – Gurupi – TO – Brazil
III School of Dentistry (Periodontics), UNIRG University Center – Gurupi – TO – Brazil
IV School of Dentistry (Pedodontics), UNIRG University Center – Gurupi – TO – Brazil
V School of Dentistry (Preventive Dentistry), UNIRG University Center – Gurupi – TO – Brazil
VI Private Practice – Goiânia – GO – Brazil
ABSTRACT
Objective: To assess frequency of pain referred to the teeth in occipital neuralgia, migraine and tension-type headache. Material and methods: 153 patients presenting with bruxing behavior and craniomandibular disorders (CMDs). Clinical examination, questionnaires, palpation, criteria for CMDs, bruxing behavior (BB), occipital neuralgia (ON), migraine (MIG), tension-type headache (TTH) and pain referred to the teeth. Results: Mean ages in the ON, MIG and TTH patients and controls were about 38.0, 37.0, 33.0 and 36.6 years, respectively (p = 0.17). The frequencies of dental pains in the subgroups ON and MIG were 37.1% and 25% (p = 0.52), ON and TTH, 37.1% and 18.6% (p = 0.03), ON and Controls 37.1% and 6.7% (p = 0.006), MIG and TTH 25% and 18.6% (p = 0.51), MIG and Controls 25% and 6.6% (p = 0.16) and TTH and controls 18.6% and 6.7% (p = 0.15). The frequencies of pain referred to the teeth decreased from the ON to the MIG, and then to the TTH and Control groups (x-square for independence p < 0.002, x-square for trends p < 0.001). Conclusion: The ON subgroup demonstrated the highest frequency of dental pain referred to the teeth. This frequency increased with the severity of pain. Neurophysiological mechanisms may explain higher frequency of referred pain associated with the severity of headache.
Keywords: occipital; tension-type headache; common migraine; pain.
Introduction and literature review
Craniomandibular disorders (CMDs) are a heterogeneous group of pathologies affecting the stomatognathic system and related structures, whose complex and diversified etiology generate several diagnostic and taxonomic problems and with signs and symptoms which in some way are associated with psychosomatic disorders 10. Major CMDs signs and symptoms include pain, impairment of jaw movements, joint sounds and headaches 17. Occipital neuralgia (ON) is a rare neuralgic pain in the distribution of the sensory branches of the cervical plexus, usually described as a paroxystic, stabbing pain in the distribution of the greater occipital nerve (GON), lesser occipital nerve (LON) and/or third occipital nerve and presents tenderness over the affected nerve 11.
ON is a type of headache that describes the irritation of the GON and the signs and symptoms associated with it 7. Common causes of ON are trauma, neoplasms, infection, aneurysms involving the affected nerves 30, head injury, direct occipital nerve trauma, neuroma formation, compression of upper cervical roots 34, degenerative changes, congenital abnormalities, compression of the nerve and other factors 3.
Migraine (MIG) is a very common, chronic, unremitting, painful disorder characterized by headache attacks lasting 4-72 hours, mostly with unilateral location, throbbing or pulsating in character, moderate to severe in intensity, sometimes accompanied by autonomic symptoms 35, and usually described in the frontal, temporal, and/ or parietal areas of the head 35. MIG attacks are aggravated by physical activity and are usually associated with nausea, vomiting and / or sensitivity to light and sound. Most people with MIG have a family history of headache, and the disorder affects primarily women 15. Each pain attack is usually more intense in the frontal, temporal and ocular regions before spreading to the parietal and occipital areas, but any region of the head or face may be affected 22.
Tension-type headache (TTH) is a headache type lasting 30 minutes to 7 days, usually reported as pressure or a tight sensation of mild to moderate intensity, typically on both sides or around the head in a "band-like" distribution. The pain in TTH is not exacerbated by physical activity and there are no other symptoms associated with this headache 15. TTH is characterized by a pressure or a band-like sensation around the head. This pain is described as unbearable, dull, obtuse, and tormenting, that builds steadily, and develops gradually, persistently, but recedes following bathing and physical exercise 33.
The orofacial region is the most frequent site for patients to seek medical attention for pain, a symptom which is commonly mistaken for a toothache, but other pains of the head and neck may mimic odontogenic pain 33. Patients with no dental causes of orofacial pain will also present themselves seeking a dental solution for their symptoms which may closely mimic toothaches 2. The neurovascular pain of MIG may present in a facial distribution, in which case, it may be confused with odontogenic pain or pain related to either masticatory muscle myalgia, bruxing behavior (BB) or to temporomandibular joint (TMJ) arthralgia 15. Neurovascular pains or headaches may also present as a variant involving the orofacial region, hence mimicking a toothache. There are only a few reported cases of patients presenting with oral, dental pains and concomitant migraine 33. Because the C2 ganglion interconnects with the trigeminal ganglion in the brainstem, ON may cause referred pain to one or many trigeminal nerve (TN) branches 13.
Because it has been reported that some headaches produce pain referred to the teeth, but, there is scarcity of studies in this field, specifically regarding the diagnosis and treatment of headaches 32 and the neurophysiological mechanisms of pain referral to the teeth are not well understood, the objective of this investigation is twofold:
1. Evaluate the frequency of dental pains referred to the teeth in a group of headache individuals, and in subgroups of those with ON, MIG and TTH;
2. Use the current literature to evaluate the neurophysiologic mechanism of pain referred to the teeth.
Methods
Sample
From a large group of individuals (N = 153) presenting with CMDs and BB referred consecutively over a period of 10 years to UNIRG-School of Dentistry, Division of Orofacial Pain and Occlusion, for diagnosis and treatment, those presenting ON (n = 35), MIG (n = 16) and TTH (n = 102), were selected and their charts were reviewed retrospectively so as to get data about the presence of dental pains and clinical characteristics of their pain disorder. Only one expert in the field (OFM), reviewed patients' charts. The investigation was approved by the Ethical Committee of the Dental School (005-13).
Procedure
Patients were classified as presenting CMDs if they demonstrated at least three of the following signs, symptoms or behaviors 18: A complaint of pain in the masticatory muscles and/or TMJs, difficulties to perform normal jaw movements, tenderness to palpation of joint and muscles, joint noises, seeking active treatment for their complaint and headaches usually of CMD origin. Because we have identified more or less 25 signs and symptoms directly associated to BB 19, we used such signs/ symptoms to classify patients as presenting CMDs and mild, CMDs and moderate, CMDs and intense and CMDs and extreme BB. The comprehensive protocol used in the current study contains a number of descriptors reported and used by patients presenting different headache pains including those evaluated in the current study.
Criteria to consider the presence of ON in CMDs and BB individuals were the presence of symptoms described previously 3, 29. Briefly: Unilateral or bilateral, paroxystic, lancinating and very severe pain described as burning, throbbing, shooting/ jabbing, electric shock-like, continuous and/or intermittent, presenting with a pain generating area in the sub-occipital region associated with a tender local area, pain reproduced with pressure over the pain generating area, occurring in the occipital/sub-occipital area and usually radiating to the vertex, frontal, orbital and peri-orbital regions. Inclusion criteria for MIG were pain described as unilateral, severe, constant, and always throbbing or pulsating, pain that increases with physical effort and a pulsating characteristic reported more frequently during severe MIG episodes 29.
Criteria for TTH were delineated in a previous investigation 19, briefly: Pain described as bilateral, reported in the temporal, frontal and occasionally in the occipital/sub-occipital region, usually dull, constant, pressing and constricting, presence of nausea much more frequently than vomiting and pain described as mil/moderate and rarely as severe. A short questionnaire was used to record all painful sites in the head, face, neck and teeth. The presence of multiple pains was diagnosed as such when four or more painful sites in the aforementioned anatomic areas were reported by patients.
Criteria to consider the presence of nonodontogenic referred dental pains were absence of dental pathology explaining the toothache, pain described as constant, dull, non/throbbing, patients report of previous examination by at least two dental surgeons reporting no dental pathology explaining the pain, patients' report that toothache occurred more frequently when headache was more intense or extremely severe and a positive correlation between an anatomic site, for instance, anterior temporal region, masseter region, occipital and sub-occipital area and pain in the anterior and/or posterior teeth in the maxilla or in the mandible.
Exclusion criteria
Criteria to exclude CMDs and BB patients presenting ON, TTH and MIG from participating in this investigation were the presence of severe psychiatric disorders, severe neurologic disease (for instance, Parkinson disease), intellectual difficulties to respond properly to questionnaires, absence of CMDs and/or BB signs and symptoms, and presence of dental pains described as extremely intense, shooting and electric-shock like suggesting the presence of any neuralgic disorder and or the presence of pulp disease. Statistical methods deemed to be appropriate for this investigation included Kruskal-Wallis ANOVA, X-square analysis of trends and Fisher's exact test.
Results
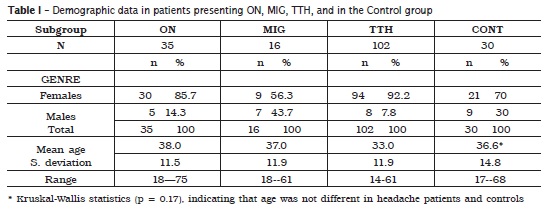
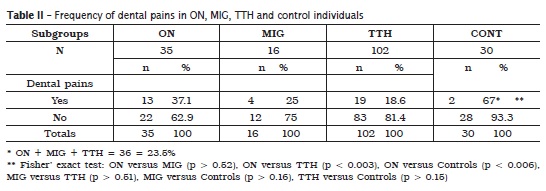
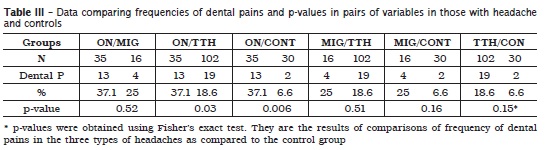
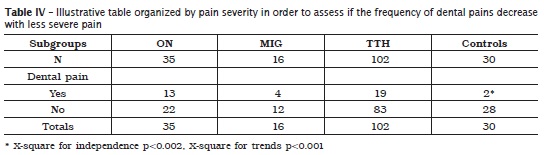
Females predominated in these subsets of individuals presenting CMDs and three types of headaches: ON (85.7%), MIG (56.3%) and TTH (92.2%). Mean ages were about 38.0 37.0, 33.0 and 36.6 in the subgroups with headaches (ON, MIG, TTH) and in the control subgroup, respectively (Kruskal-Wallis statistics p = 0.17, table I). The frequency of dental pain was about 37.1% in the ON subgroup, 25.0% in the MIG subgroup, 18.6% in the TTH subgroup and 6.7% in the control one. The total frequency of pain referred to the teeth in the three headache groups was about 23.5% (table II).There were no statistically significant differences in the frequency of pain referred to the teeth when comparing the subgroups ON+MIG (p > 0.52), MIG and TTH (p > 0.51), MIG and CONT (p > 0.16), and TTH and CONT (p > 0.15), however, there were statistically significant differences in the frequencies of pain referred to the teeth when comparing the pairs of subgroups ON and TTH (p < 0.03), and ON and CONT (p < 0.006), based on Fisher's exact test (table III). When the subgroups were organized by the severity of pain (ON more severe than MIG, MIG more severe than TTH, TTH more severe than pain in the control group), the frequencies of dental pains decreased with less severity of headache pain and the difference was statistically significant (X square for independence p < 0.002, X-square for trends p < 0.001) (table IV).
Discussion
Frequency of dental pains in headache individuals
One objective of this investigation was to assess the frequency of pain referred to the teeth in a group of 153 individuals presenting ON, MIG or TTH. In the current investigation, we report a frequency of 23.5% dental pains associated with headaches. Data in the current study are different from those from another research 2, indicating that 12.2% of patients with orofacial pain reported dental pains. A different methodology may account for this difference, for instance, researchers in that study did not report nor types neither frequencies of headache in orofacial pain patients. However, those investigators reported that it is common for pain in the orofacial region to be mistaken for a toothache and that other pains in the head and neck may mimic odontogenic pain 2.
Many headaches have thei r source i n neuromuscular disorders in adjacent cervical structures. It is known that many musculoskeletal disorders, neuropathic and vascular headaches may mimic odontalgia 8. The frequency of pain referred to the teeth was high in the current study, thus, such an outcome is in line with a previous investigation reporting that toothache is probably the most common form of headache 15. Neurovascular pains or headaches are common complaints and headaches may also present as a variant involving the orofacial region, hence mimicking toothache 2.
Frequency of dental pain in ON
In the current study, we found a frequency of 37.1% of pain referred to the teeth in those individuals presenting with ON. This outcome is different from the frequency of 15% of pain referred to the teeth in cases diagnosed with some type of cranial neuralgias in a previous investigation 13. The difference in the frequency of pain referred to the teeth, may be explained by a different collecting data method, for instance, in Linn and associates' study 13, researchers evaluated toothaches in patients referred to an endodontic practice presenting with orofacial pains whereas, we evaluated orofacial pain and headache patients referred to a CMD unit. Nevertheless, such researchers stated that neuralgic pains may mimic closely acute toothache of pulp origin.
The outcome in the current study has partial support in two investigations 26, 31, indicating that ON may cause symptoms similar to migraine, pain in the face and referred pain to the upper molars. Moreover, in the clinical setting, it is not uncommon to observe patients in whom the cause of their toothaches is a neuralgic disorder 13. Neuralgic pain follows the path of a nerve, and such a pain is a diagnostic dilemma for the dentist 30. ON is currently considered a neuropathic disorder and one investigation 14, indicates that neuropathic tooth pain can present exclusively intra-orally in the absence of obvious infection or trauma. Moreover, neuropathic pain in the head and neck region is common and can result in multiple unnecessary dental treatments.
Frequency of dental pains in migraine
Even though the sample size in migraine patients was small, data indicated a frequency of 25% migraineurs reporting pain referred to the teeth. Findings in the current investigation have some support in another study 35, indicating that facial pain including toothaches may occur in 29.8% of migraine individuals. It may be that very intense pain in headache individuals is more likely to contribute to pain in the teeth and to be associated with central sensitization. Such an assumption is supported by one case report investigation, indicating that unilateral dental pain was associated with very severe headache 9. There are reasons to believe that many headache types can produce referred pain to the teeth. Thus, it is not uncommon to observe unilateral and ipsilateral tooth pain in patients presenting MIG 1.
The outcome in the current investigation is also supported by a recent study 15, indicating that MIG may present in a facial distribution in which case may be confused with odontogenic mechanisms. Additional support for the findings from the current research comes from one study 22, defending the notion that any region of the head or face may be affected in patients with MIG, including the parietal, upper and lower jaw, teeth, malar area and the anterior upper neck. Many MIG patients report typical features of a MIG attack with atypical pain in the face in one or both of the lower TN distributions, thus, headache, may occur together with pain in any structure in the lower half of the face 35. Additionally, there are reasons to believe that toothaches associated with a MIG disorder are more likely to occur in the maxilla than in the mandible 2.
Frequency of dental pains in TTH
In the current investigation we report a frequency of 18.6% of pain referred to the teeth in those CMD individuals presenting with TTH. Thus, the outcome in the current study is supported at least in part by one investigation 13, reporting that TTH may also cause pain referred to the teeth. Patients with a muscular problem usually myofascial pain, TTH or chronic neck disorders, usually complain of referred pain to the teeth and to the alveolus and the pain usually involves multiple teeth 12. In one investigation, 37% of patients diagnosed with a muscular orofacial pain had previously undergone endodontic or exodontic treatment in an attempt to alleviate their pain 2. The current study reinforces the idea that some MPD and myogenic headaches may cause pain referred to the teeth.
Many TTH patients present with many cervical and facial masticatory/non masticatory muscles trigger points that cause referred pain to the frontal, temporal, facial and oral structures including the teeth, or even to other anatomic regions. In such patients, trigger points in the trapezius, sternocleidomastoid, temporalis and masseter muscles, causing referred pain are observed very frequently. Thus, pain referred to the teeth may occur more or less frequently in TTH patients. These assumptions are supported by one investigation 2, asserting that the temporalis, sternocleidomastoid and trapezius muscles, often refer pain to the maxillary teeth (temporalis muscle), posterior upper and lower teeth (masseter), oral structures and the forehead (sternocleidomastoid muscle), mandible or temporalis muscle area (trapezius).
The frequency of dental pains decreased with less severe pain
In the current study, we al located the experimental subgroups in decreased order of severity of headache pain based on data from the review of the literature and patients' report about the severity of their pain. We found that the frequency of pain referred to the teeth decreased from the ON to the MIG, to the TTH and to the Control group and this trend was statistically significant. It may be that increased duration and intensity of pain is associated with central excitatory effects, enhanced neurophysiological connections outside the normal receptive field with adjacent neural structures including with trigeminal nerve branches. These mechanisms cause referred pain to peripheral structures including those innervated by the fifth cranial nerve. These observations are echoed by one study 35, indicating that a longer lasting history of migraine and increased pain intensity may enhance activation of the trigeminal autonomic system.
Pain in the area of the GON is more intense as compared to pain in MIG, TTH and pain from the TMJ and adjacent structures. More intense pain may be an important factor contributing to a higher frequency of pain referred to the teeth and enhancing synaptic connections and thus, increasing local and central sensitization. This assumption has partial and indirect support in one investigation 26 demonstrating that massaging over the GON ipsilateral to migraine causes significant pain reduction in territories innervated by the trigeminal and cervical nerves. More severe pain in ON patients is more likely to produce pain in multiple anatomic areas including the teeth as ON is related to superficial cutaneous sensitization which is considered an indicator of central sensitization and more chronic pain 29. There is evidence that neuralgic pain due to aberrant function or structural abnormalities in one branch in the TN system, may give rise to referred pain to a second upper molar 21. Thus, there are reasons to believe that more intense craniofacial pain is more likely to produce referred pain to adjacent and/or distant anatomic structures including the teeth. Because ON is a neuropathic severer pain, it is more likely to sensitize adjacent neural structures and produce pain referred to distant structures in the head and face 20.
Mechanisms of referred pain to the teeth in headache patients
The close association between sensory, motor fibers of some spinal nerves and sensory fibers or adjacent nucleus of the TN allows for exchange of sensory and motor information from the trapezius, sternocleidomastoid and other cervical muscles to converge in the trigeminal and cervical nucleus, resulting in the referral of pain to TN sensory fields of the head and face including the teeth 4. The presence of such neurophysiological connections is exemplified by the fact that GON blocks interventions to alleviate ON and cervicogenic headache may reduce pain in 14% patients presenting signs and symptoms of TTH and in 54.5% of patients presenting with cervicogenic pain 5 indicating that not only pain in areas innervated by some cervical nerves may be alleviated, but also pain in structures innervated by the TN.
The convergence of the upper cervical nerves and trigeminal sensory afferents at the trigeminalcervical complex is well documented and there is neurophysiological coupling between the craniofacial and cervical systems 16. Because the C2 ganglion interconnects with the trigeminal ganglion in the brainstem, ON can refer pain to any anatomic area innervated by the TN, especially the retro-orbital area. These neurophysiological mechanisms in ON seem to operate in the same way in patients presenting with MIG and TTH. It is known that migraine headache is characterized by increased sensitization of the trigeminovascular system. Moreover, the longer the pain experience, there is enhanced peripheral and central sensitization associated to decreased effect iveness of the descending inhibitory system. Maladaptation of the trigeminal nociceptive system may be induced by repetitive nociceptive activation, trigemino-spinal sensitization and impaired descending inhibitory pain control 23. A number of peptides including calcitonin gene related peptide (CGRP) can contribute to enhanced activation of the trigeminal vascular system 6.
Diagnostic and therapeutic implications
Even though ON, MIG and TTH are different clinical disorders, there is substantial overlap of symptoms, thus, the diagnostic is a challenge for many practitioners. Consequently, both clinicians and orofacial pain specialists need to dedicate effort and time to establish the differential diagnosis of non-odontogenic toothache. The frequency of both endodontic treatment and extraction of teeth is very high in orofacial and endodontic patients in whom the differential diagnosis has not been established previously 24. Careful attention is necessary to take the clinical history to reconstruct all parameters needed for diagnosis purposes such as frequency, intensity and duration of pain attacks so as to make it possible to distinguish between some common headache types 27. Complete diagnosis and identification of all the factors associated with underlying pathosis is the key to successful treatment 28. Chronic headaches and facial pains syndromes are an indication for intervention of physicians of numerous medical specialties, thus, interdisciplinary diagnostic and therapeutic approach is warranted 25.
There is substantial evidence indicat ing that myogenic mechanisms are involved in the development of many headache disorders and that local anesthesia to trigger points and or to pain generating zones is a well-established and recognized therapeutic procedure. In the case of ON, GON local anesthesia is thought to interfere with the subsequent sensitization, a concomitant of acute headache attacks, modulating the excitability of second-order neurons which receive constant input from trigeminal and cervical afferents 11.
There is considerable neurophysiological input to the TN subnucleus caudalis, from both peripheral orofacial and cervical structures in those patients presenting with cervical disorders and pain radiating to TN innervated structures. Germaine to this issue, is one study indicating that local superficial anesthesia to selective cervical structures may alleviate dental pain in a significant proportion of patients 16. Thus, local anesthesia may be incorporated as an effective mode of therapy in the treatment of some craniofacial disorders, including muscle pains referred to the face, headaches and toothaches originating in myofascial structures. Undoubtedly, local anesthesia and other modes of therapy to manage some craniofacial and headache disorders, should be tailored appropriately and carefully for each individual case. Conclusions: Within the limitations of this investigation we conclude that higher frequencies of pain referred to the teeth were observed in those individuals presenting with occipital neuralgia and migraine. Because ON is characterized by very severe, more diffuse, protracted pain, it may be that such characteristics of that pain combined with convergence or spreading of nociceptive input to the trigeminal system and with increased central sensitization may be implicated in the mechanisms of pain referred to the teeth.
References
1. Alonso AA, Nixdorf DR. Case series of four different headache types presenting as tooth pain. J Endod. 2006;32:1110-3. [ Links ]
2. Balasubramanian R, Turner LN, Fischer D, Klasser GD, Okeson JP. Non-odontogenic toothache revisited. Open J Stomatol. 2011;1:92-102.
3. Barma S, Hashmi M. Occipital neuralgia. Pain Management Rounds. 2004;1:1-6.
4. Biondi DM. Cervicogenic headache: diagnostic evaluation and treatment strategies. Pain Management Rounds. 2004;1:1-6.
5. Bovin G. Cervicogenic headache, migraine without aura and tension-type headache: diagnostic blockade of the greater occipital and supra-orbital nerves. Pain. 1992;51:43-8.
6. Capuano A, Greco C, Navarra P, Tringali G. Peptide (CGRP) and activation of trigeminal vascular system in an in vivo experimental model of nitroglycerin-induced sensitization. European Journal of Pharmacology. 2014;740:97-102.
7. Comley L. Chiropractic management of greater ON. Clin Chiropract. 2003;6:120-8.
8. Czerminsky R, Benoliel R, Sharav Y. Odontalgia in vascular orofacial pain. JOP. 1999;13:196-200.
9. DeBruyne F, Herroelen L. Migraine presenting as chronic facia l pa in. Acta Neurol Bel g. 2009;109:235-7.
10. Fantoni F, Salvetti G, Manfredini D, Bosco M. Current concepts on the functional somatic syndromes and temporomandibular disorders. Stomatol Baltic Dental Maxillofac J. 2007;9:3-9.
11. Jürgens JP, Muller P, Seedorf H, Rigelsberger J, May A. Occipital nerve block is effective in craniofacial neuralgia but not in idiopathic persi stent facia l pa in. J Headache Pa in. 2012;13:199-213.
12. Kim ST. Myofascial pain and toothaches. Aust Endod J. 2005;31:106-10.
13. Linn J, Tranton I, Teo N, Thanigaivel R, Goss AN. The differential diagnosis of toothache from other orofacial pains in clinical practice. Aust Dent J. 2007;52:100-4.
14. Matwychuk MJ. Diagnostic challenges of neuropathic tooth pain. JCDA. 2004;70:542-6.
15. Mehta SA, Epstein JB, Greene C. Recognition and management of headache. JCDA. 2006;71:835-9.
16. Mellick LB, Mellick GA. Treatment of acute orofacial pain with lower cervical intramuscular bupivacaine injection. J Orofac Pain. 2008;22:57-64.
17. Molina OF, Santos J, Nelson SJ, Nowlin T. A clinical study of specific signs and symptoms of CMD in bruxers classified by the degree of severity. Cranio. 1999;17:268-79.
18. Molina OF, Peixoto MG, Eid NL, Aquilino RN, Rank RC. Headache and bruxing behavior types in craniomandibular disorders (CMDs) patients. Rev Neurociênc. 2011;19:449-57.
19. Molina OF, Santos ZC, Marquezan RF, Silva N, Gama KR. A comprehensive method to classify subgroups of bruxers in temporomandibular disorders (TMDs) individuals: frequency, clinical and psychological implications. RSBO. 2013;10:11-20.
20. Molina OF, Rank RC, Simião BR, Torres SMP, Sobreiro MA, Cury SE et al. Occipital neuralgia as a true neuropathic pain: clinical and neurophysiological evidence. Rev Neurociênc. 2014;22:242-8.
21. Murayama RA, Stuginsku-Barbosa J, Moraes NP, Specia l i JG. Toothache referred f rom auriculotemporal neuralgia: case report. Int End J. 2009;42:845-51.
22. Nadkar MY, Desai SD, Itolikar M. Migraine: pitfalls in the diagnosis. JAPI. 2010;58:10-3.
23. Oshninsky ML. Sensitization and ongoing activation in the trigeminal nucleus caudalis. Pain. 2014;155:1181-2.
24. Penarrocha M, Bandres A, Bagan JV. Lowerhalf facial migraine: a report of 11 cases. J Oral Maxillofac Surg. 2004;62:1453-6.
25. Pihut M, Szuta M, Ferendiuk E, Zenczak- Wiekiewicz D. Differential diagnostic of pain in the course of t rigeminal neuralgia and temporomandibular joint dysfunction. BioMed Research International. 2014 Jun;1-7.
26. Piovesan E, Distani F, Kowacs PA, Mulmari RA, Radenz VH, Utiumi M et al. Massaging over the greater occipital nerve reduces the intensity of migraine attacks. Arq Neuropsychiat. 2007;65: 599-604.
27. Rampello L, Vecchio I, Migliore M, Malaguarnera M, Malaguarnera G, Rampello L. The most frequent medical neuralgias. Acta Med Medit. 2012;28:109-11.
28. Rajput G, Madhok S, Barghav A, Bhatt V. Facial pain: an enigma. Journal of Neck Physicians and Surgeons. 2014;2:1-13.
29. Sahai-Srivastava S, Zheng L. Occipital neuralgia with and without migraine: difference in pain characteristics and risk factors. Headache. 2011;51:124-8.
30. Solanki G, Solanki R. A review on facial neuralgias. Int J Biomed Adv Res. 2010;1(2):11-3.
31. Sulfaro MA, Gobetti JP. Occipital neuralgia manifesting as orofacial pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:751-5.
32. Trescot AM. Headache management in an interventional pain practice. Pain Physician. 2000;3:197-200.
33. Tsuboi K. Tension-type headaches. JMAJ. 2002;45:202-6.
34. Weiner RL, Reed KL. Peripheral stimulation for control of intractable occipital neuralgia. Neuromodul. 1999;2:217-21.
35. Yoon MS, Mueller DF, Hansen N, Poitz F, Slomka M, Dommes P et al. Prevalence of facial pain in migraine: a population-based study. Cephalalgia. 2009;30:92-6.
 Correspondence:
Correspondence:
Omar Franklin Molina
Avenida Pará, 1.544 – Faculdade de Odontologia
CEP 77400-000 – Gurupi – TO – Brasil
E-mail: omar-nyorker-harvardtexas@hotmail.com
Received for publication: August 29, 2014
Accepted: March 6, 2015













