Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.12 no.2 Joinville Abr./Jun. 2015
Original Research Article
Frequency of temporomandibular disorder diagnosis: a study on 102 patients undergoing dental treatment
Larissa de Oliveira ReisI; Josemar Parreira GuimarãesI; Isabel Cristina Gonçalves LeiteII; Isabela Maddalena DiasII
I School of Dentistry, Federal University of Juiz de Fora – Juiz de Fora – MG – Brazil
II School of Medicine, Federal University of Juiz de Fora – Juiz de Fora – MG – Brazil
ABSTRACT
Introduction: Epidemiological studies show that the prevalence of temporomandibular disorders (TMD) is high, ranging from 9.8 to 74%, it is important that the diagnosis be made as early as possible to avoid future clinical failure. Objective: To evaluate the prevalence of TMD in patients attended at the School of Dentistry of Federal University of Juiz de Fora (FO / UFJF), associated with age, gender and clinical group. Material and methods: 102 patients of both sexes were selected during treatment at FO / UFJF in Periodontics I and II, Partial Denture (RPD), Total Denture (TD), Secondary Care Clinic I and II disciplines, aged above 18 years-old. Patients were submitted to axis I of the RDC / TMD. Results: Of the total sample, 53.9% had a diagnosis of TMD. Of these, 67.3% were female and 52.7% were between 41-60 years. The most prevalent diagnosis of TMD was disc displacement with reduction corresponding to 18.6% of the population. RPD and TD clinics were, in this order, those who had more patients with diagnoses of TMD, respectively, 27.3% and 25.5% of the sample with TMD. Conclusion: A considerable proportion of patients had at least one sign or symptom of TMD. The evaluated sample shows how relevant is the evaluation of the masticatory apparatus as a whole, where teeth, muscles and temporomandibular joints, are viewed with the same level functional importance, regardless of which treatment the patient will receive.
Keywords: temporomandibular joint; diagnosis; temporomandibular joint disorders.
Introduction
The stomatognathic system is an extremely complex interrelated system, composed of muscles, bones, ligaments, teeth, nerves and the temporomandibular joints (TMJ) 1. TMJ is an element formed by various internal and external structures capable of performing complex movement s. The mast icat ion, swa l lowing and phonation rely heavily on function, health, and stability of this joint 24, and depend on the harmony of the muscles of the stomatognathic system 28. Currently, one of the major dentistry concerns is painful and / or functional disorders that affect the structures of this system such as pathological abnormal conditions caused by physical stress and primary changes of the masticatory muscles and temporomandibular joints 28.
The term temporomandibular disorder (TMD) is used to gather a group of diseases that affect the mast icatory muscles, TMJ and adjacent structures. The TMD can be classified into two large groups: those of articular origin, i.e. those in which the signs and symptoms are related to the ATM; and muscular origin, in which signs and symptoms relate to stomatognathic muscle 12. Several theories have been proposed to determine its etiology, but a single, specific factor was not detected 19. Thus, it is considered that the TMD have a multifactorial etiology and are related to structural, neuromuscular, occlusal (tooth loss, ill-fitting dentures, inadequate restorations, among others), and psychological factors (due to tension there is an increased muscular activity that generates spasm and fatigue); parafunctional habits (bruxism, onychophagia, supporting hand to the jaw, finger or pacifier sucking); and traumatic or degenerative injuries of TMJ 13, 20, 27.
In recent years it has been observed a considerable increase in the prevalence of signs and symptoms of TMD 19. The most frequently reported by patients with TMD are pain in TMJ and facial muscles, mouth opening limitation, joint sounds 3, 20, mandibular deviation 3, migraine, facial pain, muscle fatigue, otalgia, tinnitus 24, sense of decreased hearing acuity, dizziness and vertigo 12.
Epidemiological studies show that the prevalence of temporomandibular disorders is high and differs depending on the population studied and the diagnostic criteria used, ranging from 9.8 to 74% 13. With predominance in females, aged 21- 40 years 24, its signs and symptoms are milder at childhood and increases at adolescence 19, a period characterized by intense physical, hormonal, emotional, social and cognitive changes 13. In the adult population, it is reported the overall prevalence of signs and symptoms, achieving more than 75% of the population. In Brazil, one validated research including 1,230 inhabitants found at least one symptom of TMD was reported by 39.2% of the sample, two symptoms by 17.6% and three or more symptoms by 9.2% 9. And other TMD epidemiological studies show that 10-15% of the population will suffer someday from a painful experience involving TMJ, at some point during their lifetime, and about 8.5 million Brazilians will require some type of intervention in relation to TMD 24. In addition, studies related to the prevalence of TMD show that a large portion of the population shows signs and symptoms of dysfunction in subclinical and clinical levels. Thus, there is high prevalence of signs and symptoms of TMD in individuals considered as non-patients, i.e., those who do not seek treatment 23. Therefore, it is very important to report that the as early as TMD is diagnosed the better and more effective will be the treatment options, making the most favorable prognosis and causing minor losses in quality of life of the patient.
The study aimed to evaluate the prevalence of different TMD diagnoses in patients treated at the School of Dentistry (UFJF), to detect cases where there is need for treatment, but the patients were not adequately referred to a TMD specialized (TMJ Service FO/UFJF). Moreover, it is necessary to emphasize the importance of evaluation and multidisciplinary approach of the patient in dental care because many clinical failures can be avoided when different areas of dentistry are assessed in an integrated manner.
Methodology
This study was conducted in accordance with the rules and guidelines of Resolution n. 196/96 of the National Health Council, which regulates research involving human subjects and was approved by the Research Ethics Committee of the Federal University of Juiz de For a under protocol number #511.418.
To participate in this study, firstly the individuals signed a consent form by getting a copy of the study and being informed about the procedure and goals.
The previous sample calculation made by the software EPI INFO accounted for 5% of patients who were in attendance at every six months at the clinics of Periodontology I and II, removable partial dentures, removable Total Denture, Integrated Clinic Secondary Care I and II of the School of Dentistry, Federal University of Juiz de Fora, since, according to Moura 21, this would be the maximum percentage of TMD patients requiring some sort of treatment. Thus, 102 individuals were selected, and the inclusion criterion adopted was to have a minimum age of 18 years and be in treatment at the above clinics. Already exclusion criteria included patients who are already undergoing TMD treatment.
The sample was subjected to the application of Axis I, based on physical findings, of the RDC / TMD – Research Diagnost ic Criteria for Temporomandibular Disorders and Diagnostic Criteria for Temporomandibular Disorders Research. The RDC / TMD is considered a diagnost ic classification available in the literature most widely used and accepted and for which acceptable levels of reliability were reported. It groups a set of diagnostic criteria for research aimed at the standardization and replication of the research on the most common TMD etiologic forms (myogenic and arthrogenic) 9.
The diagnostic system is not hierarchical and allows multiple diagnoses for a single individual. As a rule to diagnose Axis I, an individual may be assigned at most one muscle diagnosis (group I) (myofascial pain or myofascial pain with limited opening, but not both) and at most one diagnosis from Group II and Group III for each side. Diagnostic within any group are mutually exclusive. This means that, in principle, an individual can receive a zero diagnosis (no diagnosable conditions) to five diagnoses (one muscular diagnosis another one from group II another one from group III for each side) 9.
So after applying the Axis I, the compilation of the results was made and the data were tabulated in Excel 2007 sheets. The descriptive analysis evaluated the frequency of TMD diagnoses present in the sample, as well as their frequency according to sex, clinical and age group.
Results
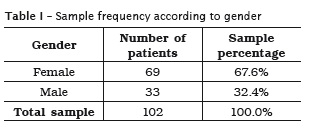
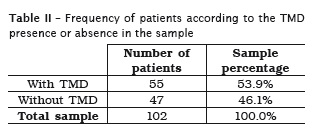
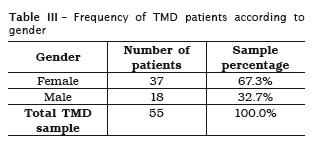
The sample consisted of 102 patients in care at FO / UFJF clinics, 69 women (67.6%) and 33 men (32.4%) (table I). Of these patients, according to the RDC / TMD diagnosis criteria, 55 patients (53, 9%) had at least one TMD diagnosis (table II), of which 37 (67.3%) were female and 18 (32.7%) were male (table III).
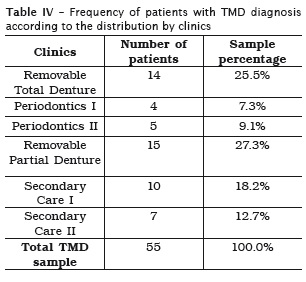
Of the 55 patients diagnosed with TMD, 14 were in attendance at Total Denture Clinics (TD) (25.5%), 4 at Periodontology I Clinics (7.3%), 5 at Periodontics II Clinics (9.1%), 15 at Removable Partial Denture Clinics (RPD) (27.3%), 10 at the Secondary Care Clinics I (CAS I) (18.2%), and 7 at the Secondary Care Clinics II (CAS II) (12.7%) (table IV).
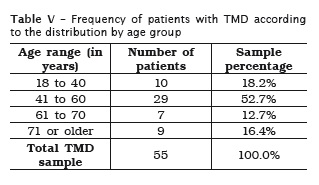
By associating the age of the sample group with TMD diagnosis, 10 patients were aged between 18 and 40 (18.2%), 29 patients between 41-60 years (52.7%), 7 patients between 61-70 years (12.7%) and 9 patients with 71 years or older (16.4%) (table V).
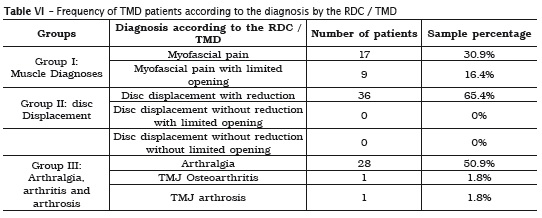
According to the diagnost ic criteria of the RDC / TMD used in this research, the disc displacement with reduct ion was the most common diagnosis, being found in 36 pat ients (65.4% of TMD pat ients) fol lowed by arthralgia, found in 28 patients (50.9% of TMD sample), myofascial pain, with 17 patients (30.9%), myofascial pain with limited opening with 9 patients (16.4%). The osteoarthritis was observed in one patient (1.8%) and osteoarthrosis also in only one pat ient (1.8%). The other diagnoses – disc displacement without reducing with limited opening and disc displacement without reducing without limited opening were undiagnosed (table VI).
Discussion
According to the RDC / TMD diagnost ic criteria, among the total sample, 55 patients (53.9%) had at least one TMD diagnosis. This result is consistent with those presented in the literature. Epidemiological studies show that the prevalence of temporomandibular disorders is high and differs depending on the population studied and the diagnostic criteria used, ranging from 9.8 to 74% 13. According to Oliveira et al. 22, studies on the TMD prevalence showed many people with signs and symptoms at clinical and subclinical levels. Thus, it has been found high TMD prevalence in non-patients, i.e. those who are not seeking health care. Prevalence studies on non-patients indicate that about 75% of people have at least one TMD signal, and 33% at least one symptom. Another estimative that evaluates the general population, according to Oliveira et al. 22 shows that 50 to 75% of people have one DTM signal, while 20 to 25% one symptom at any period of life.
According to Delboni and Abrão 10, due to the etiological complexity and variety of signs and symptoms that can generally also represent other conditions, the recognition and differentiation of TMJ disorders are not very clear to the professional. It is important to realize, in addition to routine dental examination, an anamnesis directed to specific TMD physical examination, so that, in combination with professional's knowledge, lead to TMD diagnosis 1.
In this study, of the 55 patients with TMD, 37 (67.3%) were female and 18 (32.7%) males, a ratio of two women for every man (2:1). Donnarumma et al. 12 claimed that women are more affected by TMD than men, a ratio 4:1. Patients evaluated in this study consists of a sample of the general population, since they were not specifically at a dental clinics for TMD and orofacial pain care, but at general care clinics, which may explain in part the proportion of involvement by gender found in this study.
With regard to age, in patients who had TMD, most of the sample had aged between 41 and 60 years (52.7%). It is noteworthy that even though the prevalent age group for TMD is 21-40 years old 24, the components of this study sample represent the general population in dental care, asymptomatic for the disorder, and not just in response to TMD and orofacial pain with symptoms. Furthermore, it is known that the age group most often affected by DTM in the literature refers to pain disorders, in which individuals have symptomatic 8. However, the present study aimed to cover all TMD diagnosis, not only the above.
By assessing patients diagnosed with TMD and the clinics the patient was being treated at, it was found that 14 (25.5%) were diagnosed at the Removable Total Denture Clinics (TD), 4 (7.3%) at the Periodontics Clinics I, 5 (9.1%) at the Periodontics Clinics II, 15 (27.3%) at the Removable Partial Denture Clinics (RPD), 10 (18.2%) at Secondary Care Clinics I (CAS I) e 7 (12.7%) at Secondary Care Clinics II (CAS II). It is clear, therefore, that the two clinics with the highest TMD patient frequencies are the RPD and TD, respectively, 27.3% and 25.5%. For Jorge et al. 18, there are controversies about the TMD in full or partial denture users. Some authors have reported that the use of prostheses do not affect the TMD appearance. Others believe that the loss of teeth, the loss of vertical dimension and occlusal instability can lead to the development of these disorders. The study of Serman et al. 26 conducted with 100 individuals with or without total dentures, were evaluated regarding to the presence or absence of TMD, occlusal condition, analysis of mandibular movement and the characteristics of the prosthesis, and 40% of the group with TD showed moderate and severe TMD symptoms, while only 12% of the dentate group had such a condition.
Furthermore, the other two clinics with higher prevalence of TMD were, respectively, the Secondary Care Clinic I (CAS I), with 18.2%, and the Secondary Care Clinic II (CAS II), 12.7%. Many professional immediately start treatment without gathering enough data to confirm or deny an attempt to TMD diagnosis. This fact may explain the occurrence of numerous cases which had established failure of therapy or waste of time, often precious, in treating the disease.
As for diagnoses of the RDC / TMD found in this research, the most prevalent one was the disc displacement with reduction (DDWR), corresponding to 65.4% of the sample, followed by arthralgia, with 50.9%, and the myofascial pain, with 30.9%. Corroborating this study, Buarque and Silva et al. 5 found that the most prevalent sign was the joint noise, observed in 71.5% of the sample. Silva 27 and Bagis et al. 3 stated that changes in condylar position can cause the disc displacement and generate a functional asynchrony between condyle and disc, causing muscle and / or joint noises and pain. In daily clinics, the dentist is often faced with this sign, but many professionals only guide their patients to seek treatment when they present painful symptoms. Studies show that individuals, who show signs and symptoms of TMD, although not in need of treatment, are at risk of becoming patients, which emphasizes the importance of Evaluating and diagnosing TMD.
Pain is an indisputable sign of the presence of any disease or injury; however our findings suggest that clinicians should also give special attention to the occurrence of TMJ noise. Pereira et al. 24 also states that TMJ crackles are also one of the other most frequent signals in patients with TMD, and for Bagis et al. 3 clicks can be a risk factor for the development of the disorder Hedge et al. 15 adds that sounds coming from the temporomandibular joint are usually indicators of a mechanical interference in this joint. The anterior disc displacement with reduction clinically verified through articular click, if not diagnosed and monitored, can develop into an anterior disc displacement without reduction, associated with pain and limited mouth opening, compromising the functional capacity of the patient 11.
In this study, the diagnosis of disc displacement without reduction (DDWR) without limited opening and DDWR with limited opening have not been verified, and only one case of osteoarthrosis and osteoarthritis were diagnosed. This finding can be explained by the fact that, besides being less prevalent than that of the other conditions, the DDWR generally are those with commonly false negative diagnoses by RDC / TMD, since this clinical sign many times has to be confirmed by imaging tests such as magnetic resonance imaging (MRI) 14. According to Isberg 17, a false negative in clinical diagnosis of disc displacement without reduction can be seen in two-thirds of the joints due to absence of noise joint. Concerning to osteoarthrosis, according to Honda et al. 16, the crackling sounds are a clinical sign of changes in joint structure, corresponding to the contact between two hard tissue surfaces, but the authors pointed out that joints with advanced cases of degeneration cannot present any noise when evaluating clinically the condylar movement, which emphasizes the importance of imaging for higher diagnostic accuracy 25.
Carrara et al. 7 emphasized that it is evident the need to devote more attention to TMD, for obvious reasons: high prevalence of signs and symptoms in the population, patient's suffering due to pain and limitations that compromise their quality of life, high social and personal cost. The pain from TMD can also cripple a patient, not only the lack of tooth. It can affect your chewing ability, disable it to talk and even swallow, and through frustrations and sufferings can lead to depression, compromising the quality of life of patients 1.
Conclusion
Considering the discussion above, the considerable frequency of TMD in the sample studied (53.9%) shows how much is relevant the assessment of the masticatory system globally, in which teeth, muscles and temporomandibular joints be viewed with the same level of functional importance, irrespective of which treatment the patient will receive.
References
1. Alencar FPG. Oclusão, dores orofaciais e cefaléias. 1ª ed. São Paulo: Santos; 2005. p. 97-110. [ Links ]
2. Ash MM. Current concepts in etiology, diagnosis and treatment of TMJ and muscle dysfunction. J Oral Rehabil. 1986 Jan;1(13):1-20.
3. Bagis B, Ayaz EA, Turgut S, Durkan R, Özcan M. Gender difference in prevalence of signs and symptoms of temporomandibular joint disorders: a retrospective study on 243 consecutive patients. International Journal of Medical Sciences. 2012;9(7):539-44.
4. Branco RS, Branco CS, Tesch R de S, Rapoport A. Frequência de relatos de parafunções nos subgrupos diagnósticos de DTM de acordo com os critérios diagnósticos para pesquisa em disfunções temporomandibulares (RDC/TMD). Rev Dental Press Ortodon Ortop Facial. 2008 Mar-Apr;2(13):61-9.
5. Buarque e Silva WA, Andrade e Si lva F, Ribeiro CE, Buarque e Silva LL, Oliveira M de. Prevalência de sinais e sintomas de disfunções temporomandibulares (DTM) em adultos tratados no Cetase: um estudo piloto transversal. Revista Portuguesa de Estomatologia Médica e Dento- Cirúrgica-Maxilofacial. 2011;52(4):2000-4.
6. Campos JADB, Carrascosa AC, Loffredo LCM, Faria JB. Consistência interna e reprodutibilidade da versão em português do critério de diagnóstico na pesquisa para desordens temporomandibulares (RDC/TMD – Eixo II). Rev Bras Fisioter. 2007 Nov- Dec;6(11):451-9.
7. Carrara SV, Conti PCR, Juliana SB. Termo do 1.º Consenso em Disfunção Temporomandibular e Dor Orofacial. Dental Press J Orthod. 2010;15(3):114-20.
8. Carlsson GE. Epidemiology and treatment need for temporomandibular disorders. Journal Orofacial Pain. 1999;4(13):232-7.
9. Costa AL, Campos LS, França Jr MC, D'Abreu A. Temporomandibular disorders in patients with craniocervical dystonia. Arq Neuropsiquiatr. 2011;6(69):896-9.
10. Delboni MEG, Abrão J. Estudo dos sinais de DTM em pacientes ortodônticos assintomáticos. Rev Dental Press Ortodon Ortop Facial. 2005 Jul- Aug;4(10):88-96.
11. Dias IM, Coelho PR, Picorelli Assis NM, Pereira Leite FP, Devito KL. Evaluation of the correlation between disc displacements and degenerative bone changes of the temporomandibular joint by means of magnetic resonance images. Int J Oral Maxillofac Surg. 2012 Sep;41(9):1051-7.
12. Donnarumma MDC, Muzilli CA, Ferreira C, Nemr K. Disfunções temporomandibulares: sinais, sintomas e abordagem multidisciplinar. Rev CEFAC. 2010 Sep-Oct;12(5):788-94.
13. Drabovicz PVSM, Salles V, Drabovicz PEM, Fontes MJF. Assessment of sleep quality in adolescents with temporomandibular disorders. J Pediatr. 2012;2(88):169-72.
14. Dworkin SF, Leresche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301-55.
15. Hegde SV, Raghavendra M, Ganapathy KS, Sujatha D, Bharati AP. Prevalence of signs and symptoms of temporomandibular disorders in dental students. Journal of Indian Academy of Oral Medicine and Radiology. 2011;23(3):316-9.
16. Honda K, Natsumi Y, Urade M. Correlation between MRI evidence of degenerative condylar surface changes, induction of articular disc displacement and pathological joint sounds in the temporomandibular joint. Gerodontology. 2008;4(25):251-7.
17. Isberg A. Disfunção da articulação temporomandibular: um guia para o clínico. São Paulo: Artes Médicas; 2005. p. 65-102.
18. Jorge JH, Silva Junior GS da, Urban VM, Neppelenbroek KH, Bombarda NHC. Desordens temporomandibulares em usuários de prótese parcial removível: prevalência de acordo com a classificação de Kennedy. Rev Odontol Unesp. 2013 Mar-Apr;42(2):72-7.
19. Machado E, Machado P, Cunali PA, Grehs RA. Ortodontia como fator de risco para disfunções temporomandibulares: uma revisão sistemática. Rev Dental Press J Orthod. 2010 Nov-Dec;15(6):1-10.
20. Mi lanesi JM. Severidade da desordem temporomandibular e sua relação com medidas cefalométricas craniocervicais. Fisioter Mov. 2013;26(1):79-86.
21. Moura RSN. Sinais e sintomas da disfunção temporomandibular: revisão de literatura. Rev Odontol Univ Cid São Paulo. 2013;25(2):135-40.
22. Oliveira AS, Dias EM, Contato RG, Berzin F. Prevalence study of signs and symptoms of temporomandibular disorder in Brazilian college students. Braz Oral Res. 2006;20(1):3-7
23. Oliveira AS, Bevilaqua-Grossi D, Dias EM. Sinais e sintomas da disfunção temporomandibular nas diferentes regiões brasileiras. Fisioterapia e Pesquisa. 2008 Oct-Dec;4(5):392-7.
24. Pereira KNF, Andrade LLS de, Costa MLG da, Portal TF. Sinais e sintomas de pacientes com disfunção temporomandibular. Rev CEFAC. 2005 Apr-Jun;2(7):221-8.
25. Ramos ACA, Sarmento VA, Campos PSF, Gonzalez MOD. Articulação temporomandibular – aspectos normais e deslocamentos de disco: imagens por ressonância magnética. Radio Bras. 2004;(37):449-54.
26. Serman RJ, Conti PCR, Conti JV, Salvador MCG. Prevalência de disfunção temporomandibular em pacientes portadores de prótese total dupla. JBA. 2003 Apr-Jun;10(3):141-4.
27. Silva FA. Pontes parciais fixas e o sistema estomatognát ico. São Paulo: Santos; 1993. p. 177-8.
28. Silva AMT, Morisso MF, Cielo CA. Relação entre o grau de severidade de disfunção temporomandibular e a voz. Pró-Fono Revista de Atualização Científica. 2007 Jul-Sep;3(19):279-88.
 Correspondence:
Correspondence:
Larissa de Oliveira Reis
Sítio Córrego Santana, s/n – Zona Rural
CEP 36525-000 – Guiricema – MG – Brasil
E-mail: larissadeoreis@gmail.com
Received for publication: September 11, 2014.
Accepted: February 19, 2015.













