Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.12 no.2 Joinville Abr./Jun. 2015
Literature Review Article
Influence of bisphosphonates on Implantology – literature review
Bárbara Botolli do NascimentoI; Claudia Aline PimentaII; Celso YamashitaII; João Cesar ZielakII; Tatiana Miranda DeliberadorII; Rafaela ScariotII
I Specialization in Implantology, Positivo University – Curitiba – PR – Brazil
II Graduate and Post-Graduate, Positivo University – Curitiba – PR – Brazil
ABSTRACT
Introduction: Oral rehabilitation with dental implants becomes limited in patients who make use of sodium bisphosphonate (BF), because this drug inhibits osteoclast activity and thus osteoblastic, fundamental steps to implant osseointegration. Furthermore, this drug can cause osteonecrosis of the jaw (OJ). The dentist has to fully know about this drug and its side effects, to differentiate it from other changes. Objective: This study aimed to review the literature on the influence of bisphosphonates on implant and to evaluate the possible complications resulting from prolonged use, providing subsidies to the dentist to prevent and recognize the patient with osteonecrosis of the jaws Literature review: The BPs are a class of drugs used for the treatment of bone diseases such as osteoporosis, because their mechanism of action inhibits the function of osteoclast. However, these drugs may cause some side effects known as the OJ. Patients undergoing intravenous therapy are more likely to develop these changes than those undergoing oral therapy. OJ is characterized by painful symptoms, leaving the exposed bone in the oral cavity. There are several treatment strategies according to the clinical stage that the patient presents. Conclusion: The installation of dental implants in patients who make use of BPs presents risks, since this drug can cause OJ.
Keywords: osteonecrosis; bisphosphonates; dental implant.
Introduction
With increasing life expectancy of Brazilians, the number of elderly also increases. This brought many challenges for many areas, especially for professional health. These patients are increasingly looking for dentists for oral rehabilitation with dental implants 23. It is extremely important that the dentist is aware of possible drug that the elderly can take. One of the most widely used drugs is sodium alendronate, a drug belonging to the class of bisphosphonates (BPs), widely used in the treatment of osteoporosis 3, 4, 9, 10, 14, 17, 20-22, 26, 30, 33.
The BPs are also employed in the control of Paget's disease, myeloma, bone metastases, breast and prostate cancer, malignant hypercalcemia of malignancy, osteogenesis imperfecta in children, idiopathic juvenile osteoporosis and reduction of bone loss associated with periodontal disease 2, 4-6, 8, 13-18, 21, 24, 27, 28, 31-33.
The long-term use of this drug can cause undesirable effects such as osteonecrosis of the mandible and maxilla. So it is of utmost importance to conduct a thorough medical history to prevent the s development risks of this condition, which can cause serious health problems 6, 11. The execution of invasive surgeries, such as installing implants in patients taking BPs, can be a highrisk procedure. The dentist should know when to indicate or contraindicate the implant placement, and it is important to understand the mechanisms of action of these drugs, having knowledge of their adverse effects and paying attention to prevention and treatment strategies 2, 8, 15, 19, 24, 29.
This study aimed to review the literature on the influence of bisphosphonates in implant and to evaluate the possible complications arising from prolonged use, providing subsidies to prevent dental surgeon and recognize the patient with osteonecrosis of the jaw caused by BPs.
Literature review
Bisphosphonates
In the decade of 1960s, the calcium pyrophosphate was discovered as physiological regulator of calcification and bone resorption; however it was inactivated by enzymes of the gastrointestinal mucosa, which prevents its oral use 22.
At the end of the 1960s, BPs were developed, which are chemical analogous of pyrophosphate 2-4, 8, 18, 27, 29, 31, with great bone-bonding ability, inhibiting the action of osteoclasts 8, 22, 29, 33. These substances are chosen for the treatment of skeletal diseases and can be used orally 6, 29. The BPs s decrease osteoclast activity, increase bone mineral density and consequently lower the risk of fractures in 4, 15, 16, 18, 29.
This group of drugs is poorly absorbed in the gastrointestinal tract (about 1 to 2%). Once free in plasma, is excreted by the kidney 6, 15. Besides the oral route of administration, the intravenous route is very employed in cancer patients 8, 13, 16, 21, 24.
This drug can stay for a long period within the bone matrix, according to the type of treatment and duration. Once within the bone, the osteoblast failure in resorption the bone causes the die of osteoblasts and osteocytes, leaving an acellular matrix in the bone. The result is the degeneration of the capillary vascularization and increased bone fragility 29.
Pharmacology, mechanism of action of BPs
BPs can be divided into nitrogenous and nonnitrogenous and are classified into three generations, according to their power. The third generation BPs are considered more potent than the second, and these more potent than the first 22.
Among the non-nitrogenous BFs are clodronate, etidronate and tiludronate. The nitrogen-containing BFs are alendronate, ibandronate, olpadronate, risedronate, zoledronate, pamidronate. These nitrogenous compounds present a greater affinity for calcium molecules present in bone tissue, so they are more potent 22, 29.
The BPs mechanism of action are similar in all the groups, and responsible for inhibiting the activity of osteoclasts, resulting in an imbalance in the bone remodeling process, and hence also affects the osteoblastic activity 4, 22, 31.
From a pharmacological point of view, this drug presents a short half-life, remaining in the plasma for a few hours, but it can accumulate over the years inside the bone matrix 13, 22, 29.
Clinical applications and adverse effects
The BPs are widely used in the treatment of skeletal diseases i.e.: osteoporosis, Paget's disease, osteogenesis imperfecta, idiopathic juvenile osteoporosis; and neoplasms i.e.: myeloma, bone metastases of breast and prostate cancer and hypercalcemia of malignancy 2, 4-6, 8, 13-18, 21, 22, 29, 33. The route of administration depends on the type of disease to be dealing with. The oral BPs are used in the treatment and osteoporosis, Paget's disease, osteogenesis imperfecta. In contrast, the injectable BPs are commonly used in cancer patients to aid in the control of skeletal bone loss resulting from metastatic lesions, together with anti-neoplastic drugs 8, 18, 29.
These drugs can present some adverse effects, e.g.: gastrointest inal disorders (esophagit is, vomiting, diarrhea, abdominal pain, esophageal ulcers), kidney problems leading to increased levels of creatinine, dyspnea, swelling, asthenia, anemia, necrosis, bone, muscle and joint aches and flu-like symptoms 13, 15, 18, 22.
Recently, an undesirable effect associated with bisphosphonate therapy was found, of utmost concern to the dental class, called osteonecrosis of the jaws (OJ) 8, 13.
Marx, in 2003, reported the first cases of osteonecrosis associated with bisphosphonates (OJ) through intravenous route 8, 18. These injectable BFs are at higher risk of developing osteonecrosis of the jaws, due to greater potency compared to oral BPs 22. Population studies show an OJ incidence of 0.01% to 0.04% by oral BPs and 0.08% to 1.5% by injectable BPs. Therefore, patients taking BPs, either orally or intravenously, are a group of risk in cases of performing oral surgery 8.
The osteonecrosis associated with BPs
Osteonecrosis is a clinical condition in which the maxillary or mandibular bone exposed in the oral cavity for at least 8 weeks in the absence of prior radiotherapy treatment rand metastasis in the jaws. It has mostly been reported in patients receiving high doses of intravenous BPs. The risk of developing OJ is mainly associated with prolonged therapy, especially in treatments for three years or more 8.
The preference for the bones of the maxilla ad mandible is because BPs accumulate exclusively in skeletal sites with high bone remodeling. The second theory is that oral mucosa is thin and can be easily traumatized during surgery, allowing contact with the infected saliva and developing osteonecrosis 16, 29.
According to Cast i lho et al. (2013), the literature reports that there is a possibility that this injury be related with the use of corticosteroids employed concurrently with BPs and with the hormonal replacement with estrogen. Obese, immunosuppressed patients; those undergoing hemodialysis; smokers; alcoholics, diabetics are more likely to develop osteonecrosis of the jaws 2, 3, 6, 8, 13, 16.
In 2007, the American Association of Oral and Maxillofacial Surgeons (AAOMS) defined OJ as the simultaneous existence of three criteria: a) current or previous treatment with BFs; b) bone necrosis in the maxillofacial area which persists for more than 8 weeks c) absence of local radiotherapy history 1, 2, 6, 8, 11, 13, 16, 18, 21, 26, 27, 29. For an accurate diagnosis, it is the necessary to distinguish it from other probable most common injuries, for example, sinusitis, gingivitis, periodontitis, caries, alveolar osteitis, periapical disease, changes in the temporomandibular joint, primary mandibular tumor, tumor metastasis, and osteomyelitis of the j 18.
The AA MS established some risk factors for the development of OJ and ranked in local, demographic/systemic and drug-related.
– Risk factors related to the drug:
• duration of therapy: the higher the duration the higher will be the therapeutic risk;
• power BFs: zoledronate> pamidronate> oral BFs.
– local risk factors:
• dentoalveolar surgery (dental extractions, dental implants, periapical al surgery) increases up to 7 times the risk of OJ;
• local anatomy: the lesions are more common in the jaw and thinner mucosal regions on bony prominences;
• concurrent oral disease: pat ients wit h inflammatory oral diseases are 7 times more likely to develop osteonecrosis of the jaws, when treated concomitantly with BFs.
– Systemic and demographic risk factors:
• Caucasians have a higher propensity than blacks;
• type of malignancy: high-risk individuals with multiple myeloma, followed by breast tumor
– Probable risk factors:
• patients taking corticosteroids, smokers, diabetics and those with poor oral hygiene have increased chance of osteonecrosis development 1, 11, 18, 26.
This injury may remain asymptomatic for weeks and even months, but the most common signs and symptoms are pain, swelling, erythema, exudation of the mucosa, soft tissue ulceration, suppuration, presence of fistula and tooth mobility. The clinical presentation is often varied, and sensitivity in the area affected by bone necrosis and episodes of chronic sinusitis secondary to osteonecrosis with or without oroantral fistula can occur when the jaw is affected 8. In more advanced stage, the patient may complain of severe pain and paresthesia 13.
Complementary imaging tests as panoramic and periapical radiographs are useful to detect osteonecrosis, but not in its early stages. Computerized tomography is also not useful for detection of disease in asymptomatic patients 2, 6.
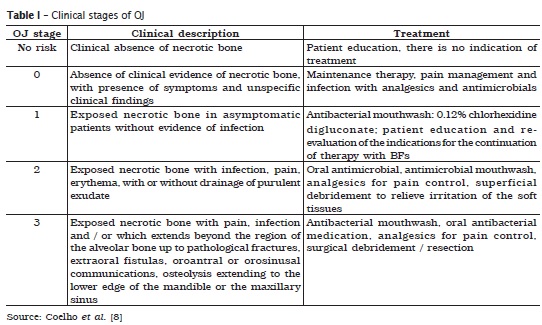
According to Coelho et al. (2010), the literature described five stages of osteonecrosis with different clinical presentations and treatments, which can be seen in the following table:
A treatment alternative would be hyperbaric ox yg en, widely us ed in t he t reatment of osteoradionecrosis of the jaw. Hyperbaric oxygen increases the amount of oxygen in the blood, allowing greater oxygenation in peripheral tissues. The benefits of this type of treatment are better healing of the surgical wound, reduction of the edema and inflammation and moderating effect of suppression of bone turnover caused by BFs. However its effectiveness as the treatment of choice for OJ has not been proven 6, 8.
Bisphosphonates X implant
As BPs act directly on the bone replacement process, there is a probability and of these patients have problems in osseointegration. BPs end up interacting with the bone and vascular turnover , which interferes in the quality and quantity of bone tissue, so important to the Implantology, and thus cause an accumulation of microdamages and changes the properties of the tissue, affecting hemostasis of newly formed tissue around the implants 33.
Intra- and extraoral exams, imaging and laboratory examinations as complete blood count and coagulation tests, fasting blood glucose, urea, creatinine should be requested to assess the health condition of the patient, together with a specific examination to evaluate bone reabsorption, called C-terminal telopeptide (CTX). The CTX allows assessing the risk of osteonecrosis in patients who are being treated with BF for more than three years. Serum levels of this test allows assessing the risk of the patient develops OJ:
• values less than 100 pg / ml - high risk;
• values between 100 and 150 pg / ml - moderate risk;
• values between 150 and 299 pg / ml - low risk;
• greater than 300 pg / ml - no risk.
Low CTX values demonstrate the need of the drug discontinuation for at least 6 months to normalize the serum levels 16, 22. If stopping the medicine is not possible, the patient should instructed about the risk of OJ 4. These patients who make use of BFs for more than three years, or associate with corticosteroids, it is recommended stopping treatment six months before and after the installation of implants, returning its use after complete healing of the tissues involved. In this case, the therapeutic modification or cessation of treatment should be made together with the doctor accompanying the patient 6, 8, 16.
An informed consent form should be signed by the patient, in order to inform the risks 13.
Discussion
BPs are widely used in the treatment of skeletal disorders, and with increasing of life expectancy the use of this drug has become increasingly common, bringing a major challenge for dentistry, especially for implant 6.
It is important that the dentist conducts an excellent anamnesis with a well-formulated questionnaire on BFs, irrespective of age, in order to avoid omission of information, for forgetfulness of patients. Also, it must be investigated the dose, frequency and duration of the treatment, since these factors contribute to the risk of OJ 22.
To have knowledge about the mechanism of act ion of BPs and their possible adverse effects is paramount in order to treat them when necessary. Also because the region of the jaws is the most commonly affected, because of their greater exposure to infection and trauma 15, 22. Several studies 2, 22, 29 reported higher incidence of OJ in patients who use intravenous BFs compared to oral administration, due to its greatest power. This complication is observed in these patients at long-term use for more than three years 13.
The OJ can be asymptomatic for months or even years and cannot be seen radiographically in its initial phase 2, 6. In more advanced stage, the patient may experience severe pain, swelling, erythema, exudation of the mucosa, soft tissue ulceration, suppuration, presence of fistula and tooth mobility 8.
The dentist must distinguish OJ from other changes. Whenever one needs to assess: if the patient makes current use or made past use of BFs, history of radiotherapy and exposed bone in the oral cavity for more than 8 weeks. For each OJ stage, a treatment should be assigned. Recently, a new therapy type has been reported, with hyperbaric oxygen, but its effectiveness as a treatment of choice has not been proven 8.
Individuals who have proven low risk of OJ should be guided by the dentist to perform routine appointments for oral health maintenance. Patients who have motor difficulties should be instructed to make the oral hygiene with the aid of an electric toothbrush and to reduce food intake with sucrose 6. On the other hand, high-risk patients who normally take intravenous BPs need to avoid any kind of invasive procedure involving bone remodeling, as dentoalveolar surgery, periapical surgery and implant placement. Conservative procedures may be performed on patients taking BPs; however, the surgical procedures must be avoided 6, 8, 13.
It is important to be a relationship between the dentist and the physician accompanying the patient management, in order to prevent problems and treat these patients, whenever necessary. The drug suspension or continuation should only be done by the patient's physician. There is greater chances of success in promoting oral health of patients who make use of BFs with a fully integrated team 8.
Conclusion
BPs have great influence in dentistry, especially in the Implantology. It is necessary that the dentist has knowledge about the drug and its great potential to cause harm to the region of the jaws. It is essential to perform a good anamnesis in order to collect important information to establish an adequate treatment plan, concurrently with the medical staff. Patients should be oriented about the risk / benefit and this drug.
References
1. Advisory Task Force on Bisphosphonate-Related Osteonecrosis of the Jaws. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg. 2007 Mar;65(3):369-76. [ Links ]
2. Bezeruska C, Moraes RS, Muller PR, Kluppel LE, Rebellato NLB, Costa DJ. Osteonecroses maxilo-mandibulares relacionadas à utilização de bisfosfonatos. Rev Cir Traumatol Buco-Maxilo-Fac. 2012 Jan/Mar;1(12):107-12.
3. Bispo LB. Implantology considerations about osteonecrosis of the jaw powerful by bisphosphonate therapy. Rev Bras Odontol. 2013 Jul-Dec;2(70): 196-201.
4. Brozoski MA, Traina AA, Deboni MCZ, Marques MM, Homem-Naclério MG. Osteonecrose maxilar associada ao uso de bisfosfonatos. Rev Brasil Reumatol. 2012;52(2):260-70.
5. Canhão H, Fonseca JE, Queiroz MV. Diagnosis and treatment of osteoporosis in childhood. Acta Med Port. 2004;17:385-90.
6. Castilho LS, Lisboa SSML, Costa LN, Vilaça EL, Silva MES, Silveira RR. Considerations about the patient being with bisphosphonates: what every dentist needs to know. Rev CROMG. 2013 Jan- Jun;1(14):19-24.
7. Chaudhry AH, Ruggiero SL. Osteonecrosis and bisphosphonates in oral and maxillofacial surgery. Oral Maxillofac Surg Clin North Am. 2007 May;19(2):199-206.
8. Coelho AI, Gomes PS, Fernandes MH. Osteonecrose dos maxilares associada ao uso de bifosfonatos. Parte II: linhas de orientação na consulta de medicina dentária. Rev Port Estomatol Med Dent Cir Maxilofac. 2010;51:185-91.
9. Consolaro A, Consolaro MFMO. Bifosfonatos e tratamento ortodôntico. Rev Clin Ortodont Dental Press. 2008 Jun-Jul;3(7):104-9.
10. Conte-Neto N, Bastos AS, Spolidorio LC, Ma rcantonio RA, Ma rcantonio Jr E. Ora l bisphosphonate-related osteonecrosis of the jaws in rheumatoid arthritis patients: a critical discussion and two case reports. Head Face Med. 2011 Apr;27(7):7.
11. Coskun BI, Guzel R. Oral bisphosphonates related osteonecrosis of the jaw: a challengin adverse effect. ISRN Rheumatol. 2013 May;2013:[6 páginas]. DOI 215034.
12. Donagelo I, Coelho SM, Farias MLF. Osteogenesis imperfecta no adulto e resposta ao alendronato. Arq Bras Endocrinol Metab. 2001 Jun;3(45):309-13.
13. Ferreira Junior CD, Casado PL, Barboza ESP. Osteonecrosis associated with bisphosphonates in dentistry. Rev Periodont. 2007 Dec;4(17):24-30.
14. Freiberger JJ, Padilha-Burgos R, Chhoeu AH, Kraft KH, Boneta O, Moon RE et al. Hyperbaric oxygen treatment and bisphosphonates-induced osteonecrosis of the jaw: a case series. J Oral Maxillofac Surg. 2007 Jul;65(7):1321-7.
15. Gegler A, Cherubin K, Figueiredo MAZ, Yurgel LS, Azambuja AA. Bisphosphonates and maxillary osteonecrosis: literature review and two case reports. Rev Bras Cancerol. 2006 Jan- Mar;52(1):25-31.
16. Guimarães J. Colocação de implantes dentários em doentes que fazem tratamento com bifosfonatos. Rev Maxillaris. 2012 Jul-Aug;41:28-34.
17. Goes P, Lima V. Efeito dos bisfosfonatos na doença periodontal: revisão narrativa da literatura. Rev Odontol UNESP. 2011 Sep-Oct;40(5):255-63.
18. Lopes I, Zenha H, Costa H, Barroso J. Osteonecrose da mandíbula associada ao uso de bifosfonatos. ArquiMed. 2009;23(5):181-5.
19. Mariotti A. Bisphosphonates and osteonecrosis of the jaws. J Dent Educ. 2008 Aug;72(8):919-29.
20. McMahon RE, Bouquot JE, Glueck CJ, Griep JA, Adams WR, Spolnik KJ et al. Staging bisphosphonate-related osteonecrosis of the jaw should include early stages of disease. J Oral Maxillofac Surg. 2007 Sep;65(9):1899-900.
21. Milani CM, Lobo M, Carrilho E, Souza JA, Machado MAN. Biphosphonate related osteonecrosis of the jaw: case report. Rev Odonto. 2012 Jan- Jun;20(39):27-33.
22. Moraes SLC, Afonso AMP, Santos RG, Mattos RP, Oliveira MTF, Zanneta- Barbosa D et al. Risks and complications to the facial bones after bisphosphonates use. Rev Bras Odontol. 2013 Jul- Dec;70(2):114-9.
23. Neto AMP, Soares A, Urbanetz AA, Souza ACA, Ferrari AEM, Amaral B et al. Rev Bras Reumatol. 2002 Nov-Dec;42(6):343-54.
24. Poubel VLN, Cruz DSM, Gil LF, Lima Júnior N, Claus JDP, Gil JN. Maxillomandibular osteonecrosis induced by bisphosphonate: a literature review. Rev Cir Traumatol Buco-Maxilo-Fac. 2012 Jan-Mar;1(12):33-42.
25. Rincón IH, Rodriguez IZ, Tambay MC, Moreno JJM. Osteonecrosis of the jaws and bisphosphonates. Report of fifteen cases. Therapeutic recommendations. Med Oral Patol Oral Cir Bucal. 2007 Aug 1;12(4):267-71.
26. Ruggiero SL, Dodson TB, Assael LA, Landesberg R, Marx RE, Mehrotra B. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaw – 2009 update. Aust Endod J. 2009 Dec;35(3):119-30.
27. Sampaio FC, Veloso HHP, Barbosa DN. Bisphosphonates mechanisms of action and it influence in the endodontic treatment prognosis. Rev Fac Odontol. 2010 Jan-Apr;1(51):31-8.
28. Sa ntos PSS, Ol i vei ra MA, Fel i z VB. Bisphosphonate-induced maxillofacial osteonecrosis in osteoporotic individuals. Rev Bras Ortop. 2011 Sep-Oct;46(5):495-9.
29. Scarpa LC, Leite LCM, Lacerda JCT, Arantes DCB. Osteonecrosis of the jaws associated with the use sodium bisphosphonates. Rev Bras Pesq Saúde. 2010;12(1):86-92.
30. Silvestre-Donat FJ, Puente SA. Efectos adversos del tratamiento del cáncer oral. Av Odontoestomatol. 2008;24(1):111-21.
31. Vasconcellos DV, Duarte ME, Maia RC. Antitumor effect of bisphosphonates: a new therapeutic perspect ive. Rev Bras Cancerol. 2004 Jan- Mar;50(1):45-54.
32. Wang EP, Kaban LB, Strewler GJ, Raje N, Troulis MJ. Incidence of osteonecrosis of the jaw in pat ients with mult iple myeloma and breast or prostate cancer on intravenous bisphosphonate therapy. J Oral Maxillofac Surg. 2007 Jul;65(7):1328-31.
33. Yama s saka J, Ol ivei ra PAD, Ol ivei ra AMS, Dutra BC, Abreu FAM. Bisphosphonate alendronate in the periodontal therapy. Rev Period. 2013;23(4):50-5.
34. Zahrowski J. Comment on the American Association of Oral Maxillofacial Surgeons statement on bisphosphonates. J Oral Maxillofac Surg. 2007 Jul;65(7):1440-1.
 Correspondence:
Correspondence:
Bárbara Bortolli do Nascimento
Rua Professora Maria de Assumpção, n. 2.401 – Hauer
CEP 81670-040 – Curitiba – PR – Brasil
E-mail: babi_f1@hotmail.com
Received for publication: April 12, 2015
Accepted: May 5, 2015













