Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.12 no.2 Joinville Abr./Jun. 2015
Case Report Article
Root coverage of adjacent gingival recessions with a combination of two surgical techniques
Thiago Marchi MartinsI; Paula Lazilha FaleirosII; Natália Marcumini PolaI; Leandro Araújo FernandesIII; Alvaro Francisco BoscoII
I Department of Semiology and Clinics, School of Dentistry, Federal University of Pelotas – Pelotas – RS – Brazil
II Department of Surgery and Integrated Clinics, School of Dentistry of Araçatuba, São Paulo State University – Araçatuba – SP – Brazil
III Department of Clinics and Surgery, School of Dentistry, Federal University of Alfenas – Alfenas – MG – Brazil
ABSTRACT
Introduction: The dentin hypersensitivity associated with gingival recession is an occurrence of high prevalence in the clinical routine of dentists. Coverage of exposed root surfaces represents a challenge for periodontal treatment. Objective: The purpose of the present study is to describe an approach for adjacent gingival recession treatment using a combination of two surgical techniques: the subepithelial connective tissue graft (SCTG) with a laterally positioned double flap. Case report: This surgical treatment was conducted in a 45-yearold female patient who complained of sensitivity when brushing the lower right teeth. Clinical and radiographic examinations showed gingival recessions (Miller Class III) with traumatic origin promoted for tooth brushing and the presence of thin periodontium in the region. In addition, interproximal bone loss was noted on vestibular face of the right mandibular second premolar and mesial root of the right mandibular first molar. At 12 postoperative months, it was observed that the association of the two surgical techniques promoted an almost complete coverage of the gingival recessions, an increased keratinized gingival band and the elimination of initial dentin hypersensitivity. Conclusion: The appropriate choice of techniques and patient compliance to the periodontal support therapy led to treatment success and periodontal health maintenance in the region during the whole follow-up period.
Keywords: gingival recession; Periodontium; surgical flaps.
Introduction
Gingival recession is the apical displacement of marginal tissue with respect to the cement-enamel junction with root surface exposure 1, 14. Gingival recession is a common characteristic in populations with high standards of oral hygiene as well as in populations with poor oral hygiene. Several factors can be responsible for the presence of this condition, such as traumatic brushing or other gingival tissue traumas, lack of attached gingiva, gingival inflammation, local iatrogenic factors, anomalous attachments of labial frenulum and bridles, altered tooth positioning, shallow vestibule, thin cortical bone, or the presence of bone fenestrations and dehiscence. Since in most cases the etiology of recessions is associated with accumulation of biofilm on the tooth surface, biofilm removal is necessary before surgical intervention 5.
The clinical recession condition is easily noticed by patients. The main complaint is tooth hypersensitivity, generally associated with thermal and tactile stimuli, with episodes of sharp and short duration pain 14. Another reason for frequent complaint by patients is the unfavorable esthetic aspect of root exposure 21. In addition, there is also the risk of caries since root surfaces become exposed to the oral environment 14.
The coverage of exposed roots represents one of the great challenges of periodontal treatment. The most widely used techniques to correct recessions are the coronally repositioned flap 18, the semilunar bone coronally repositioned flap 24, pedicle grafts 11 and the laterally positioned flap (LPF) 9. Among these techniques, the LPF continues to be an efficient option for periodontal treatment, despite being one of the earliest mucous gingival surgery techniques 15. LPF is a pedicle graft, derived from plastic surgery techniques and similar to the rotation flap for skin surgery 20. This technique has undergone some modifications since the first reports, and is currently combined with other techniques, such as subepithelial connective tissue graft (SCTG) 15, 20.
LPF is mainly recommended to cover gingival recessions of one or two teeth, promoting better esthetics and augmenting attached gingiva in order to restore the mucogingival region. This results in reduced hypersensitivity and prevents cervical caries and other non-carious cervical injuries. Conversely, this technique must not be used in the presence of interproximal periodontal pockets, shallow vestibules, multiple recessions, and in areas exhibiting insufficient adjacent soft tissue, excessive root prominence, or deep cervical abrasions 9.
The LPF was first described by Grupe and Warren 9 as a surgical procedure that encompasses the use of a full-thickness flap that is horizontally displaced to cover the exposed root. However, this technique has undergone some modifications since the first reports, and is currently combined with other techniques. One of modifications was proposed by Bosco et al. 4 in which an internal bevel is performed in the recipient area and an external bevel is performed in the flap to be laterally positioned. This technique promotes better flap adaptation to the recipient area and favors the esthetic result by reducing incision line perception after scarring. In addition, other authors have been proposed the association of a connective tissue graft coverage by LPF 15, 19. This technique is presented as bilaminar, and the recession would be covered by two tissue layers: the connective tissue graft and the LPF.
With respect to the LPF technique evolution in root coverage, the purpose of this study was to report a clinical case of root coverage of adjacent gingival recessions with subepithelial connective tissue graft (SCTG) associated with double LPF.
Case report
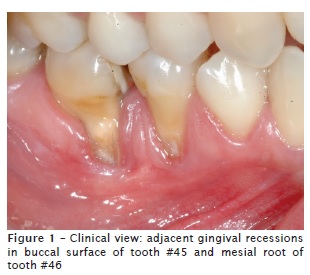
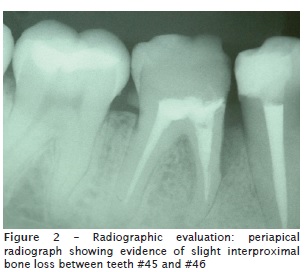
The patient described in this case report gave her consent for publication. Patient JMM, female, 45 years old, sought treatment with the main complaint of sensitivity while brushing in the right lower teeth region. At the intraoral clinical examination, Miller Class III adjacent gingival recessions were noticed in the buccal face of the right mandibular second premolar and mesial root of right mandibular first molar (figure 1). During the radiographic examination, a slight interproximal bone loss was also verified between the same teeth (figure 2).
Based on the clinical and radiographic data obtained, it was concluded that the recessions had a traumatic origin from brushing with the presence of thin periodontium in the region. The patient was then submitted to basic periodontal treatment with scaling and root planning and oral hygiene education. After four weeks, surgical periodontal treatment was performed using a culmination of a double LPF with tunnel SCTG under the interproximal papilla between the right mandibular second premolar and first molar.
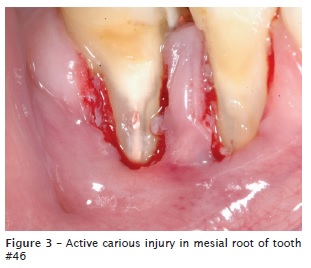
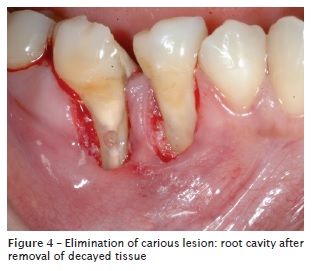
Initially, extraoral and intraoral antisepsis and anesthesia of lower alveolar, lingual, and oral nerves was achieved using mepivacaine hydrochloride 20 mg/mL with epinephrine 0.01 mg/ (Mepivalem AD, Dentsply Pharmaceutical, Catanduva, Brazil). With a 15C scalpel blade (Swann-Morton LTD, Sheffield, England), a gingival collar of approximately 1.5 mm was harvested from around the right mandibular second premolar recession and the mesial root of the right mandibular first molar, with the purpose of improving flap attachment in the recipient area. During this incision, an internal bevel was performed on the distal region of the right mandibular second premolar and on the mesial region of the right mandibular first molar. At that moment, the presence of an active carious injury was observed on the mesial root of the first molar (figure 3) and required repair, causing a communication with the endodontically treated root canal (figure 4). The root cavity was restored with resin-modified glass ionomer cement (Vitro Fil LC, Nova DFL, Rio de Janeiro, Brazil) (figure 5), followed by root planning with finishing diamond burs (KG Sorensen, Medical burs, Cotia, Brazil) and Gracey curettes (Hu-Friedy Co. Inc., Chicago, United States). The roots were conditioned for two minutes with cotton pellets soaked with 100 mg/ml tetracycline hydrochloride solution, followed by abundant irrigation with saline solution 25.
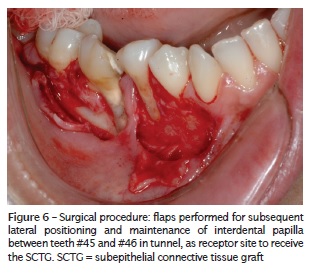
Incisions were then performed with a 15C scalpel blade (Swann-Morton LTD, Sheffield, England) to obtain a mesial to distal flap on the right mandibular second premolar root and a distal to mesial flap on the mesial root of the right mandibular first molar. Full-thickness flaps were obtained in the region near to the recession defects and partial-thickness flaps in proximal donor areas to avoid bone exposure in the donor site. The more distal edges of the donor area (with the donor area being the mesial surface of the right mandibular second premolar and distal surface of the mesial root of the right mandibular first molar) were scarified with an external bevel in order to expose the connective tissue (figure 6). The interproximal papilla between both teeth remained attached to the bone crest level. At its base, the tunnel technique was thoroughly carried out with a 15C scalpel blade (Swann-Morton LTD, Sheffield, England) parallel to the cortical bone to avoid flap fenestration and to allow SCTG positioning under the papilla (figure 6).
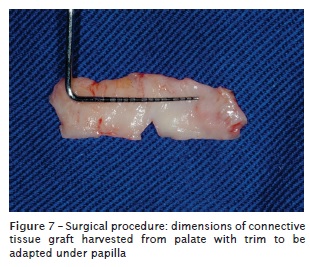
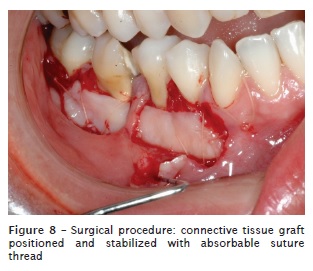
With a new 15C scalpel blade (Swann-Morton LTD, Sheffield, England), the connective tissue graft was harvested from the palate by the trapdoor technique, stretching out between premolars and right side second molar 19. The extension of the graft to be harvested was between the relaxing incisions and was determined by the mesiodistal width of the region being covered (figure 7) 13. During graft harvest, an incision was performed in the three sides of a rectangle, preserving the fourth side facing the palate center so as to keep the pedicle intact, and extending the graft deeply in the palate up to the desired graft height. After the incisions, a f lap with a movable base that allowed surgical access to harvest connective tissue of approximately 1.5 mm was obtained. A minimum distance of 2 mm from the gingival edge was respected. The SCTG was carefully harvested and subsequently tunneled under the preserved papilla and onto the exposed root surfaces, where it was stabilized in close contact with the adjacent tissues through sutures with 5.0 absorbable surgical threads (Ethicon, Johnson & Johnson, São José dos Campos, Brazil). The coronal graft margin was stabilized at the level of the cementoenamel junction, and its apical edge exceeded the bottom of the bone dehiscence defects bottom by 3 mm (figure 8). In the palate donor area, sutures were also placed to protect the underlying connective tissue and to minimize patient postoperative discomfort.
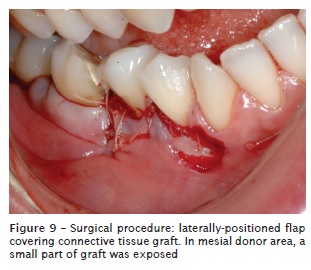
Next, the flaps were laterally positioned over the SCTG, covering a majority of the area. The flaps were sutured so that they were static to the alveolar mucous membrane during a traction test (figure 9). The donor and recipient areas were protected with surgical cement for one week to protect against possible mechanical traumas. The patient was instructed to take 500 mg amoxicillin, 1 pill every 8 hours, for seven days (Medley Indústria Farmacêutica Ltda, Campinas, Brazil), 100 mg nimesulide, 1 pill every 12 hours, for three days (Medley Indústria Farmacêutica Ltda, Campinas, Brazil), 500 mg sodium dipyrone, 40 drops every 6 hours, for pain (Medley Indústria Farmacêutica Ltda, Campinas, Brazil) and perform mouth washes with 0.12% chlorhexidine digluconate, twice a day for 14 days (Periogard®, Colgate-Palmolive Company, São Paulo, Brazil).

Results
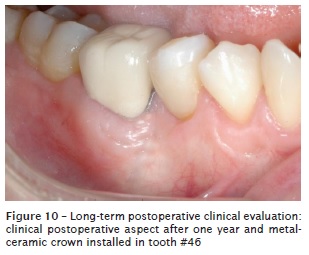
After seven days of the surgical procedure, the patient returned for the removal of sutures, and presented an adequate initial clinical condition of repair in the area. Four months after the operation, a metallic nucleus and metallic-ceramic prosthesis was constructed for the right mandibular first molar. After one year, it was possible to observe the almost complete coverage of recessions, an increase of the keratinized tissue band and the absence of hypersensitivity during brushing (figure 10).
Discussion
The treatment of gingival recessions still represents a great challenge in the everyday clinic. Despite the fact that to this day there are several techniques reviewed in the literature for root coverage 11, 17, 19, the periodontal plastic surgery field still needs techniques that meet the esthetic needs of professionals and patients.
The success of the root coverage procedure, which would eliminate its reoccurrence, depends on the elimination and control of gingival recession etiology 3, the interproximal bone level, and especially the choice of best surgical coverage technique for each case. These parameters could guarantee predictable clinical results. The LPF combined with SCTG was chosen in this clinical case due to the good periodontal conditions of the adjacent region of the recession, the appropriate keratinized gingival band and normal interproximal bone height, which allowed the surgical technique achievement. In addition, the SCTG technique produces a greater success rate in relation to root coverage when compared to other techniques for both healthy and decayed 8, restored or unrestored teeth 7.
Due to the presence of an active carious injury in the mesial root of the right mandibular first molar during the surgical procedure, restoration with resin-modified glass ionomer cement was necessary. Alkan et al. 2 in a case report concluded that SCTG can be successfully performed to treat gingival recession associated with a glass ionomer-restored root surface. Martins et al. 16 evaluated histologically the biocompatibility of resin-modified glass ionomer cement restorations after root coverage on restored root surfaces. These authors reported that the formation of an extensive junctional epithelium, with the absence of inflammation or insertion of connective tissue, predominantly occurred over restoring materials. The clinical result observed in the present report corroborate with this findings.
It is also important to emphasize that in this clinical case, the roots were submitted to scaling and planning and an application of tetracycline hydrochloride (100 mg/ml saline solution) during two minutes, prior to the coverage. The choice of tetracycline was because this solution reacts with the tooth hard tissues and acts as an antimicrobial agent in the formation of the bacterial biofilm, delaying and reducing the collagenolytic activity of bacterial endotoxins 8.
The tunnel technique associated with the SCTG and LPF was used due to the necessity of adjacent gingival recession coverage, to facilitate suture and stabilization of the connective graft. The use of the tunnel technique not only preserved papillae height between defects, but also maintained an appropriate blood supply to the graft 23. The surgical trauma in the recipient area was minimal, which contributes to the lateral and papillary graft vascular nutrition 22. This technique produced predictable and versatile results for root coverage, restoring the morphology of the gingival tissue in the region.
According to Hürzeler and Weng 12, the trapdoor technique used for connective tissue graft harvesting produces a type of incision that favors scarring and minimizes patient morbidity in the postoperative period, due to covering of the surgical area by the flap epithelium. In the current study, a 2 mm minimum distance from the gingival edge was respected during the incision to avoid gingival recessions in the donor area without gingival outline alterations, in addition to excluding from the flap important anatomical structures, such as the palatine nerve and artery.
Another advantage of the combination of SCTG and LPF techniques is the coverage of the avascular area of the recipient site by the flap, in addition to increased predictability, good esthetics and root coverage results. There is also the added benefit of a greater chance of graft survival and an increase or induction of keratinized tissue. The excellent esthetic result is obtained due to gingival tissue of the adjacent flap, which is a similar tissue to its surrounding recipient area, being transferred to the treatment site. In this study, the gingival marginal position after the graft appeared stable and in time the grafted tissue will match the adjacent tissue with regards to color and texture 13.
A part of the connective graft remained exposed, and this area epithelized quickly from the wound edges. If at least two-thirds of the graft is covered by the flap, the uncovered remaining third will remain on the exposed root, due to double blood supply of the periosteum situated below and laterally to the graft and LPF 13. If the root coverage obtained in the first weeks was not complete, it is suitable to wait to evaluate the result, since creeping attachment might occur, which is the migration of tissue in a coronal direction after scar maturation in subsequent months 10. According to Harris 10, creeping attachment can be observed within six months, but it can occasionally take up to one or two years 6.
The keratinized tissue created in the recipient site comes from the donor area adjacent to the recession defects and to the connective tissue graft. For the LPF, a keratinized tissue band apical to the recession is not necessary. At the end of the intervention, the presence of adequate keratinized tissue thickness covering the roots was noticed. The gingival volume gain present in this case is just one of the favorable aspects obtained by the applied technique.
Due to the use of a partial-thickness flap in the region of the mandibular right second premolar, there was no incidence of bone exposure, which might cause postoperative pain or gingival recession in the donor site. In this case, a small part of the SCTG was exposed, improving the keratinized tissue volume in the vestibular region of the mandibular right second premolar. It´s even important to report that the flap bevel inversions 4 were used to allow better adaptation at the moment of suture, in order to avoid flap superposition on the recipient area, and to reduce the incision line. This technical aspect favored better esthetics, and allowed greater proximity of the flap to the exposed root, reducing the risk of recurrence and suture dehiscence.
Despite the root coverage predictability of Miller Class III recessions be only partial in other studies, satisfactory coverage was obtained by the applied surgical technique in this case report. A total coverage of recessions could not be obtained because the level of periodontal tissue support in the proximal surfaces of the right mandibular second premolar and first molar was insufficient.
Appropriate choice of techniques and patient compliance to the periodontal support therapy led to treatment success and periodontal health maintenance in the region during the whole followup period. The association of surgical coverage techniques, in addition to technical requisites, has contributed to elevated root coverage rates, with better esthetic and functional results in long-term evaluations 9, 20.
In conclusion, the SCTG combined with the double LPF contributed to coverage of most exposed adjacent root surfaces in the posterior jaw region with an increased keratinized gingival band and the el iminat ion of init ial dent in hypersensitivity.
References
1. Akkaya M, Böke F. Shallow localized gingival recession defects treated with modified coronally repositioned flap technique: a case series. Eur J Dent. 2013 Jul;7(3):368-72. [ Links ]
2. Alkan A, Keskiner I, Yuzbasioglu E. Connective tissue grafting on resin ionomer in localized gingival recession. J Periodontol. 2006 Aug;77(8):1446-51.
3. Ando K, Ito K, Murai S. Improvement of multiple facial gingival recession by non-surgical and supportive periodontal therapy: a case report. J Periodontol. 1999 Aug;70(8):909-13.
4. Bosco AF, Milanezi LA, Passanezi E. Contribution to the technique of covering the exposed roots. Rev Reg Araçatuba Assoc Paul Cir Dent. 1990;10:9-12.
5. Chrysanthakopoulos NA. Gingival recession: prevalence and risk indicators among young greek adults. J Clin Exp Dent. 2014 Jul 1;6(3):243-9.
6. Deliberador TM, Martins TM, Furlaneto FA, Klingenfuss M, Bosco AF. Use of the connective tissue graft for the coverage of composite resinrestored root surfaces in maxillary central incisors. Quintessence Int. 2012 Jul;43(7):597-602.
7. Goldstein M, Nasatzky E, Goultschin J, Boyan B, Schwartz Z. Coverage of carious roots by a subepithelial connective tissue graft. Am J Dent. 2002 Jun;15(3):143-8.
8. Greenwell H, Bissada NF, Henderson RD, Dodge JR. The deceptive nature of root coverage results. J Periodontol. 2000 Aug;71(8):1327-37.
9. Grupe HE, Warren Jr RF. Repair of gingival defects by a sliding flap operation. J Periodontol. 1956 Apr;27(2):92-5.
10. Harris RJ. Creeping attachment associated with the connective tissue with partial-thickness double pedicle graft. J Periodontol. 1997 Sep;68(9):890-9.
11. Harris RJ. The connective tissue and partial thickness double pedicle graft: a predictable method of obtaining root coverage. J Periodontol. 1992 May;63(5):477-86.
12. Hürzeler MB, Weng D. A single-incision technique to harvest subepithelial connective tissue grafts from the palate. Int J Periodontics Restorative Dent. 1999 Jun;19(3):279-87.
13. Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985 Dec;56(12):715-20.
14. Marini MG, Greghi SL, Passanezi E, Sant'ana AC. Gingival recession: prevalence, extension and severity in adults. J Appl Oral Sci. 2004 Sep;12(3):250-5.
15. Martins TM, Bosco AF, Gazoni GG, Garcia SF. Laterally positioned f lap associated with subepithelial connective tissue graft for coverage of isolated gingival recession. RSBO 2011 Oct;8(4): 464-8.
16. Martins TM, Bosco AF, Nóbrega FJ, Nagata MJ, Garcia VG, Fucini SE. Periodontal tissue response to coverage of root cavities restored with resin materials: a histomorphometric study in dogs. J Periodontol. 2007 Jun;78(6):1075-82.
17. Miller Jr PD. A classification of marginal tissue recession. Int J Periodontics Restorative Dent. 1985;5(2):8-13.
18. Moka LR, Boyapati R, Swarna C, Putcha M. Comparison of coronally advanced and semilunar coronally repositioned flap for the treatment of gingival recession. J Clin Diagn Res. 2014 Jun;8(6): 4-8.
19. Nelson SW. The subpedicle connective tissue graft. A bilaminar reconstructive procedure for the coverage of denuded root surfaces. J Periodontol. 1987 Feb;58(2):95-102.
20. Rappaport NH, Netscher DT. Plastic surgery techniques applicable to periodontal flap surgery. Periodontol 2000. 1996 Jun;11:95-102.
21. Santamaria MP, Suaid FF, Casati MZ, Nociti FH, Sallum AW, Sallum EA. Coronally positioned flap plus resin-modified glass ionomer restoration for the treatment of gingival recession associated with non-carious cervical lesions: a randomized controlled clinical trial. J Periodontol. 2008 Apr;79(4):621-8.
22. Santarelli GA, Ciancaglini R, Campanari F, Dinoi C, Ferraris S. Connective tissue grafting employing the tunnel technique: a case report of complete root coverage in the anterior maxilla. Int J Periodontics Restorative Dent. 2001 Feb;21(1):77-83.
23. Sanz M, Simion M, Working Group 3 of the European Workshop on Periodontology. Surgical techniques on periodontal plastic surgery and soft tissue regeneration: consensus report of Group 3 of the 10th European Workshop on Periodontology. J Clin Periodontol. 2014 Apr;41:92-7.
24. Tarnow DP. Semilunar coronally repositioned flap. J Clin Periodontol. 1986 Mar;13(3):182-5.
25. Wikesjö UM, Claffey N, Christersson LA, Franzetti LC, Genco RJ, Terranova VP et al. Repair of periodontal furcation defects in beagle dogs following reconstructive surgery including root surface demineralization with tetracycline hydrochloride and topical fibronectin application. J Clin Periodontol. 1988 Jan;15(1):73-80.
 Correspondence:
Correspondence:
Thiago Marchi Martins
Faculdade de Odontologia
Universidade Federal de Pelotas
Rua Gonçalves Chaves, 457
CEP 96015-560 – Pelotas – RS – Brasil
E-mail: tmperio@hotmail.com













