RSBO (Online)
ISSN 1984-5685
RSBO (Online) vol.12 no.2 Joinville abr./jun. 2015
Case Report Article
Symptomatic mucous retention cysts of the maxillary sinus: case report
Eduardo Sanches GonçalesI; Andréia Guedes Barreto GonçalesI; Emanuelle da Silva LimaII; Julierme Ferreira RochaII; José Wilson NoletoII; Eduardo Hochuli-VieiraIII
I Department of Stomatology, School of Dentistry of Bauru, University of São Paulo – Bauru – SP – Brazil
II Department of Oral and Maxillofacial Surgery, School of Dentistry, Federal University of Campina Grande, Campus Patos – Campina Grande – PB – Brazil
III Department of Oral and Maxillofacial Surgery, São Paulo State University Júlio de Mesquita Filho – Araraquara – SP – Brazil
ABSTRACT
The retention mucous cyst of the maxillary sinus is a benign lesion that occurs in the interior of the maxillary sinus due ductal obstruction. In the majority of the cases it is asymptomatic, and discovered on routine radiographic examinations. However, in some cases, this cyst can become large and cause symptoms as paresthesia, sensitivity to palpation, chronic headache, nasal blockage, and dizziness. Conservative treatment is conduct in most cases. Symptomatic retention cysts are treated by enucleation or curettage. Objective and case report: This study aimed to report a clinical case of symptomatic mucous retention cyst accidentally discovered in a patient treated by surgically-assisted rapid maxillary expansion. Conclusion: The curettage of the cyst allowed for the regression of symptoms and at 12 months postoperatively the patient is free of symptoms and no signs of recurrence of lesion were noted.
Keywords: cysts; maxillary sinus; mucocele.
Introduction
The mucous retention cyst of the maxillary sinus (MRCMS) is a benign and self-limiting injury, resulting from the leakage of mucus within the sinus mucosa due to ductal obstruction 4, 12. It has been suggested that MRCMS is of non-odontogenic origin, since it may also occur in dentate and edentulous patients. Nevertheless, Veltrini et al. 14 emphasized that periapical and periodontal disease associated with maxillary molars may be an important etiological factor for sinusitis and MRCMS.
As the MRCMS pathogenesis seems to be based on hypothesis, many denominations are attributed to this injury: pseudocyst, the retention cysts of the maxillary sinus, serous cyst, mucous cyst, benign maxillary mucous cyst or mucocele. Pseudocyst is one that has no epithelial lining showing fibrous connective tissue around the cystic content. However, the MRCMS presents epithelial lining, which seems to indicate that this is the correct name 7, 12.
MRCMS is commonly found in radiographic examinations performed for other reasons. The injury appears in panoramic and periapical radiographs of maxillary posterior teeth as a homogeneous radiopacity, outlined, dome-shaped, hemispherical or circular, of variable dimensions, most frequently located on the floor of the maxillary sinus, and preserving the sinus walls. In cases which the retention cyst completely fills the maxillary sinus, the radiographic interpretation becomes difficult, and complete blurring can be interpreted as maxillary sinusitis 7, 8, 10.
No treatment should be inst ituted for MRCMS especially when the lesion is small and asymptomatic. It is suggested only radiographic monitoring, since most do not evolve and some regress spontaneously. In larger or symptomatic lesions, treatment should be performed by enucleation or curettage 2, 3, 4, 5, 14. It is proposed in this paper to present a clinical case of symptomatic MRCMS accidentally discovered during surgically assisted maxillary expansion.
Case report
A patient, male, leucoderm aged 33 year-old, presenting transverse maxillary deficiency, was referred to treatment due to orthodontic indication to undergo surgically assisted maxillary expansion (SAME).
At medical history it was found that the patient was in good general health, reporting only difficulty to breathing, which was why he sought orthodontic treatment recommended by the ENT.
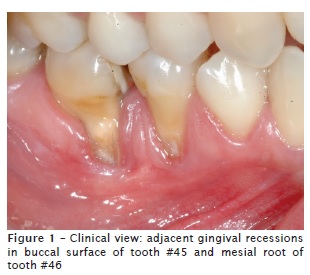
Clinical examination revealed maxillary atresia and bilateral posterior crossbite (figure 1).
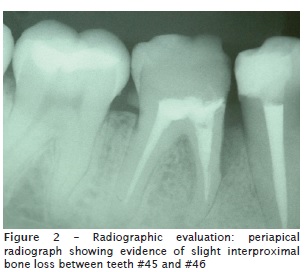
The panoramic radiograph showed discrete diffuse opacification of the right maxillary sinus (figure 2).
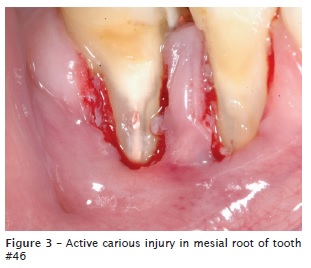
During SAME, performed according to the technique suggested by Betts et al. 1, and the osteotomy performed in the zygomatic process of the maxilla, yellowish content was observed (figure 3) and removed by curettage.
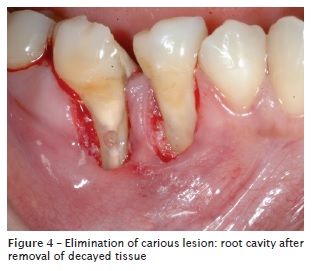
Such content, with approximately dimensions of 6.0 x 5.5 x 2.5 cm, presented gelat inous consistency and was sent to histopathological examination, and diagnosed by mucous cysts of the maxillary sinus. After the removal of the lesion, the sinus cavity was unobstructed and clean (figure 4), which allowed the routine care with the surgical wound, ending with the suture. At the immediate postoperative period, the patient reported significant improvement in their breathing.
Microscopically, a virtual cystic cavity was observed, lined by ciliated cylindrical pseudostratified epithelium with underlying layer of loose connective tissue, rich in delicate blood vessels. In between, foci of intense mononuclear infiltrate were observed (figure 5).

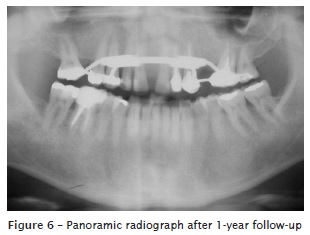
After twelve months postoperat ively, the panoramic radiography showed the structures with normal aspects (figure 6).
Discussion
The MRCMS is not a phenomenon of the maxillary sinus and its pathogenesis is not fully known. Nevertheless, previous infection of the sinus mucosa appears to be important in the pathogenesis of this cyst, especially the odontogenic infection. An intense inflammation around the duct of the sinus mucous glands coating can change its integrity and lead to obstruction. Thus, respiratory infections such as maxillary sinusitis favor the development of MRCMS 4, 7, 12.
Although most MRCMS are asymptomatic and discovered by the radiographic examinations for other purposes 6, the MRCMS may present eventual signs and symptoms, as migraine, nasal congestion, dizziness, paresthesia, yellow f luid drainage, respiratory allergy, sensitivity to palpation on the anterior wall of the maxillary sinus, leading the individual to seek treatment 5. It seems clear that these symptoms are preferably perceived by individuals with larger cysts, as in the case reported herein, but complaining only on difficulty breathing.
Radiographically, smaller retention cysts show as dome-shaped or rounded, but occasionally they completely fill the sinus cavity, making it difficult its radiographic diagnosis, for generating fine diffuse opacification of the image of the maxillary sinus 3, 10, 13. In the reported case, the lesion occupied almost entirely the right maxillary sinus, which presented a diffuse opacification not suggestive of cyst, but consistent with chronic maxillary sinusitis. Computed tomography is indicated for cases in which the diagnosis through conventional examinations is limited 7, 8, 11, 13.
The differential diagnosis of MRCMS should be done with other injuries that produce sinus opacification, as apical radicular cyst, odontogenic tumor, keratocyst ic, dent igerous cyst, even considering that these injuries can cause intraoral signs and symptoms, with changes in alveolar process. In this region, a variety of cancers may appear; the epidermoid carcinoma seems to be the most common one and should not be confused with the MRCMS 5, 14. The maxillary ciliated surgical cyst (MCCS) stems from the proliferation of sinus epithelium trapped in the wound, during invasive procedures OF the maxillary sinus. It is also called secondary mucocele and is a late complication of sinusectomies and maxillary orthognathic surgeries.
Small lesions may have spontaneous regression 2; however, the greatest symptomatic cyst and must be removed by surgical treatment, preferably by curettage or maxillary sinusectomy 3, 4, 14. In this case, the sinus operation was timely, taking advantage of the SAME procedure. The behavior of the injury is eminently benign, allowing its satisfactory removal, even with limited access, that is, the bone window in the maxillary zygomatic process.
The immediate improvement in the patient's breathing corroborates data that emphasize the need for treatment of symptomatic mucous retention cysts of the maxillary sinus. Obviously, this improvement was not the result of the maxillary expansion procedure since it was immediate, although Ribeiro Júnior et al. 9 have asserted that the SAME may result in improved breathing pattern.
Conclusion
The correct clinical and radiographic diagnosis of MRCMS is mandatory in symptomatic cases, as it seems to be decisive for treatment indication. The clinical and radiographic monitoring of MRCMS cases is, however, the most common procedure, as small and asymptomatic lesions are more prevalent and require no treatment.
References
1. Betts NJ, Vanarsdall RL, Barber HD, Higgins- Baber K, Fonseca RJ. Diagnosis and treatment of transverse maxillary deficiency. Int J Adult Orthod Orthognath Surg. 1995;10(2):75-96. [ Links ]
2. Bhattacharyya N. Do maxillary sinus retention cysts reflect obstructive sinus phenomena? Arch Otolaryngol Head Neck Surg. 2000;126(11):1369-71.
3. Bugarelli AF, Silva ABM, Paulino SM, Watanabe PCA, Pardini LC. Cisto de retenção do seio maxilar – considerações para o clínico geral. Rev Assoc Paul Cir Dent. 2002;56(3):178-81.
4. Garcia Júnior IR, Magro Filho O, Ramos RQ, Bassi APF, Carvalho CA. Cisto mucoso do seio maxilar – revisão de literatura e relato de caso clínico. Revista BCI. 2000;28(7):59-62.
5. Hadar T, Shvero J, Nageris BI, Yaniv E. Mucous retention cyst of the maxillary sinus: the endoscopic approach. Br J Oral Maxillofac Surg. 2000;38(3):227-9.
6. Mardinger O, Manor I, Mijiritsky E, Hirshberg A. Maxillary sinus augmentation in the presence of antral pseudocyst: a clinical approach. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:180-4.
7. Parks ET. Cone beam computed tomography for the nasal cavity and paranasal sinuses. Dent Clin North Am. 2014;58(3):627-51.
8. Rege ICC, Sousa TO, Leles CR, Mendonça EF. Occurrence of maxillary sinus abnormalities detected by cone beam CT in asymptomatic patients. BMC Oral Health. 2012;12(30):1-7.
9. Ribeiro Júnior PD, Gonçales ES, Souza PCU, Nary Filho H, Luz JGC. Avaliação clínica dos procedimentos de expansão cirurgicamente assistida da maxila (ECAM). R Dental Press Ortodon Ortop Facial. 2006;11(1):44-59.
10. Rodrigues CD, Freire GF, Silva LB, Fonseca da Silveira MM, Estrela C. Prevalence and risk factors of mucous retention cysts in a Brazilian population. Dentomaxillofac Radiol. 2009;38(7):480-3.
11. Rodrigues CD, Silveira MF, Alencar AHG, Silva MAGS, Mendonça EF, Estrela C. Three dimensional images contribute to the diagnosis of mucous retention cyst in maxillary sinus. Med Oral Patol Oral Cir Bucal. 2013;18(1):151-7.
12. Soikkonen K, Ainamo A. Radiographic maxillary sinus findings in the elderly. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80(4):487-9.
13. Vallo J, Taipale LS, Huumonen S, Soikkonen K, Norblad A. Prevalence of mucosal abnormalities of the maxillary sinus and their relationship to dental disease in panoramic radiography: results from the Health 2000 Hearth Examination Survery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(3):80-7.
14. Veltrini V, Ferreira O, Tostes D. Mucosal cysts of the maxillary sinus: a literature review. Med Oral. 2001;6(3):185-91.
 Correspondence:
Correspondence:
Julierme Ferreira Rocha
Faculdade de Odontologia
Universidade Federal de Campina Grande
Centro de Saúde e Tecnologia Rural
Avenida dos Universitários, s/n.º – Rodovia Patos/Teixeira, km 1 – Jatobá
CEP 58700-970 – Patos – PB – Brasil
E-mail: juliermerocha@hotmail.com













