Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.12 no.3 Joinville Jul./Set. 2015
Literature Review Article
Can quality of life index measure oral health over the years? A systematic review
Paulo Roberto SilvaI; Márcia Cristina LopesI; Wellington M. ZaitterII; Edgard Michel CrosatoI
I Department of Social Dentistry, University of São Paulo – São Paulo – SP – Brazil
II Positivo University– Curitiba – PR – Brazil
ABSTRACT
Introduction:The referred quality of life has been increasingly used in dental studies to measure the impact that the dental treatment can cause on the individuals. However, there are few studies that monitor longitudinally this condition. Objective: The aim of this study was verify the behavior of the impact of the quality of life of the individuals through a systematic review on observational or interventional longitudinal studies. Literature review: The articles were selected in the period from February 5th to March 15th of 2014, with selection criteria: Objectives of the study, longitudinal studies, assessment of the quality of life of the studied population. The determination of the 24 selected articles was conducted by two examiners and revised together. Results: The study generated five tables related to common areas of dentistry: prosthesis, dental caries, geriatric health, orthodontics and oral oncology. The impact achieved in the quality of life of the people with the treatment was not maintained over the years. Conclusion: The quality of life of the individuals is little influenced by dental treatments over the years, with the exception of the cases of prosthesis and severe orthodontic treatments. The impact of the quality of life seems to be a measurement of occasional use, preferably carried soon after some oral intervention and not for longitudinal studies in which other factors cannot be controlled..
Keywords: longitudinal studies; oral health; quality of life.
Introduction
Quality of life related to the oral health is a term used at the present time to describe or quantify the level of impact of the oral health on the quality of life of an individual. The measurements initially designed as subjective or socioeconomic indexes of the oral health, are now used as reference measurements of the impact on the quality of life. In this context, the functional and psychosocial impacts of perceived dental problems, generated by a composite score, may suggest the perceived changes in the life of the individual.
An issue that is still approached ref lects the concern of the studies to show how these measurements were developed 20,30,35,37, however the frequency of the functional and psychosocial impacts of the oral diseases may still establish equivocally the meaning and the importance of this impact on the quality of life 24. This can be well defined after the conclusion of a dental treatment 33, as well as the measurement of a direct relation between the social impact and the dental care necessity perceived by the patient 26. However, how these oral disorders really affect the quality of life of an individual over the time have not been clearly elucidated in the literature yet. That is, what happens with the quality of life indexes of these individuals after the treatment or re-treatment and after some years of the oral interventions. In face of what is exposed, this study aimed at answering through a systematic review the behavior of the quality of life impact described in observational longitudinal studies or of the intervention in the individuals.
Data collection and analysis
For the conduction of this systematic revision, the articles were selected in the period from February 5th to March 15th of 2014, by two independent examiners (Kappa > 0.8). The researched databases were: Medline (1997-2014), Scopus, Cochrane Library and Lilacs, in English, Portuguese and Spanish. The keywords used were: quality of life, oral health and longitudinal studies. The criteria of inclusion in this first stage were: Objectives of the study, longitudinal studies, assessment of the quality of life of the studied population. 71 articles were detected at Scopus (limited to dentistry), 548 at Medline and six at Lilacs. Being that no reference was found at Cochrane Library. Of these, 35 articles were selected initially without duplicated. For this stage, the exclusion criteria were: abstracts not in accordance with the objective of the research (Flowchart). In an agreement, four articles were excluded by the two examiners and the reviewer of the study after abstract analyses.
Making use of pre-structured instruments in full text, the 31 selected articles brought the following complementary information: authors, local where the study was carried out, year of the publication, journal, period of the study, objective of the study, age or age range of the studied population, quality of life index used, main findings and/or conclusions.
Of these, seven failed to meet the inclusion criteria. Reasons for exclusion were: three studies were not longitudinal 1,18,19, one study did not specify well the quality of life 28, one study was the description of a new index 11, one study was not related to oral health 21 and one study used the same data 9.
At the end, 24 articles were selected for a careful analysis and reported according to systematic review, for presenting similar characteristics the authors found it convenient to divide the subjects by common areas of the dentistry. This way, the articles were grouped in five big tables according to the affinity of the area once, with this division, more specific data was generated for the conclusions.
Results and Discussion
On the table I, regarding the dental prosthesis, the quality of life indexes presented improvements and are maintained under the initial one after some years. In either cases, with prosthesis supported or not by implants, there is a decrease in the quality of life indexes 3,2,4,8,17,23,26,29,36. However, in the implant supported patients the improvement in the quality of life was higher 3,4,8,29. For treatments of conventional denture, the patients who requested prosthesis over the implant, but received conventional prosthesis, obtained few changes in the quality of life 3. However, in patients who requested conventional prosthesis and received them, there was an improvement in the quality of life 23. Removable dentures require a longer period for the improvement in the quality of life of the patients 17,36. According to the authors, this is the adaptation time. The improvement in the quality of life can also be associated with the desire or personal expectations that suffer interferences with the time 23.
By the results found in table II, children without dental caries have a quality of life, in general, better than the ones who have dental caries 13. However, the earlier treatment of these children with caries improves their quality of life according to the parents along the time. Now, in adolescents, the presence or absence of dental caries does not affect their quality of life16. However, according to the author, the lack of a strong association between the incidence of caries and the quality of life along the three years in these adolescents, also raises questions about the capacity of an index to reflect changes in the experience of caries and its effect on the quality of life in this population.
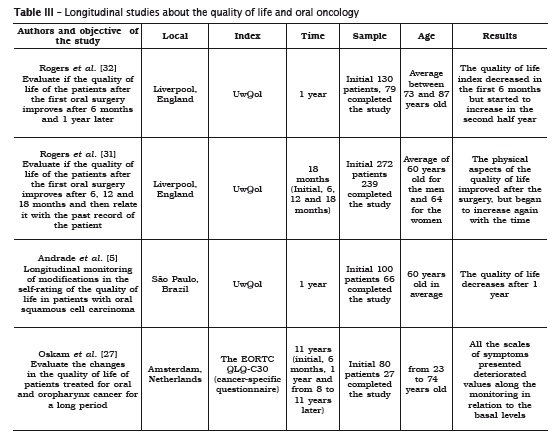
In the area of oral oncology (table III) the quality of life seems to be more associated to the size of the injuries and their recovery expectations. Being that the physical aspects of the quality of life always reduce after the surgery they, however, start to return to the normality after 6 months or 1 year 5,27,31,32. Factor associated mainly to the complaint about difficulties in the mastication, besides difficulties to swallow, pain and lack of saliva 5. Suggesting that the oral functional deficiency continues even after the surgeries 27.
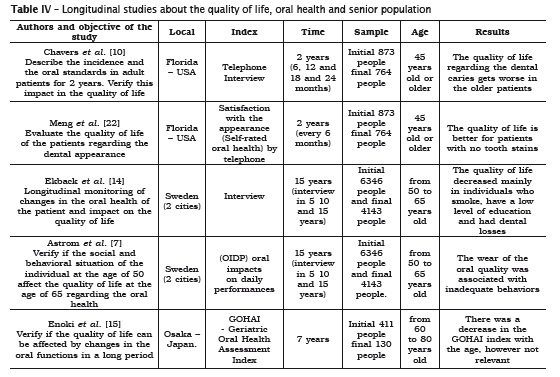
Longitudinal studies about the quality of life, oral health and more senior citizens (table IV) showed that changes in the oral clinical status along the time are reflected directly on the quality of life of these people 7,10,14,15,22. In this case in especial, two studies were maintained, due to their use of different measures of the quality of life of these same studied people 7,22. Social behaviors such as the low educational level and personal behaviors like smoking, directly affect the oral health-related and general quality of life of this population 7,14. With the increasing age, other health problems also affect the quality of life of this population 10,15. However, for the oral health the main complaints regarding the decrease in this quality of life are: toothache, abscesses and difficulties in the mastication due to tooth losses. Patients satisfied with the dental appearance describe a better quality of life 22.
Longitudinal studies about the quality of life and orthodontics (table V) showed that only patients with severe orthodontic problems presented changes in the quality of live along the years, mainly regarding the women 6,12,25,34,38. In the surgical cases, the quality of life improves only after the performance of the orthognathic surgery 12,25. It was surprising the conclusion that only the orthodontic treatment does not influence the quality of life in adolescent or adult patients 6,38. Nevertheless, the orthodontic treatment improves the appearance, oral function, health and social well-being of the people.
Conclusion
By means of the proposed objective of the study, it is observed that the oral health-related quality of life of the people undergo changes during the entire studied period. Prosthesis and severe orthodontic treatments are the procedures that can maintain the impact on the improvement of the quality of life the longer. Our study could not determine the exact time in which these quality of life measurements start to recede, so other studies shall be conducted verifying this question. Some cohort studies which also generate results in defined demographic populations should be seen with endorsement. Due to the fact that these articles use measurements in scales, it is difficult the comparison of all the studies as a single one, as well as a single conclusion, but the study suggests us a scientific evidence that the quality of life of the people is little influenced by dental treatments along the years, with the exception in the case of prosthesis and orthodontic severe dental treatments. In summary, oral health-related quality of life is a measurement that should be used in a timelier manner, preferably soon after some oral intervention and not for longitudinal studies in which other factors cannot be controlled.
Implications for research
Studies that aim at measuring the impact of the quality of life make use of indexes that suffer influence from both the lifestyle that the people and different habits and places. Consequently, studies with more uniform groups are valid for assessing the impact that the dentistry can cause on the life of these people along the time. The use of different instruments of quality of life can measure the additional positive aspects of patients regarding their perceptions of the oral health in specific cases (such as of the prosthesis), as well as in negative aspects (such as of misguided treatments). Articles that can better elucidate these aspects, in which it is also achieved the homogeneity of the dental treatment and successive collections regarding the quality of life of these people in more controlled periods become necessary.




References
1. Agou S, Locker D, Streiner DL, Tompson B. Impact of self-esteem on the oral-health-related quality of life of children with malocclusion. Am J Orthod Dentofacial Orthop. 2008 Oct;134(4): 484-9. [ Links ]
2. Alfadda SA, Attard NJ, David LA. Five-year clinical results of immediately loaded dental implants using mandibular overdentures. Int J Prosthodont. 2009 Jul-Aug;22(4):368-73.
3. Allen PF, McMillan AS, Walshaw D. A patientbased assessment of implant-stabilized and conventional complete dentures. J Prosthet Dent. 2001 Feb;85(2):141-7.
4. Allen PF, McMillan AS. A longitudinal study of quality of life outcomes in older adults requesting implant prostheses and complete removable dentures. Clin Oral Implants Res. 2003 Apr;14(2):173-9.
5. Andrade FP, Antunes JL, Durazzo MD. Evaluation of the quality of life of patients with oral cancer in Brazil. Braz Oral Res. 2006 Oct- Dec;20(4):290-6.
6. Arrow P, Brennan D, Spencer AJ. Quality of life and psychosocial outcomes after fixed orthodontic treatment: a 17-year observational cohort study. Community Dent Oral Epidemiol. 2011 Dec;39(6):505-14.
7. Astrom AN, Ekback G, Ordell S, Unell L. Social inequality in oral health-related quality-of-life, OHRQoL, at early older age: evidence from a prospective cohort study. Acta Odontol Scand. 2011 Nov;69(6):334-42.
8. Berretin-Felix G, Nary Filho H, Padovani CR, Machado WM. A longitudinal study of quality of life of elderly with mandibular implant-supported fixed prostheses. Clin Oral Implants Res. 2008 Jul;19(7):704-8.
9. Chavers LS, Gilbert GH, Shelton BJ. Racial and socioeconomic disparities in oral disadvantage, a measure of oral health-related quality of life: 24-month incidence. J Public Health Dent. 2002 Summer;62(3):140-7.
10. Chavers LS, Gilbert GH, Shelton BJ. Two-year incidence of oral disadvantage, a measure of oral health-related quality of life. Community Dent Oral Epidemiol. 2003 Feb;31(1):21-9.
11. Cunningham SJ, Garratt AM, Hunt NP. Development of a condition-specific quality of life measure for patients with dentofacial deformity: I. Reliability of the instrument. Community Dent Oral Epidemiol. 2000 Jun;28(3):195-201.
12. Cunningham SJ, Garratt AM, Hunt NP. Development of a condition-specific quality of life measure for patients with dentofacial deformity: II. Validity and responsiveness testing. Community Dentistry and Oral Epidemiology. 2002 Apr;30(2):81-90.
13. Cunnion D, Spiro A, Jones J, Rich S, Papageorgiou C, Tate A et al. Pediatric oral healthrelated quality of life improvement after treatment of early childhood caries: a prospective multisite study. J Dent Child (Chic). 2010 Jan-Apr;77(1): 4-11.
14. Ekback G, Nodrehaug-Astrom A, Klock K, Ordell S, Unell L. Satisfaction with teeth and life-course predictors: a prospective study of a Swedish 1942 birth cohort. Eur J Oral Sci. 2010 Feb;118(1):66-74.
15. Enoki K, Ikebe K, Matsuda KI, Yoshida M, Maeda Y, Thomson WM. Determinants of change in oral health-related quality of life over 7 years among older Japanese. J Oral Rehabil. 2013 Apr;40(4):252-7.
16. Foster Page LA, Thomson WM. Caries prevalence, severity, and 3-year increment, and their impact upon New Zealand adolescents' oralhealth- related quality of life. J Public Health Dent. 2012 Fall;72(4):287-94.
17. John MT, Slade GD, Szentpetery A, Setz JM. Oral health-related quality of life in patients treated with fixed, removable, and complete dentures 1 month and 6 to 12 months after treatment. Int J Prosthodont. 2004 Sep-Oct;17(5):503-11.
18. Katsoulis J, Nikitovic SG, Spreng S, Neuhaus K, Mericske-Stern R. Prosthetic rehabilitation and treatment outcome of partially edentulous patients with severe tooth wear: 3-years results. J Dent. 2011 Oct;39(10):662-71.
19. Kressin NR, Reisine S, Spiro A 3rd, Jones JA. Is negative affectivity associated with oral quality of life? Community Dent Oral Epidemiol. 2001 Dec;29(6):412-23.
20. Locker D. Measuring oral health: a conceptual framework. Community Dental Health. Mar 1988;5(1):3-18.
21. McGrath C, McMillan AS, Zhu HW, Li LS. Agreement between patient and proxy assessments of oral health-related quality of life after stroke: an observational longitudinal study. J Oral Rehabil. 2009 Apr;36(4):264-70.
22. Meng X, Gilbert GH, Litaker MS. Dynamics of satisfaction with dental appearance among dentate adults: 24-month incidence. Community Dent Oral Epidemiol. 2008 Aug;36(4):370-81.
23. Meng X, Gilbert GH. Predictors of change in satisfaction with chewing ability: a 24-month study of dentate adults. J Oral Rehabil. 2007 Oct;34(10):745-58.
24. Michel-Crosato E, Biazevic MGH, Crosato E. Relationship between dental fluorosis and quality of life: a population based study. Brazilian oral research. 2005 Apr-Jun;19(2):150-5.
25. Murphy C, Kearns G, Sleeman D, Cronin M, Allen PF. The clinical relevance of orthognathic surgery on quality of life. Int J Oral Maxillofac Surg. 2011 Sep;40(9):926-30.
26. Nuttall N, Steele J, Pine C, White D, Pitts N. Adult dental health survey: the impact of oral health on people in the UK in 1998. Br Dent J. 2001 Feb 10;190(3):121-6.
27. Oskam IM, Verdonck-de Leeuw IM, Aaronson NK, Witte BI, de Bree R, Doornaert P et al. Prospective evaluation of health-related quality of life in long-term oral and oropharyngeal cancer survivors and the perceived need for supportive care. Oral Oncol. 2013 May;49(5):443-8.
28. Peek CW, Gilbert GH, Duncan RP. Predictors of chewing difficulty onset among dentate adults: 24-month incidence. J Public Health Dent. 2002 Fall;62(4):214-21.
29. Petricevic N, Celebic A, Rener-Sitar K. A 3-year longitudinal study of quality-of-life outcomes of elderly patients with implant- and tooth-supported fixed partial dentures in posterior dental regions. Gerodontology. 2012 Jun;29(2):e956-63.
30. Reisine ST, Fertig J, Weber J, Leder S. Impact of dental conditions on patients' quality of life. Community Dentistry and Oral Epidemiology. 1989 Sep;17(1):7-10.
31. Rogers S, Kenyon P, Lowe D, Grant C, Dempsey G. The relation between health-related quality of life, past medical history, and American Society of Anesthesiologists' ASA grade in patients having primary operations for oral and oropharyngeal cancer. Br J Oral Maxillofac Surg. 2005 Apr;43(2):134-43.
32. Rogers SN, Lowe D, Fisher SE, Brown JS, Vaughan ED. Health-related quality of life and clinical function after primary surgery for oral cancer. Br J Oral Maxillofac Surg. 2002 Feb;40(1):11-8.
33. Rosenberg D, Kaplan S, Senie R, Badner V. Relationships among dental functional status, clinical dental measures, and generic health measures. Journal of Dental Education. 1988 Nov;52(11):653-7.
34. Rusanen J, Lahti S, Tolvanen M, Pirttiniemi P. Quality of life in patients with severe malocclusion before treatment. Eur J Orthod. 2010 Feb;32(1): 43-8.
35. Slade GD, Spencer AJ. Development and evaluation of the oral health impact profile. Community Dental Health. 1994 Mar;11(1):3-11.
36. Stober T, Danner D, Lehmann F, Seche AC, Rammelsberg P, Hassel AJ. Association between patient satisfaction with complete dentures and oral health-related quality of life: two-year longitudinal assessment. Clin Oral Investig. 2012 Feb;16(1):313-8.
37. Strauss RP, Hunt RJ. Understanding the value of teeth to older adults: influences on the quality of life. Journal of the American Dental Association. 1939 Jan;124(1):105-10.
38. Taylor KR, Kiyak A, Huang GJ, Greenlee GM, Jolley CJ, King GJ. Effects of malocclusion and its treatment on the quality of life of adolescents. Am J Orthod Dentofacial Orthop. 2009 Sep;136(3): 382-92.
 Corresponding author:
Corresponding author:
Paulo Roberto Silva
Faculdade de Odontologia – Universidade de São Paulo
Rua Lineu Prestes, 2.227 – Butantã
CEP 05508-000 – São Paulo – SP – Brasil
E-mail: paulorobertosilva@usp.br
Received for publication: June 19, 2015
Accepted for publication: July 24, 2015













