Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.12 no.3 Joinville Jul./Set. 2015
Case Report Article
Prosthetic rehabilitation using association of total and implant-supported total denture (Brånemark protocol) – case report
Rodrigo Lorenzi PoluhaI; Clóvis Lamartine de Moraes Melo NetoI; Sérgio SábioI
I Department of Dentistry, State University of Maringá – Maringá – Paraná – Brazil
ABSTRACT
Introduction: The rehabilitation with implant-supported fixed prosthesis is an effective therapy for the treatment of edentulous patients, especially for mandibles, following Brånemark protocol. Case report:A male patient, aged 62 years, fully edentulous, already had 05 implants, between mental foramen. The rehabilitative therapy employed used both maxillary total denture upper associated with mandibular implant-supported denture following Brånemark protocol. Conclusion: The implant-supported denture following Brånemark protocol is a viable alternative, providing stability to the denture, masticatory efficiency, and aesthetics. Each case should be carefully analyzed and planned to reach a successful treatment.
Keywords: dental implants; dental prosthesis; dental prosthesis, implantsupported.
Introduction
The functional and esthetic rehabilitation of edentulous patients has always challenged the dentists in clinical practice. The use of dental implants is of great value to provide the most clinically successful rehabilitation 5,14. This type of therapy is particularly used in edentulous jaws 10,12.
Among the implant-supported options, the prosthesis following the Brånemark protocol has good longevity 6 and clinical efficacy. This prosthesis is characterized by the placement of four to six implants in the anterior mandible, among mental foramen, with distal cantilever on both sides to replace the posterior teeth. Also, the prosthesis is composed by metallic infrastructure and resin base to bond to the acrylic resin teeth 1.
To perform the rehabilitation with the highest quality, the dentist should know all clinical steps, as well as the analysis of the details of each case. This case describes the association of a maxillary total denture with a mandibular implant-supported fixed denture following Brånemark protocol type, and discusses the case characteristics affecting the technical steps.
Case report
A male patient, aged 62 years, melanoderm, with no contributory disease, searched the Dental Prosthesis Clinics of the State University of Maringa, for prosthetic treatment.
At clinical and radiographic examinations, the patient exhibited an edentulous maxillary arch, with consistent alveolar ridge, within the normal range; he has been using the same total denture for 23 years, which was poorly adapted and had severe tooth wear. The patient complained about the function and esthetics. In the mandible, the patient no longer wore prosthesis for several years due to low stability. Five implants Tissue Level (TL) (Straumann®, São Paulo, SP, Brazil) Ø 4,1 mm, length of 10 mm, Regular Neck (RN), Slactive surface, with prosthetic platform of 4.8 mm were installed 90 days ago in the specialization course in periodontics. The patient's file showed that all implants had excellent primary stability with insertion torque above 35 Ncm, also with uneventful post-operative occurrences. After surgery, the patient was absent from the city because of his work for three months, after which he returned and sought care. The implants had no pockets, bleeding to probing, degree of mobility or significant bone loss observed on radiographs (figures 1 and 2).

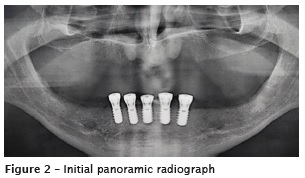
The patient sought a stable, functional, and aesthetically pleasing prosthetic rehabilitation. Thus, the proposed treatment planning included a new maxillary total denture and mandibular implantsupported fixed total denture following Brånemark protocol on the five implants. After the explanation of the advantages and disadvantages of this therapy and signature of consent form, an impression of the current maxillary dentures and mandibular implants was carried out, followed by the registering of the maxillo-mandibular relationship, the facial bow, and mounting in semi adjustable articulator, along with the kit selection of TL components (Straumann®, São Paulo, SP, Brazil), to optimize the choice for the prosthetic components. Seeking a position favoring an aesthetic solution for the screws and a single passive insertion axis, five abutments SynOcta (Straumann®, São Paulo, SP, Brazil), regular neck, height 1.5 mm were selected.
Defined the components, the work impression was executed with molding hoods bolted with integrated guide screw (Straumann®, São Paulo, SP, Brazil), with height of 21 mm. After that, the hoods were united with self-curing low shrinkage polymethylmethacrylate (Pattern Resin®, GC, Tokyo); elapsed 15 minutes for maximum releasing of contraction forces, and already out of the mouth, the structure was sectioned into five blocks with the use of a thin cutting disc. Then, again screwed to implants, the blocks were joined with the same polymethylmethacrylate; elapsed more 15 minutes, with a previously customized tray, a new impression was taken with the aid of light and heavy addition silicone (Elite®, Zhermack, Italy) through doublemixture technique, following the manufacturer's instructions. After polymerization, the screw guide of the hoods were withdrew and the whole set was removed; assured the a good reproduction of the RN implant analogs (Straumann®, São Paulo, SP, Brazil), length of 12 mm de, Ø 4,8 mm, were inserted into the impression. After 1 hour, the artificial gingiva was applied (Gingifast®, Zhermack, Italy) around the analogs followed by its polymerization. The dental cast was obtained with type VI plaster (Durone®, Dentsply, DE, USA), following the manufacturer1s instructions (figures 3 and 4).

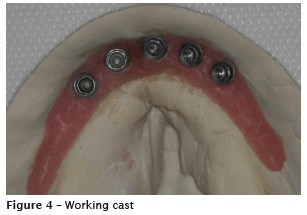
As an additional measure, a template of the impression was made through the use of impression hoods screwed to the implants. Unlike the impression procedure, after the polymethylmethacrylate polymerization time, there was no use of any impression material. The assembly was removed, the analogs were screwed and positioned in a container with type VI plaster (figures 5 and 6).


In the maxilla, an impression a with alginate (Cavex®, Haarlem, DV, Netherlands), casted in type III plaster (Asfer®, São Paulo, SP, Brazil), to construct a customized tray; followed by the functional impression with the aid of low fusion Godiva (Godibar®, São Paulo, SP, Brazil), for peripheral sealing, and zinc-enolic paste (Lysanda®, São Paulo, SP, Brasil), with the following pouring with type VI plaster.
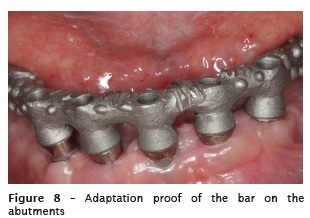
In the next step, the proof of the chrome-cobalt metallic bar took place. Following, the abutments SynOcta were screwed on the implants, the bar was inserted passively at single axis and its perfect match was found through visual inspection, probing of interfaces with the aid of a sharp explorer, and bitewing radiographs (figures 7 and 8).

At the same appointment, the ma xi l lomandibular relationship was recorded, establishing a new vertical dimension of occlusion (VDO), lip support, buccal corridor, occlusal plane, high smile lines, medium and labial commissures, color selection and size of the teeth. Throughout this stage the patient actively participated, expressing their desires and aesthetic considerations (figure 9).

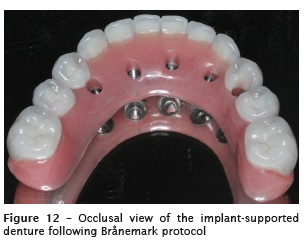
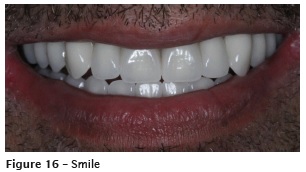
The selected teeth were Chroma-4 A1/ED6 (NOVA DFL®, São Paulo, SP, Brazil). The waxed teeth were proved, and the Class I occlusion, protrusive and canine guides, bilateral and simultaneous subsequent contacts, alignment, exposure to smile, shape, and color were verified, with the approval by the patient and subsequent acrylization (figure 10).

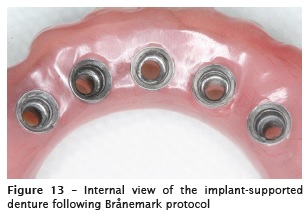
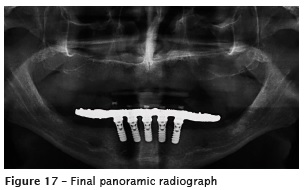
At the prosthesis del ivery appointment abutments SynOcta 1.5 mm were placed on the implants and tightened to a torque of 35 Ncm. The mandibular fixed prosthesis was installed, verifying the adaptation to the implants and the good relationship with mandibular ridge, checking for access to interdental brushes; at that time, the patient received detailed instructions to perform oral hygiene. Then, the screw holes were closed with the aid of polytetrafluoroethylene tape (Tigre S/A®, Joinville, SC, Brazil) and light-cured composite resin (Brilliant New Line®, Rio de Janeiro, RJ, Brazil). The maxillary denture was adjusted regarding adaptation and extension. The patient was very satisfied with the aesthetic and functional outcomes (figures 11 - 17).



Discussion
Fixed implant-supported dentures are the most desired ones among edentulous patients, because they promote greater masticatory efficacy and comfort, less maintenance, and eliminate the removable aspect of other modalities such as conventional dentures or overdentures, adding positive psychological factors. However, the technique is difficult, more expensive, and requires more care and attention to daily hygiene processes 13. All these factors were discussed with the patient and, in addition to their understanding, we did not find the existence of any cognitive or physical disability that could prevent or hinder the correct cleaning of the prosthesis.
The protocol type prostheses show good indication because of some conditions such as occlusal compatibility in cases where the patient uses antagonist denture, low cost compared to metallic-ceramic, good functionality, and they can be indicated for most of mandibular cases 16.
The proper planning of all stages of this prosthesis is critical to a successful outcome. In our case, there was some difference of inclination between implants, which could suggest the use of angled components. However, during the component selection step, it was found that the use of angled abutments of this system, even short, would create different axes of insertion, which would hinder the passive fit of the bar. With the straight abutments, the vertical area of the components was smaller, facilitating the insertion of the bar. Passivity is extremely important, because a structure without passivity can lead to loss of osseointegration 8,9.
In the open or work impression, direct transfer of components was used, which during the impression removal from the tray will stay in the impression. They allow the union to each other with resin. After polymerized, they are separated with discs and again linked directly in the mouth, a fact that reduces the amount of acrylic and polymerization shrinkage and its interference with the position of the implants 2. In addition to conventional work impression, a template was confectioned with the hoods attached without the potential interference of the impression material over the conventional impression materials. This measure provides a counter proof of the impression and enable a more detailed analysis of the bar settlement and adjustments still in the laboratory, saving clinical time.
The wax bases were made to allow the recording of the maxillo-mandibular relationship. The determination of the vertical dimension of occlusion (VDO) is established following the patterns of facial anthropometry 15. In this case report, the VDO reestablishment was fundamental to the esthetic and functional modifications requested; as he did not use any prosthesis on the mandible, the lower third of the face was shorter, consequently the patient had a frequent injury on labial commissures due to saliva accumulation and wounds in the region.
It was not necessary to cut the metallic infrastructure because the adaptation had been tested both on the working cast and on the template and the necessary corrections already made in the laboratory. The bar design itself compensated the different inclinations of the implants, searching to maintain a uniformity in the resin thickness that would be applied, and maintaining additional retention for better retention with it. Technically, it is recommended for the mandible that the cantilever length does not exceed 18 to 20 mm 11; the cantilever of this case report had 18 mm on the right and 19.5 mm on the left side.
At the proof of the teeth step, it is essential to examine the labial/buccal and lingual contours of the prosthesis, so that there is interference in the movements of the lips and tongue during speech and swallowing 4,15. All the aesthetic, phonetic, and functional proofs and the acceptance by the patient should be analyzed 15.
The bottom surface of the protocol type prosthesis was also covered by resin including the metallic structure, because once this area is involved by the resin, the resin weariness or addition, if necessary, are more simply and quickly made.
At the moment of prosthesis delivery, during installation, the screws are adjusted sequentially so that the prosthesis has passive fitting, a radiograph is taken to evaluate the bone level of each implant and the adjustment of the components 4. After that, it is needed to confirm the existence of adequate space for cleaning, followed by a correct training and implementation of hygiene measures to ensure good soft tissue health at the long term 3,6,7.
Conclusion
The prosthesis Brånemark protocol is a viable and effective alternative in edentulous patients, providing stability to the prosthesis, masticatory efficiency, and aesthetic. The analysis and planning of each case are necessary to treatment success.
References
1. Adell R, Lekholm U, Rockler B, Brånemark P-I. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10(6):387-416. [ Links ]
2. Arita CA. Prótese sobre implantes no segmento posterior. Implant News. 2006;3(4):336-43.
3. Balshi TJ, Wolfinger GJ, Slauch RW, Balshi SF. A retrospective analysis of 800 Brånemark system implants following the All-on-Four™ protocol. J Prosthodont. 2014;23(2):83-8.
4. Darcymar MR, Zardo CM, Souza Neto J. Odontologia estética e a prótese fixa dentogengival. São Paulo: Artes Médicas; 2003.
5. Dinato JC, Nunes LS. Tratamento protético sobre implante no desdentado total na atualidade. Implant News. 2006;3(5):452-67.
6. Ferrigno N, Lauretti M, Fanalli S, Grippaudo G. A long-term follow-up study of nonsubmerged ITIimplants in the treatment of totally edentulous jaws. Part I: ten-year life table analysis of a prospective multicenter study with 1.286 implants. Clin Oral Implants Res. 2002;13(3):260-73.
7. Friberg B, Jemt T. Rehabilitation of edentulous mandibles by means of osseointegrated implants: a 5-year follow-up study on one or two-stage surgery, number of implants, implant surfaces, and age at surgery. Clin Implant Dent Relat Res. 2015;17(3):413-24.
8. Greco GD, Jansen WC, Landre JJ, Seraidarian PI. Biomechanical analysis of the stresses generated by different disocclusion patterns in an implantsupported mandibular complete denture. J Appl Oral Sci. 2009;17(5):515-20.
9. Guichet DL, Caputo AA, Choi H, Sorensen JA. Passivity of fit marginal opening in screw - or cement - retained implants fixed partial denture designs. Int J Maxillo Fac Implants. 2000;15(2):239-46.
10. Lindquist LW, Carlsson GE, Glantz PO. Rehabilitaion of the edentulous mandible with a tissue-integrated fixed prosthesis: a sixyear longitudinal study. Quintessence Int. 1987;18(2):89-96.
11. Lindquist LW, Rockler B, Carlson GE. Bone resorption around fixtures in edentulous patients treated with mandibular fixed tissue-integrated prostheses. J Prosthet Dent. 1988;59(1):59-63.
12. Minoretti R, Triaca A, Saulacic N. Unconventional implants for distal cantilever fixed full-arch prostheses: a long-term evaluation of four cases. Int J Periodontics Restorative Dent. 2012;32(2): 59-67.
13. Misch CE. Prótese sobre implantes. São Paulo: Santos; 2007. p. 252-64.
14. Rasmusson L, Roos J, Bystedt H. A 10- year follow-up study of titanium dioxide-blasted implants. Clinical Implant Dentistry and Related Research. 2005;7(1):36-42.
15. Telles D, Coelho AB, Lourenço EV. Próteses fixas sobre implantes. São Paulo; 2014.
16. Telles D, Hollweg H, Castellucci L. Prótese total convencional e sobre implantes. São Paulo: Santos; 2003.
 Corresponding author:
Corresponding author:
Rodrigo Lorenzi Poluha
Departamento de Odontologia – Universidade Estadual de Maringá
Avenida Mandacaru, 1.550 – Vila Santa Izabel
CEP 87080-000 – Maringá – Paraná – Brasil
E-mail: rodrigopoluha@gmail.com
Received for publication: June 29, 2015
Accepted for publication: August 4, 2015













