Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.12 no.4 Joinville Out./Dez. 2015
CASE REPORT ARTICLE
Reestablishing aesthetic and function of patient with severe worn dentition: a conservative approach with provisional fixed tooth/implant supported prosthesis
Guilherme Gonçalves AndreattaI; Fernanda Durski TeixeiraI; Leonardo Fernandes CunhaI;Adilson Yoshio FuruseII; Gisele Maria Correr NolascoI; Carlos Eduardo E. RezendeI
I Department of Dentistry, Positivo University – Curitiba – PR – Brazil
II Department of Operative Dentistry, Endodontics and Dental Materials, Bauru School of Dentistry, University of São Paulo – Bauru – SP – Brazil
ABSTRACT
Introduction:Patients with severe parafunctional habits can have a reduction of their occlusal vertical dimension (OVD) and may create complex cases of oral rehabilitation, in which the patient may develop occlusal, masticatory and psychological problems. Objective: To report a clinical case of restoration of masticatory function and aesthetics from the production of tooth/implant-supported prostheses with conservative preparations, reestablishing the OVD and occlusal stability.Case report: Patient MVN, 55 years old, wheelchair user, presenting bruxism with a history of gastric reflux due to hiatal hernia, attended the clinic at the University complaining of dental sensitivity, difficulty in chewing and aesthetic smile commitment. At clinical examination it was found widespread wear of teeth. Radiographic examination showed good periodontal health and dental implants in good condition of osseointegration. The OVD was established from the VDR and confirmed by the metric method. The initial casts were positioned on the articulator for diagnostic waxing. From the waxing it was possible to make provisional fixed tooth/implant-supported prostheses. In the lower arch, the prosthesis was screwed on the implants #35, #37, #46, and #47, with the remaining teeth working as an auxiliary support, while in the upper arch two interim prosthesis were made, one for the elements #16 and #17 (tooth-supported) and one for the elements #13, #12, #11, #21, #22, #23, #24 (tooth/implant-supported). Thus, the OVD and the aesthetics lost by bruxism abrasion were restored. Conclusion:This case demonstrates the importance of the provisional prostheses for aesthetic and functional rehabilitation of patients with severe worn dentition.
Keywords: bruxism; dental implant; dental prosthesis; implantsupported.
Introduction
Of ten dent ists are faced with cases of oral rehabilitation in which the function and aesthetics need to be restored. Patients with trauma, temporomandibular disorders, periodontal disease, multiple large cavities untreated, and parafunctional habits with deleterious effects may have compromised the harmony of the stomatognathic system 2.
Patients with parafunction might have wear of tooth surface, leading to consequences in the stomatognathic system. The parafunction most commonly found in dental clinics is bruxism, which is characterized by clenching or grinding of teeth as a consequence of repetitive jaw-muscle activity 7. These patients might suffer of general worn dentition and alveolar bone resorption 9. In such cases, the use of an occlusal device is indicated for relieving the stress on the teeth, which predominantly occur involuntarily during sleep 8. The severe wear of teeth can lead to a pulp irritation. In addition, bruxism consequences may involve headaches and facial pain, tooth sensitivity and aesthetic impairment of smile 14.
The teeth wear can lead to a decrease in occlusal vertical dimension (OVD), reducing the space between the arches and maintaining and keeping the muscles strained, causing loss of balance in the distribution of occlusal forces and further intensifying the wear on teeth 4. The loss of vertical dimension of occlusion caused by physiological tooth wear does not occur when compensated for by continuous tooth eruption, in conjunction with the alveolar bone remodeling 17. When teeth wear rate exceeds the compensatory mechanisms, a loss of vertical dimension of occlusion is observed 11,17.
The wear of tooth surfaces can be aggravated by the erosive action of acids in the oral environment. It is common for such a situation arises in patients with gastroesophageal ref lux disease (GERD). Such erosive action of GERD associated with the abrasive action of bruxism can lead to rapid loss of tooth structure, causing functional and aesthetic impairment of the patient's dentition 1.
The rehabilitation of patients with severe tooth wear and loss of OVD consists in the restoration of adequate space between the arches, the reconstruction of the anatomy of the teeth and the readjustment of the occlusal stability of the patient 9. These objectives should be achieved already at the stage of interim prosthesis, in which the patient will get used to the new vertical dimension and occlusal condition restored 10. At this stage, it is important to wait 40 days from the restoration of OVD in order to prepare the stomatognathic system for the final rehabilitation treatment 5.
For patients with worn dentition the amount of tooth tissue should be considered, in seeking to evaluate the necessity of cores and preparations, allowing for the better treatment planning. However, because this is a complex and costly treatment, it is important to take into account the best cost/ benefit for the patient and, when possible, aim at conservative maneuvers 12.
The aim of this study is to report a case of restoration of masticatory function and aesthetics from the production of tooth/implant-supported prosthesis with conservative preparations in order to return the OVD and the occlusal stability.
Case report
Patient MVN, male, 55 year-old, presented to the dental clinic of the University complaining of severe teeth wear, difficulty to chew, esthetical impairment and thermal tooth sensitivity (Figure 1). The patient also expressed a desire to put prosthetics on implants that had been installed for more than 18 months ago. However, he expressed financial concerns. At the anamnesis, the patient reported being wheelchair user due to automotive accidents and to have a history of hiatal hernia. Furthermore, it was found that the patient had bruxism.
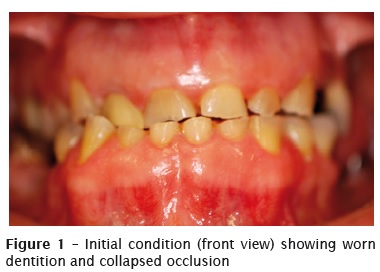
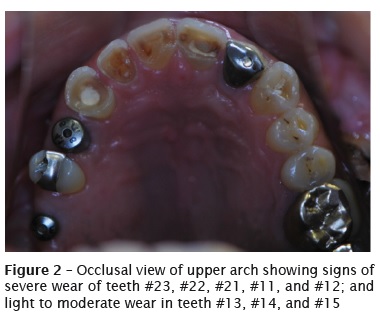
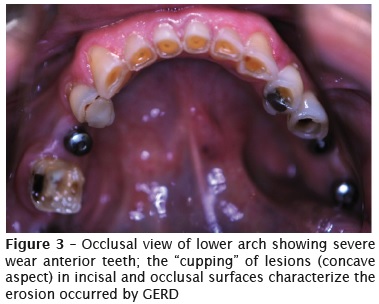
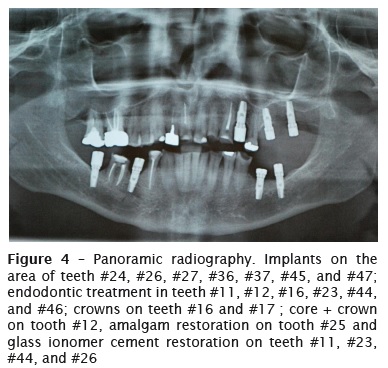
At intraoral examination, it was observed in the maxillary arch: the absence of third molars; teeth #16 and #17 with metal-ceramic crowns and unsatisfactory endodontic treatment; teeth #13, #14 and #15 with moderate wear; tooth #12 with core and crown; teeth #11, #21, and #22 with severe wear, and tooth #11 with endodontic treatment; tooth #23 with endodontic treatment and moderate wear; osseointegrated dental implants on the area of teeth #24, #26, and #27; tooth #25 with satisfactory MO amalgam restoration (Figure 2). In the lower arch: osseointegrated implants on area of teeth #36, #37, #45, and #47; teeth #35-#43 all with severe wear and pulp vitality; tooth #44 with moderate wear, endodontic treatment and temporary restoration in restorative glass ionomer; tooth #46 with sharp coronal wear and endodontic treatment (Figure 3).
After the clinical examination it was found that all implants had external hexagon joint and regular platform (Ø4.1 mm), duly osseointegrated and exposed to the oral environment through the use of healing abutments. The wear of tooth surfaces in concave appearance, demonstrated the erosive process, resulting from GERD, in the process of loss of tooth structure 1. The parafunctional habits (bruxism) without the use of occlusal devices was appointed as the main reason for the severe wear of the teeth.
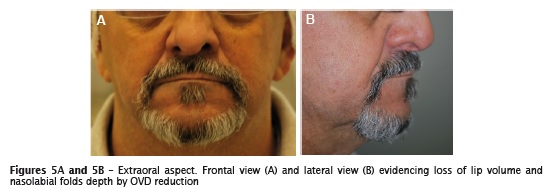
A panoramic radiograph was requested to complement diagnosis. Thus, it was possible to analyze the bone insertion of teeth and implants as well as the quality of endodontic and restorative treatments (Figure 4). At the extraoral examination, a loss of occlusal vertical dimension was found, being confirmed by the deepening of the nasolabial folds and reduced volume of lips (Figures 5A and 5B).
Restorative procedures
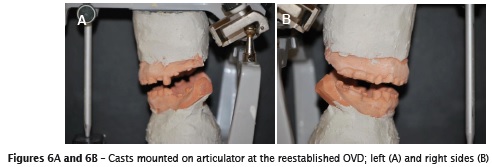
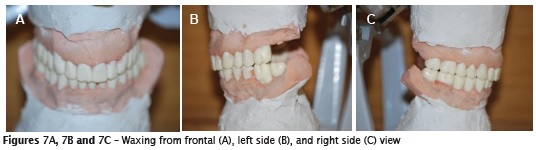
It was first established the new OVD from the vertical dimension at rest (VDR) using the Willis compass, reducing 3mm from VDR. Then, the OVD obtained was confirmed by the method of the facial proportions. Alginate impressions (Cavex, Fustweg; Netherlands) were carried out to obtain study models of the upper and lower arches. The facial bow was set up to assist the correct positioning of the models in the semi-adjustable articulator (SAA) and an occlusal registration was held with dense silicone, at OVD, measured by manipulating the patient in centric relation (CR) by Dawson's bimanual technique. The articulator with mounted models (Figures 6A and 6B) was referred to the dental laboratory for the waxing of the teeth #16-#27, and #47-#37 (Figures 7A, 7B and 7C).
After waxing, the removal of metallic ceramic crowns was done for the teeth #16, #17, and #12 and a re-preparation was done for metal-ceramic crown with a chamfer finish line. Teeth #11 and #21 received conservative preparations with a reduction of 0.5 mm on the buccal and incisal surfaces to facilitate the accommodation of the restorative material. The remaining upper arch teeth were not prepared. The implant corresponding to the tooth #24 received an UCLA titanium abutment (UCLA HE titanium; Neodent; Curitiba-PR; Brazil), which was prepared for a cemented prosthesis.
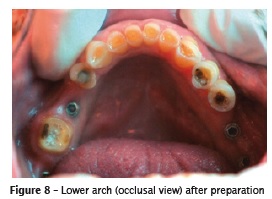
In the lower arch, the tooth #36 was prepared for a metal-ceramic crown and tooth #35 tooth was prepared for an onlay ceramic crown. In the remaining teeth, just a plasty for regularization of the edges were made on the occlusal/incisal surfaces worn by parafunctional habit (Figure 8).
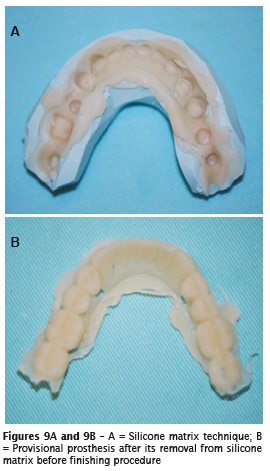
The upper and lower waxing was then copied with a condensation silicone (Speedex; Coltène; Rio de Janeiro, Brazil) to perform provisional fixed prostheses by the silicone matrix technique. The acrylic resin (Dencor, Campo Limpo Paulista - SP, Brazil) was mixed at the ratio indicated by the manufacturer and inserted in the silicone matrix at the sandy phase stage. After the loss of brightness of the resin and the set of the silicone matrix and the acrylic resin, they were taken off the patient's mouth (Figures 9A and 9B). This step was performed with the healing abutments in position to mark the placement of implants in the prosthesis. The excess was removed with tungsten cutters (maxicut and minicut), as well as serrated discs for removal of excess in the proximal regions.
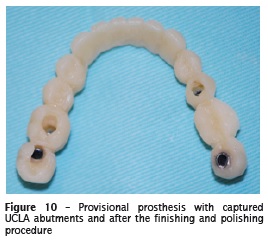
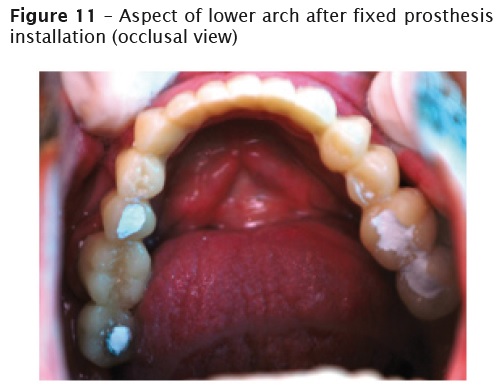
In the case of the lower arch, a round steel bur (size No. 10) for handpiece was used for the opening of holes corresponding to the implant abutments in the prosthesis and four titanium UCLA abutments with anti-rotational device (UCLA HE titanium; Neodent; Curitiba-PR) were installed on the implants and cut at the occlusal plane level. Then, the UCLA abutments were captured, using the bead-brush technique to bond them to the prosthesis. Thus, the result for the lower arch was a single piece implant-retained fixed prosthesis, screwed onto the implants (37, 36, 45 and 47) and only supported by the remaining teeth (Figure 10). The finishing and polishing process was performed with rubber and abrasive polishing paste with felt disc and Robinson brush (Figure 11). Spaces were left in the gingival aspect to allow cleaning by the patient.
In seeking to seal the teeth/prosthesis interface, it was used glass ionomer cement (GIC) (Vidrion C, SS White, Rio de Janeiro - RJ, Brazil) to avoid marginal leakage and reduce sensitivity of worn teeth. This material was chose due to its capability to release fluoride.
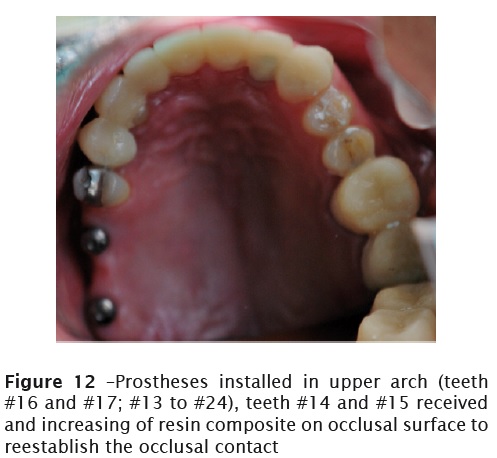
In the upper arch, two provisional prostheses were constructed, one joining the teeth #16 and #17, and the other extending from the teeth #13 to #24, cemented over the prepared tooth #12 and the prepared titanium abutment on the implant of tooth #24; and just leaning on teeth #13, #11, #21, #22, and #23 with GIC liner used for sealing the interface between them and the provisional prosthesis (Figure 12). The finishing and polishing procedures were performed in the same manner described for the lower arch.
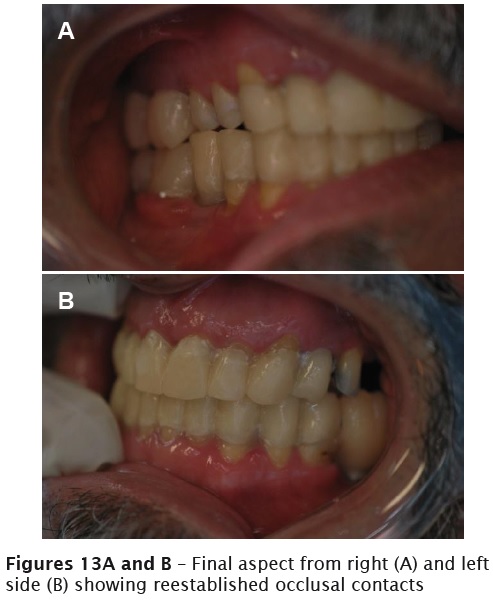
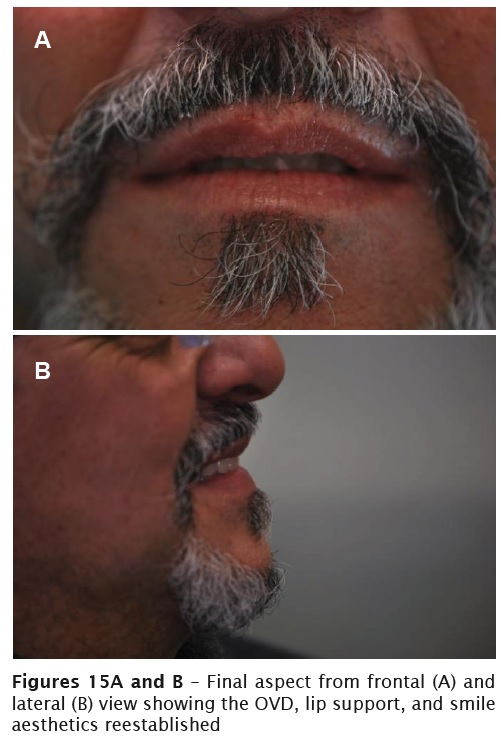
The hygiene instruction was performed after the provisional prostheses installation. After 15 and 30 days, maintenance was done to evaluate the occlusal condition and hygiene. Temporary occlusal acetate splint (BIOART, San Carlos - SP, Brazil) was constructed for the upper arch, aiming at the protection of the prosthetic work and avoid the deleterious effects of bruxism. Figures 13A, 13B, 14, 15A and 15B shows the provisional prostheses finished installed on patient's mouth.

Discussion
This paper reports the case of a male patient, partially edentulous, with worn dentition generating an OVD loss. Among the options of treatment available for this situation there is: Overlay removable prosthesis, which re-establishes the function and aesthetics as well as being relatively simple, fast and affordable 6,13,18. However, implant-supported dentures can promote an increase of 60 to 200 times in the masticatory muscle activity 16. The tooth/implant-supported fixtures presents the advantage of not being removed from the mouth, since this act causes a slight wear of the teeth over time, causing a loss in stability of the removable prosthesis 15, which may already have poor retention and stability due to short abutment crowns and therefore with smaller retentive area due to teeth wear 1. In addition, the chewing function is directly related to the neuromuscular action, especially the masseter and temporal muscles, and the force of muscles contraction is lower in PPR wearers when compared to fixed prostheses users 3. Faced with such evidence, in this case report the construction of a fixed prosthesis was preferred, seeking greater chewing efficiency and comfort for the patient.
Therefore, in this study, it was decided to make the provisional PFP with acrylic resin, supported by implant and tooth, being screwed to the implants in the lower and cemented in the upper arch. For the lower arch the prosthesis was screwed on implants (#46, #47, #35, and #37), rebuilding the worn structure of the remaining teeth with acrylic resin, joining the entire arch. In the maxilla were made two prostheses in acrylic resin, one for teeth #17 and #16 (together), other for the teeth #13-#24 (attached), and a small recovery in the teeth #14 and #15 with composite resin for occlusal contact restoration. So, the option for a better comfort and masticatory efficiency, as well as a less costly treatment, was made.
In cases of severe wear associated to erosion by GERD, the treatment should be as conservative as possible, taking advantage of the advances in the use of fluoride, the adhesive dentistry, and biomimetic materials 1. Remember that conservative preparations were carried out in order to avoid irreversible wear of the teeth, which would limit the final rehabilitation treatment options. The way tooth preparations were made in this study, allows the use of various treatment modalities, such as reconstruction of teeth with composite resin, partial crowns, total crowns, and removable prosthesis. Thus, upon the final rehabilitative treatment, we can discuss with the patient the treatment alternative with better cost-benefit ratio to him.
There is no consensus on the treatment protocol for cases of severe worn dentition. However, available evidence advises the use of diagnostic waxing and the determination of CR as occlusal position for rehabilitation 9,10. In addition, the restoration of OVD at the interim stage before the final treatment is recommended 10. Such procedures were followed in this study. Regarding the final treatment, both resin composites as ceramics, could be considered for the final rehabilitation, since the indication of an occlusal device (occlusal splint) and the regular monitoring of patient is performed 10.
Knowing the etiology of severe worn dentition is critical for correct treatment plan. Furthermore, an early diagnosis can prevent the need for more complex rehabilitation treatments. Dentists may be the first health professionals to diagnose GERD because of its oral manifestations.
In the present study, the data from the anamnesis and the clinical experience were essential to determine the treatment plan, allowing for the indication of the material and technique with better cost/benefit for the case. Cases of oral rehabilitation associated with the restoration of the OVD are complex and require professional extensive knowledge, from diagnosis to the indication and execution of the treatment technique. Worn dentition by bruxism and/or GERD should involve multidisciplinary team, creating conditions to reach the harmony between function and aesthetics, making the treatment to last.
Conclusion
The use of provisional tooth/implant supported prosthesis for the rehabilitation of severely worn dentition proved to be feasible, by enabling the restoration of function and aesthetics, from conservative preparations and thus providing a good cost/benefit relation.
References
1. Barron RP, Carmichael RP, Marcon MA, Sàndor GKB. Dental erosion in gastroesophageal reflux disease. J Can Dent Assoc. 2003 Feb;69(2):84-9. [ Links ]
2. Behsnilian V. Oclusion y rehabilitation. 2 ed. Montevideo: Papelera; 1974. p.68-100.
3. Dakhilalian M, Rismanchian M, Fazel A, Basiri K, Azadeh H, Mahmoodi M et al. Conventional versus implant-retained overlay dentures: a pilot study of masseter and anterior temporalis electromyography. J Oral Implantol. 2014 Aug;40(4):418-24.
4. Dantas EM. A importância do restabelecimento da dimensão vertical de oclusão na reabilitação protética. Odonto 2012;20(40):41-8.
5. Dekon SFC, Pellizzer EP, Zavanelli AC, Ito L, Resende CA. Reabilitação oral em paciente portador de parafunção severa. Rev Odontol Araç. 2003 Jan/Jul;24(1):54-9.
6. Freitas R. Diagnóstico e tratamento da dimensão vertical de oclusão diminuída. RGO. 2006 Apr/ Jun;54(2):161-4.
7. Lobbezoo F, Ahlberg J, Glaros AG, Kato T, Koyano K, Lavigne GJ et al. Bruxism defined and graded: an international consensus. J Oral Rehabil. 2013;40:2-4.
8. Marques JLS, Fernandes CMO, Cardoso PC, Torres EM, Rocha S. Reabilitação estética-funcional com ajuste prévio da oclusão em relação cêntrica. Rev Odontol Bras Central. 2010;19(51):356-61.
9. Moshaverinia A, Kar K, Aalam AA, Takanashi K, Kim JW, Chee WW. A multidisciplinary approach for the rehabilitation of a patient with an excessively worn dentition: a clinical report. J Prosthet Dent. 2014 Apr;111(4):259-63.
10. Muts EJ, van Pelt H, Edelhoff D, Krejci I, Cune M. Tooth wear: a systematic review of treatment options. J Prosthet Dent. 2014 Oct;112(4): 752-9.
11. Phuhong DD, Goldstein GR. The use of a diagnostic matrix in the management of the severely worn occlusion. J Prosthodont. 2007 Jul- Aug;16(4):277-81.
12. Soares CJ, Pizi EC, Fonseca RB, Martins LR, Fernandes AJ Neto. Direct restoration of worn maxillary anterior teeth with a combination of composite resin materials: a case report. J Esthet Restor Dent. 2005;17(2):85-91.
13. Souza JEA, Silva ET, Leles CR. Prótese parcial removível overlay: fundamentos clínicos e relatos de casos. Robrac. 2009;18(47):41-8.
14. Turner KA, Missirilian DM. Restoration of the extremely worn dentition. J Prosthet Dent. 1984 Oct;52(4):467-74.
15. Van der Bilt A, van Kampen FM, Cune MS. Masticatory function with mandibular implant-supported overdentures fitted with different attachment types. Eur J Oral Sci. 2006; Jun;114(3):191-6.
16. Van Kampen FM, van der Bilt A, Cune MS, Bosman F. The influence of various attachment types in mandibular implant-retained overdentures on maximum bite force and EMG. J Dent Res. 2002 Mar;81(3):170-3.
17. van't Spijker A, Kreulen CM, Creugers NH. Attrition, occlusion, (dys)function, and intervention: a systematic review. Clin Oral Implants Res. 2007 Jun;18(Suppl 3):117-26.
18. Windchy AM, Morris JC. An alternative treatment with the overlay removable partial denture: a clinical report. J Prosthet Dent. 1998 Mar;79(3):249-53.
 Corresponding author:
Corresponding author:
Carlos Eduardo E. Rezende
Rua Prof. Pedro Viriato Parigot de Souza, n. 5.300 – Campo Comprido
CEP 81280-330 – Curitiba – PR – Brasil
E-mail: carlosrezende@up.edu.br
Received for publication: August 14, 2015
Accepted for publication: September 29, 2015













