Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.12 no.4 Joinville Out./Dez. 2015
CASE REPORT ARTICLE
Dental treatment of a child with oral cleft: a case report
Iara Aparecida Zanon AndradeI; Sheila de Carvalho StroppaI; Juliana Yassue Barbosa da SilvaI
I Department of Dentistry, Positivo University - Curitiba - PR – Brazil
ABSTRACT
Introduction:The cleft lip and palate are the most common facial congenital malformations, developing in the early embryonic stages between the fourth and eighth week of intrauterine life. Objective: To present the dental treatment of a child with cleft lip and palate under general anesthesia. Case report: Patient, aged four years, with cleft lip and palate, living in an indigenous village in the city of Vilhena, Rondônia, Brazil, with poor hygienic conditions and with dental caries, needed dental treatment under general anesthesia. The clinical examination revealed that the child had impaired general health by the presence of several wounds in the feet and nails, low weight, and many carious lesions. Discussion: In addition to parents' instructions and monitoring of multidisciplinary team, it is important to know the life of the patients with oral cleft, to target the most appropriate treatment to be successful in their rehabilitation process. Conclusion:Children with cleft lip and palate can have their quality of life improved through adequate care.
Keywords: cleft lip and palate; child; oral health.
Introduction
Cleft lip and palate have accompanied the existence of mankind, and are the most common facial congenital malformations 13. The cleft lip and palate develops in the first embryonic stages, which comprise the period from fourth to eighth week of intrauterine life, originating in the branchial or pharyngeal arches and its derivatives 1,4,9,11.
Several studies were conducted in order to increase knowledge of the etiology of oral clefts. Knowledge of etiologic factors, prevalence and variable expression of the genetic factor and defects related to it can help in the clinical treatment and patient's approach, and contributes to a better understanding of the etiology and pathogenesis 10,15.
As for racial pattern, cleft lip and palate can affect all racial and ethnic groups, irrespective of gender or economic class 7. The most accepted cleft and lip and palate classification was established by Spina et al., in 1972 4. This classification covers the morphological and embryological malformation, regarding to the incisive foramen. The classification is divided into groups:
1) Pre-incisive foramen cleft: only affects the lip, with or without involvement of the alveolar ridge and nose wing. Bilateral or unilateral, complete or incomplete.
2) Trans-incisive foramen cleft: more complex type, affecting lip, alveolar ridge, and all palate. Bilateral or unilateral, complete or incomplete.
3) Post-incisive foramen: the cleft palate, generally median, which can be located only in the uvula, palate, and involve all the hard palate. Bilateral or unilateral, complete or incomplete.
4) Rare facial clefts.
The cleft lip and palate can be corrected and should not prevent the individual from living a normal life. However, since birth, children with oral clefts have difficult to feed due to: insufficient intake, weak suction, nasal escape, excessive swallowing of air, abundant vomiting, choking and suffocation 5.
In general, cleft lip and palate compromise the aesthetics and much of orofacial functions, which implies in the need for a multidisciplinary team to establish the basis for a rehabilitation treatment through specific protocols for each case 15. According to the American Cleft Palate Association (ACPA) and the European Association for Cleft Palate (Eurocleft), the multidisciplinary team should be minimally composed by plastic surgeons, psychologists, dentists, audiologists, and otolaryngologists 2.
This study aims to report a clinical case of dental treatment under general anesthesia of a child aged 4 years with cleft lip and palate, living in an indigenous village, in the city of Vilhena, Rondônia, Brazil.
Case report
Patient N.N., male, with non-syndromic bilateral trans-incisive foramen cleft, born in an indigenous village, in the city of Vilhena, Rondônia, Brazil. The child lived with his parents and sister in a place without basic sanitation without treated water (water withdrawal from well) and no electricity. The family was treated at the Basic Health Unit in the city. The child's food was basically made up of vegetables, chicken and fish; he did not like to eat fruit, but frequently eats breads and cakes.
The mother was an artisan and the father was a farmer. The reported family income was from zero to half minimum wage, plus the benefit of social program Bolsa Familia.
NN was the second son and the mother reported to have prenatal care since the first quarter, which proved to have access to the health service. The child was born by normal delivery with 3,010 k g, with height of 48 cm and Apgar 10 at 1 minute and 5 minutes which were signs very characteristics of a healthy child.
The first appointment at the Center for Integral Treatment to the Individual with Cleft lip and palate (CAIF), in Curitiba (PR) was at two months of age, through referral by a primary care unit of Vilhena. At the time, the child and his parents went through appointments with pediatrician, plastic surgeon, genetics, social worker, speech therapist, psychologist, and dentist. Also, the extraction of a neonatal tooth located at premaxilla was performed. The child already used artificial milk, showing that breastfeeding was not possible. Although the parents do not speak properly and understand Portuguese, they understood that there is a familial genetic component in the etiology of cleft lip and cleft, since the mother and a maternal uncle also have cleft lip and palate.
At four months old, in August of 2010, the general health status of the child was satisfactory and the first lip repair (reconstructive surgery of the upper lip) was realized. Sometime after surgery, but unrelated to this, the child had anemia and began using ferrous sulfate until the beginning of 2011. In July of 2011, a new lip repair was carried out.
The child only returned to CAIF in 2013, two years later, when the plastic surgeon made the the oral hygiene conditions, biofilm presence, and active caries that contraindicated the palatoplasty (surgical reconstruction of the palate, generally performed at 18 months of age). Dental evaluation was performed, and because of non-cooperation, the complexity of procedures, the number of carious lesions, the child does not understand Portuguese, which made psychological management, treatment planning comprised dental treatment under general anesthesia.
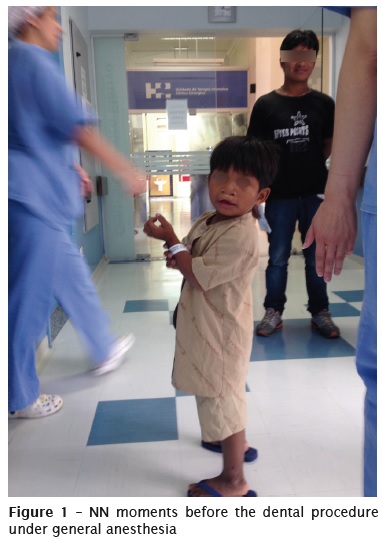
In November, 2014 the dental treatment under general anesthesia was scheduled. At that moment, NN aged 4 years and 7 months. weighed 15 kg (Figures 1 and 2), and was frequently consuming sugar-rich foods (breads and cakes) The father reported that oral hygiene is made by the child only once a day, using children's toothbrush and f luoride toothpaste, and showed no interest in learning how to control and improve the child's oral hygiene and nutritional situation.

Oral condition
Large amounts of biofilm and extrinsic stains from the use of ferrous sulphate were present on several teeth. The child had 16 primary teeth, all showing carious lesions (Figure 3).

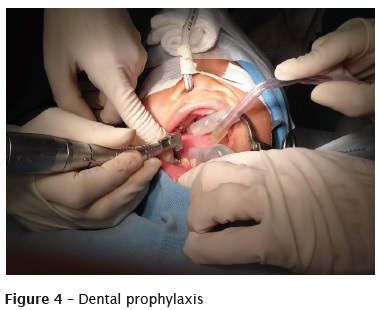
Dental treatment started after general anesthesia with the patient intubated nasally, in the following sequence:
Extraoral antisepsis of the face with degermant chlorhexidine and intraoral ant isepsis with alcoholic solution of 0.12% chlorhexidine. Gauze cap placement to protect the oropharynx and placement of Molt mouth gag. Tooth prophylaxis with Robinson brush and saline to remove biofilm from all teeth (Figure 4).
After local anesthetic with 2% Mepivacaine with norepinephrine to promote vasoconstriction and reduce local bleeding, the extraction of teeth #81, #71, and #74 was performed.
Absolute isolation, removal of enamel and cavity preparation with drills at high speed, carious tissue removal with drills at low speed, dentin excavation curettes and restoration of the following teeth and surfaces:
– 85: dental amalgam restoration lined with glass ionomer cement, BOL surfaces;
– 84: resin composite restorat ion MODLB surfaces;
– 83: resin composite restoration, LL surfaces;
– 82: resin composite restoration, L surface;
– 55: dental amalgam restoration, O surface;
– 54: dental amalgam restoration, OP surfaces;
– 53: resin composite restoration, MVP surfaces;
– 65: resin composite restoration, O surface;
– 64: resin composite restoration, O surface;
– 63: resin composite restoration, LPM faces;
– 75: resin composite restoration, OB surfaces;
– 73: resin composite restoration, LL faces;
– 72: resin composite restoration, L surface.
The Figures 5 and 6 show, respectively, the oral health status before and after dental treatment.


He returned five months after these procedures. At clinical examination, it was found that the restorations were in good condition, with no caries, but still with marked presence of oral biofilm. At that time, plaque disclosing procedures, hygiene guidance (parents were more interested), removal of biofilm with toothbrushing, application fluoride varnish, and reinforcement regarding food and diet were carried out. The child was very collaborative and after palatoplasty, he can be fed better. The Figures 7 and 8 show, respectively, the current oral health status of the child and his collaborative behavior in the chair.

Discussion
According to Andrade Júnior et al. 3, parents of individuals with cleft lip and palate become disoriented regarding to the procedures for the establishment of children's well-being. Thus, at prenatal care or after the birth, questions arise of how to care for the baby and how will be rehabilitation treatment. At that moment, the guidance and monitoring by a multidisciplinary health team are essential.
Parents who discover that their child has cleft lip and palate should look for all kinds of guidelines to enable full rehabilitation of the child. It is recommended that parents remain calm, because rejection, denial, and guilt can be considered normal at the first moment, but with professional help both the parents and the baby will have a healthy and happy life 12.
The individual with cleft lip and palate has normal personality and intellectual aspect; however, he/she may present common characteristics such as low self-concept, dependence on parents, avoidance of social contacts, communication difficulties, fear, shame, insecurity, low self-esteem, depression, inhibition as the severity of the deformity, stress, and difficulty in learning 8. These features can be aggravated if the guardians and caregivers are not properly oriented and able to look after the health of children with cleft lip and palate.
In this present case report, besides the parents' disinterest, various environmental factors involved, as distance to the care service, not speaking Portuguese, lack of basic health and hygiene, make difficult to follow-up and the appropriate treatment for the child.
The fact that the child does not speak and understand Portuguese, which would be critical to his compliance, was one of the main indications for the use of general anesthesia. Moreover, the treatment complexity and the need of the surgical treatment of palate were also contributory, because palatoplasty could not be performed in poor dental condition.
The oral health status of indigenous peoples in Brazil is very little known. The available studies have shown a worsening trend, particularly in the populations most exposed to changes in dietary patterns, including the incorporation of manufactured items, particularly refined sugar 6. The child of this case report daily ingested fermentable carbohydrate by breads and cakes.
It is expected that the family continues the treatment of the child until such time that all necessary corrections are made, and that dental treatment may also have aroused the family about the importance of oral hygiene and care with food. As for the precarious conditions in which they live, it is difficult to know what will be the prognosis of the treatments. Ironically, in the indigenous environment, caries risk is increasing due to the industrialized food, mainly sugar, changing diet habits.
Conclusion
The dental treatment under general anesthesia was indicated due to the dental condition that the child presented and the non-cooperation and misunderstanding of Portuguese language. We expected that the family incorporates the importance of dental care of the child, his hygiene, diet, and appointments with health professionals to complete treatment aiming at the quality of life of the child.
References
1. Allagh KP, Shamanna BR, Murthy GV, Ness AR, Doyle P, Neogi SB et al. Birth prevalence of neural tube defects and orofacial clefts in India: a systematic review and meta-analysis. Plus One. 2015;10(3):e0118961. [ Links ]
2. Amaral CER, Kuczynski E, Alonso N. Qualidade de vida de crianças com fissura labiopalatina: análise critica dos instrumentos de mensuração. Rev Bras de Cirurgia Plástica. 2011;26(4):639- 44.
3. Andrade Júnior CV, Oliveira LEG, Bandeira AP, Silva B.C, Jesus LD, Viana MFS et al. Estudo do índice de malformações orofaciais em neonatos no Hospital Geral Prado Valadares no município de Jequié – Bahia. Revista Saúde. 2009;5(2):108- 15.
4. Baroneza JE, Faria MJSS, Kuasne H, Carneiro JLV, Oliveira JC. Dados epidemiológicos de portadores de fissuras labiopalatinas de uma instituição especializada de Londrina, Estado do Paraná. Acta Scientiarum Health Sciences. 2005;27(1):31-5.
5. Brito LA, Cruz LA, Bueno DF, Bertola D, Aguena M, Bueno MRP. Fatores genéticos têm maior contribuição na etiologia das fissuras lábiopalatinas no interior do Ceará (região metropolitana do Cariri), Brasil. Rev Bras Cir Craniomaxilofacial. 2009;12(4):151-4.
6. Carneiro MCG, Santos RV, Garnelo L, Rebelo MAB, Coimbra Junior CEA. Cárie dentária e necessidade de tratamento odontológico entre os índios Baniwa do Alto Rio Negro, Amazonas. Ciência & Saúde Coletiva. 2008;13(6):1985-92.
7. Di Ninno CQMS, Gomes R, Santos P, Bueno M, Galvão DA, Meira A et al. O conhecimento de profissionais da área da saúde sobre fissura labiopalatina. Revista da Sociedade Brasileira de Fonoaudiologia. 2004;9(2):93-101.
8. Domingues ABC, Picolini MM, Lauris JRP. Desempenho escolar de crianças com fissura labiopalatina na visão dos professores. Revista da Sociedade Brasileira de Fonoaudiologia. 2011;16(3):310-6.
9. Figueiredo MC, Pinto NF, Silva DDF, Oliveira M. Fissura bilateral completa de lábio e palato: alterações dentárias de má oclusão – relato de caso clínico.Ciências Biológicas e da Saúde. 2008; 14(1):7-14.
10. Kianifar H, Hasanzadeh N, Jahanbin A, Ezzati A, Kianifar H. Cleft lip and palate: a 30- year epidemiologic study in North-east of Iran. J Otorrinolaringol. 2015 Jan;27(78):35-41.
11. Neves ACC, Patrocínio MC, Leme KP, Ui RT. Anomalias dentárias em pacientes portadores de fissuras labiopalatinas: revisão de literatura. Revista Biociência. 2002;8(2):75-81.
12. Ribeiro EM, Moreira ASCG. Atualização sobre o tratamento multidisciplinar das fissuras labiais e palatinas. Revista Brasileira de Promoção de Saúde. 2005;18(1):31-40.
13. Sandrini FAL, Chaves Junior AC, Beltrão RG, Panarello AF, Robinson MW. Fissuras labiopalatinas em gêmeos: relato de caso. Revista de Cirurgia e Traumatologia Buco-Maxilo-Facial. 2005;5(4):43-8.
14. Silva Filho OG, Ozawa TO, Borges HC. A influência da queiloplastia realizada em tempo único e em dois tempos cirúrgicos no padrão oclusal de crianças com fissura bilateral completa de lábio e palato. Rev Dental Press Ortodon Ortop Facial Maringá. 2007;12(2):24-37.
15. Souza J, Raskin S. Clinical and epidemiological study of orofacial clefts. J Pediatric. 2013;89(2): 137-44.
 Corresponding author:
Corresponding author:
Juliana Yassue Barbosa da Silva
Rua Professor Viriato Parigot de Souza, n. 5.300 – Campo Comprido
CEP 81280-330 – Curitiba – PR – Brasil
E-mail: juyassue@hotmail.com
Received for publication: July 12, 2015
Accepted for publication: September 4, 2015













