Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.13 no.1 Joinville Jan./Mar. 2016
Case Report Article
Surgical treatment of mandibular condyle fracture with bicortical screws: case report
Guilherme dos Santos Trento I; Paola Fernanda Cotait de Lucas Corso I; Naylin Danyelle de Oliveira II; Leandro Eduardo Klüppel I; Delson João da Costa I; Nelson Luis Barbosa Rebellato I; Rafaela Scariot I,II
I Federal University of Paraná – Curitiba – PR – Brazil
II Positivo University – Curitiba – PR – Brazil
ABSTRACT
Introduction: Mandibular condyle fractures are, of all facial fractures, those with the greatest controversies in relation to its conduct. Patient systemic condition, location and displacement degree of the fracture, mouth opening amplitude, and occlusion alteration are some factors that influence on the decision on conservative or surgical treatment. Pain, mandibular movement limitation, altered dental occlusion, and facial asymmetry are signs and symptoms that indicate condylar fracture. The surgical treatment consists of surgical fracture reduction and subsequent fixing through titanium miniplates and\or screws. Objective: The aim of this study was to report the case of a patient who had parasymphyseal fracture associated with left mandibular condyle fracture, presenting limited excursive movements of the jaw, pain in function, altered dental occlusion, and bruising on chin region. Case report: Due to the type of fracture and patient systemic condition, we decided to open reduction of fractures and stable internal fixation. Conclusion: At 12-month follow-up, the patient showed significant improvement in both clinical and functional condition, demonstrating the effectiveness of the treatment method and technique.
Keywords: surgery; mandible; mandibular fractures; jaw fixation techniques.
Introduction
Among all face fractures, mandibular condyle fractures show great difficult in diagnosing and no consensus regarding the treatment 9. Mandibular condyle fractures occur due to the energy absorption from direct impacts on the condyle, or more frequently, indirectly from impacts on the mandibular symphysis and/or parasymphysis, socalled counterblow fractures 12.
After the trauma, the signs and symptoms showed by the patient will help the dentist in diagnosing and planning the treatment 1. Pain complaints during function, on palpation of the fractured side, crackling, altered dental occlusion, limitation on mandible movements, shifting of the mouth opening toward the fractured side are the most common clinical signs 2.
Many factors influence on treatment decision: surgical – direct scanning of the fracture site, fragment reduction and fixture with titanium plates and/or screws 8; or conservative – maxillamandible block, physiotherapy with elastics or both 7 –, among them: patient's age, fracture site, displacement of the fractured fragment, other associated facial fractures, presence of teeth, and occlusion establishment 9.
The surgical approach is performed by exposing the fracture through facial access: preauricular or endaural, submandibular, and retromandibular. The choice for the access site will rely on the clinical characteristics of the fracture, the professional's expertise or preference, and association with fractures in other mandible or face's areas 4,12.
This case report aimed to show the surgical treatment through reduction and fixation with t itanium screws in a pat ient underwent left mandibular condyle fracture with displacement associated with contralateral parasymphyseal fracture.
Case report
Patient S.B.M., female, leucoderm, aged 45 years, with history of falling from the bicycle, was referred to the Service of Oral-maxillofacial Surgery and Traumatology of the Hospital XV, in Curitiba (PR, Brazil), complaining about pain and difficult in mastication and open the mouth.
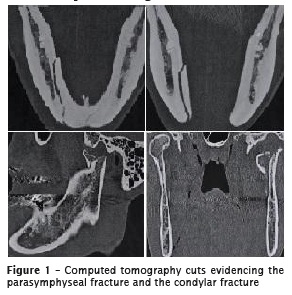
At anamnesis, the patient did not report any systemic disease, allergy, and comorbidities. At extraoral examination, the patient showed mild swallowing, and pain to palpation on left preauricular area; moderate swallowing and injury previously sutured on the right chin area; shifting on opening the mouth towards the left side, and only the right mandibular condyle was palpable. At intraoral examination, the patient exhibited altered dental occlusion characterized by shifting of the midline towards left and absence of posterior teeth contact. Imaging examinations showed left mandibular condyle fracture with medial displacement and right parasymphyseal fracture with left displacement (figure 1).
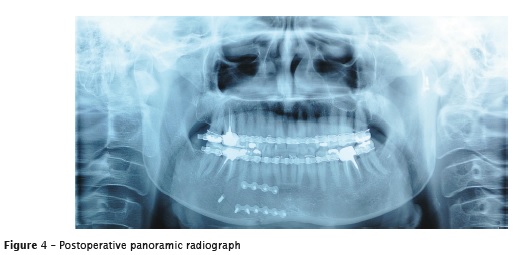
The treatment of choice was the surgical reduction and fracture fixation under general anesthesia. An Erich's plate was installed on both arches to block the maxilla and mandible trans operatively. To reduce the parasymphyseal fracture, an intraoral access was performed with reduction and fixation with two straight plates measuring 2.0 mm with ten monocortical screws and one bicortical screw. To reduce the mandibular condyle fracture, a preauricular access was performed. Following the exposure of the fragments, we noted the oblique fracture line. Fixation was accomplished through two bicortical screws measuring 2.0 mm (figure 2).

We prescribe antibiotics, anti-inflammatory, and analgesic drugs, post-operatively. Also, drugs to reverse peripheral neural traumatology and compressive disorders, elastic therapy, liquid diet, and oral hygiene instructions were prescribed. After 15 days, the patient showed no signs/symptoms of infection, proper oral hygiene, stable occlusal, and satisfactory healing.
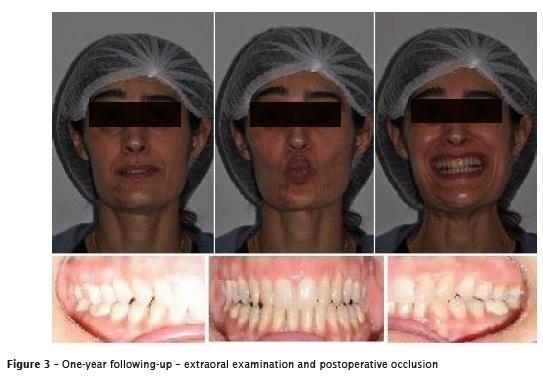
The panoramic radiograph of followingup showed proper reduction and fixation of the fractures and satisfactory position of the mandibular condyle. After 12 months of followingup, the patient was asymptomatic with satisfactory occlusion and free mandibular movements (figures 3 and 4).
Discussion
By opting to treat surgically, some aspects should be taken into account, such as: the type of surgical access and type of fixation. The extraoral access, as performed in this case report, is the choice of most of the surgeons to treat condylar fractures 3.
Ellis and Dean 3 reported that rigid internal fixation is the most used regarding to the steel wire osteosynthesis, while primary bone healing does not require maxilla-mandibular block, resulting in better postoperative comfort, as presented in this case report.
According to Sugiura et al. 11, surgical treatment comprise the surgical reduction of the fracture followed by fixation through titanium miniplates and screws, Kirschner wires or lag screw – the technique performed to reduce the mandible condyle fracture after evaluating the patient, the imaging examinations, and the observation of the fracture line. Gabrielli et al. 5 cited that it is not always easy to define the proper fixation type to treat mandibular fractures, that is, the surgeon must keep in mind the indications whenever choosing the fixation system and type. Thus, these indications will depend on the fractures characteristics, patient's behavior, lack of systemic diseases, proper care and postoperative following-up 5.
The aim of bicortical fixation of mandibular fractures is to provide the fixation and recovering of the fragments, enabling primary bone healing, promoting enough rigidity to the fractured fragments to resist to the movements along the fracture line during the mandible's normal function 6. This is considered as a simple, fast execution technique that allows the compression of the fractured fragments through rotation movements applied to the screw head during installation 10.
Conclusion
The treatment success of mandibular condyle fractures is associated with the correct diagnosis, choice of proper techniques, surgeon's expertise, and detailed postoperative following-up. Although the use of titanium miniplates and monocortical screws is largely indicated and used, the treatment with bicortical screws was effective and satisfactory for this fracture type.
References
1. Barros JJ, Manganello-Souza LC. Traumatismo buco-maxilo-facial. 2. ed. São Paulo: Roca; 2000. [ Links ]
2. Chacon EG, Larsen PE. Principles of management of mandibular fractures. In: Peterson's principles of oral and maxillofacial surgery. 2. ed. BC Decker Inc.; 2004. p. 401-33.
3. Ellis E, Dean J. Rigid fixation of mandibular condyle fractures. Oral Surg Oral Med Oral Pathol. 1993;76(1):6-15.
4. El l is E, Throckmorton GS. Treatment of mandibular condylar process fractures: biological considerations. J Oral Maxillofac Surg. 2005;63(1):115-34.
5. Gabrielli MAC, Gabrielli MFR, Marcantonio E, Hochuli-Vieira E. Fixation of mandibular fractures with 2.0mm: review of 191 cases. J Oral Maxillofac Surg. 2003;61:430-6.
6. Gorzelnik L, Kozlovski E. Bicortical extraoral plating of mandibular fractures. Atlas of the Oral and Maxillofacial Surgery Clinics. 2009;17(1): 35-43.
7. Hayward J, Scott RA. Fractures of mandibular condyle. J Oral Maxillofac Surg. 1993;1:57-61.
8. Laskin DM. Management of condylar process fractures. Oral Maxillofac Clin North Am. 2009 May;21(2):193-6.
9. Manganello LC, Silva AAF. Mandibular condylar fractures: classification and treatment. Rev Bras Otorrinolaringol. 2002;68(5):749-55.
10. Pereira ICS, Galdino AS, Palitó APPG, Santos TL, Barros F, Sobreira T. Redução cirúrgica de fratura mandibular oblíqua: parafusos transcorticais x placas e parafusos de titânio – relatos de caso. Rev Surg Traumatol Buco-Maxilo- Fac. 2011;11(3):69-76.
11. Sugiura T, Yamamoto K, Murakami K, Sugimura M. A comparative evaluation of osteosynthesis with lag screw, miniplates, or Kirschner wires for mandibular condilar process fractures. J Oral Maxillofac Surg. 2001;59: 1161-8.
12. Zachariades N, Mezitis M, Mourouzis, Papadakis D, Spanou A. Fractures of the mandibular condyle: a review of 466 cases. Literature review, reflections on treatment and proposals. J Craniomaxillofac Surg. 2006;34(7):421-32.
 Corresponding author:
Corresponding author:
Guilherme dos Santos Trento
Rua Belém, 61
CEP 80035-170 – Curitiba – PR – Brasil
E-mail: guilhermetrento@yahoo.com.br
Received for publication: November 1, 2015
Accepted for publication: December 22, 2015













