Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.13 no.1 Joinville Jan./Mar. 2016
Case Report Article
A simplified restorative technique of fractured maxillary anterior teeth
Adilson Yoshio Furuse I; Fabio Antonio Piola Rizzante I; Rafael Francisco Lia Mondelli I; Juliana Fraga Soares Bombonatti I
I Department of Operative Dentistry, Endodontics and Dental Materials, Bauru School of Dentistry, University of São Paulo – Bauru – SP – Brazil
ABSTRACT
Introduction: Fractures of the anterior teeth consists of a clinical condition that generates not only aesthetic and psychological problems, but may also cause dental pain. Thus, the affected teeth should be treated as urgencies in dental offices and their resolution whenever possible should be in a single session. Direct resin composite restorations should wherever possible be preferred due to the speed and possibility of obtaining good results. Objective: The objective of this case report is to describe the clinical sequence for restoration of a maxillary central incisor that presented a crown fracture using an immediate insert technique for resin composite (a "free hand" technique) with a modification to obtain dentin layer. Case report: A patient sought treatment after she fractured tooth #21. The restoration was performed with resin composite using the immediate technique. To facilitate the layering technique, the immediate insertion technique was changed for making the dentin lobes with the aid of a Teflon tape and the support with the index finger. Conclusion: The restoration of fractured anterior teeth can be performed quickly with the use of resin composites of different opacities and the use of the technique of immediate insertion proposed in this case report.
Keywords: smiling; esthetics; permanent dental restoration.
Introduction
Dental fractures due to trauma are common occurrences in permanent teeth. Among several factors are the increasing number of practitioners of contact sports (like soccer and martial arts) and automobile accidents; also, teeth tend to remain longer in the mouth and the restorative cycle itself increase trauma prevalence 3,14.
The trauma may affect the hard tissue (alveolar bone, enamel, dentin, and cementum) and adjacent soft tissues 2. The diagnosis of the extent of those injuries is fundamental to understanding the most appropriate treatment protocol.
The dental changes resulting from this clinical occurrence, in general, lead to a reduced quality of life of patients. This occurs because of the sensitivity and also because of the aesthetic conditions, reducing the quality of social life because of reduced self-esteem 1,9. The aesthetic factor is even more critical considering the standards of beauty socially imposed, where minimal changes in shape, color and/or positioning have become highly valued.
In dental trauma, restorative technique can be divided into immediate or mediate, depending on the availability or impossibility of performing the wax-up of the tooth fractured. The mediated technique, in which a silicone matrix is obtained from the waxing-up of the fractured tooth is faster and easier, because the matrix guides the palatal insertion of composite resin. On the other hand, the immediate technique with composite resin requires good technique and skills 6,7 and should, wherever possible, be used in cases of aesthetic emergency. This technique is also known as "free hand" technique 13. In these cases, the patient with a fractured anterior tooth often requires an immediate solution for the aesthetic problem.
A common problem found when employing immediate technique is to obtain the palatal contour of the restoration. The purpose of this case report is to demonstrate the restorative sequence of a fractured maxillary central incisor using a modified immediate technique to facilitate obtaining the shape of the palatal surface.
Case report
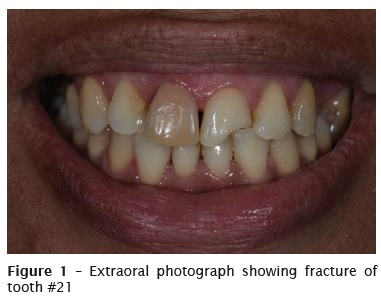
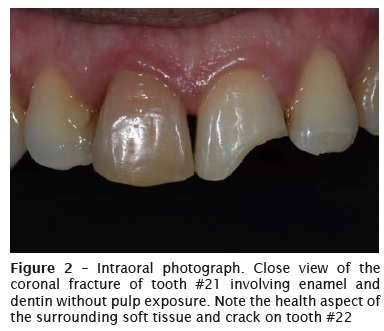
A patient, female, aged 32 years, sought treatment after fracture of tooth #21 (figure 1). The anamnesis, clinical and radiographic examinations were noncontributory. At intraoral evaluation, tooth #11 was darkened; tooth #21 had enamel-dentin fracture without pulp exposure and without involvement of the surrounding soft and hard tissues (figure 2). According to the patient, the fracture took place at sports practice and the tooth fragment was not found. The tooth #11 showed a satisfactory endodontic treatment and tooth #21 exhibit normal responses to pulp sensitivity test. The treatment planning comprised the restoration of the fractured tooth.
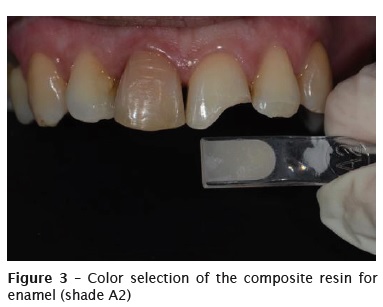
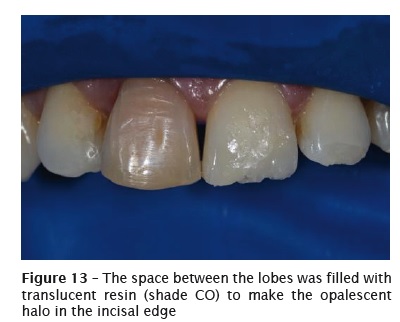
This was an esthetic emergency, so we opted to restore the tooth through immediate technique with resin composite (Charisma Diamond, Heraeus Kulzer, Hanau, Germany). First, color selection was performed through VITA scale for enamel resins, while for dentin resins, a predetermined scale based on the value/luminosity was used. Thus, following the scale of the resin system itself, shade A2 was selected for enamel and the corresponding shade OM (medium opaque) for dentin, associated with a opalescent effect resin (Clear Opal – CO), to obtain the translucent halo in the incisal edge (figures 3 e 4).

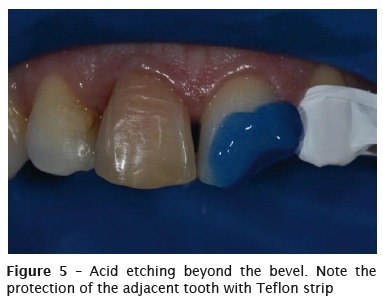
A concave bevel was made on the enamel of the fracture area with the aid of a flame-shape Diamond bur number #1111 (KG Sorensen, Cotia, SP, Brazil). Prior to the beginning of the restoration, the modified absolute isolation was executed with dental dam (Madeitex, São José dos Campos, SP, Brazil), to make easy the operative field visualization and to control moisten. The tooth #22 was protected with Teflon tape and tooth #21 enamel was etched for 30s (beyond the bevel) and dentin for 15 s with 37% phosphoric acid, (Heraeus Kulzer, Hanau, Germany) (figure 5). The adhesive system Gluma 2Bond (Heraeus Kulzer) was applied actively, at a single layer, on all etched area. After the solvent evaporation, gentle air jets for 5 s, the adhesive agent was light-cured for 20 s with LED device (Radii-cal, SDI, Bayswater, Victoria, Australia).
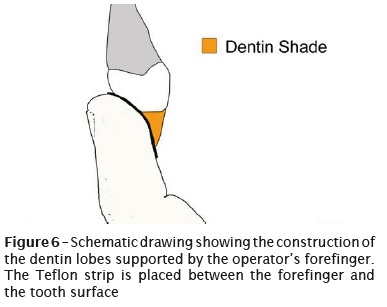
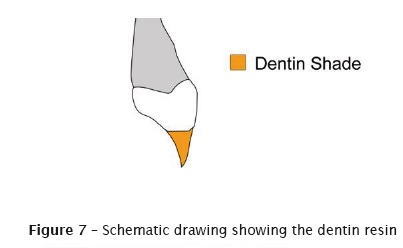
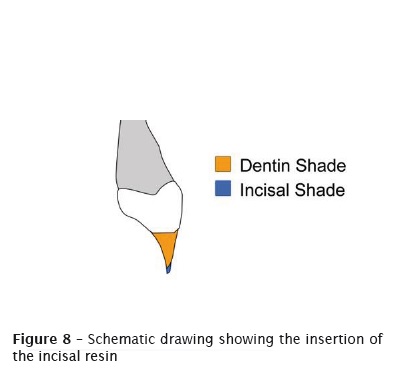
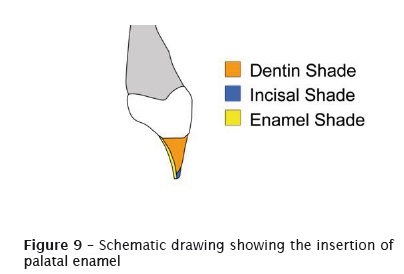
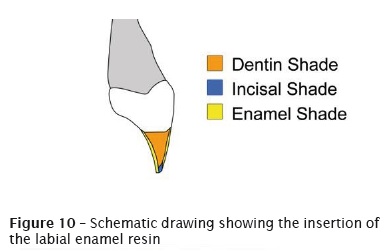
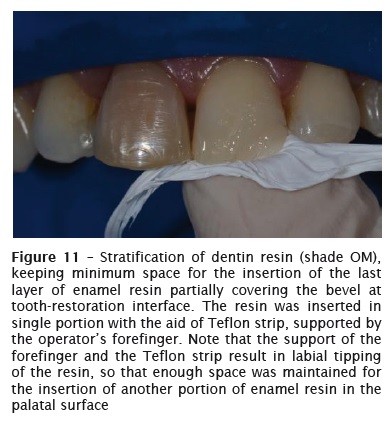
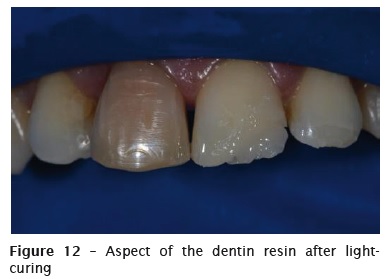
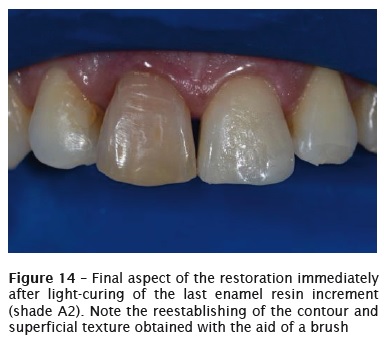
The immediate technique was modified to make the resin stratification easy. Thus, instead of making the palatal surface with enamel resin, the dentin lobes were supported with Teflon tape and the operator's forefinger (figure 6 to 10). The dentin lobes were constructed with resin shade OM (figure 11). This layer was inserted at single portion filling approximately half of the bevel extension to mask the fracture line, establishing the shape of the dentin lobes and keeping the space for the insertion of a thin translucent resin layer for enamel. After light-curing of this increment, the resin shade CO (translucent) was inserted between the lobes in the proximal surface (figure 12). On the resin for dentin, the resin for enamel was stratified, at single layer, reestablishing the contour and texture with the aid of a brush (Tigre, Joinville, SC, Brazil) (figure 13). The last resin layer covered the palatal surface with the same resin for enamel.
Occlusion adjustment was executed both at maximum habitual intercuspation and at the movements of protrusion and laterality. The initial finishing was performed with bulk-to-medium grit abrasive sandpapers (Diamond PRO, FGM, Joinville, SC, Brazil). The micro texture was obtained with the aid of an extra fine Diamond bur. The final polishing was performed with thin grit abrasive sandpapers and felt discs with diamond past (Diamond Master, FGM, Joinville, SC, Brazil). The final restoration is seen in figures 14 to 16.


Discussion
Dental fractures consist of aesthetic emergencies that can cause physical and psychosocial discomfort for patients 1,9 and should, whenever possible, be solved in a single session. For these cases, the restorative technique is relatively complex and requires great professional skill, so that the simplification of the techniques is highly desirable 6. The immediate restoration without obtaining a dental cast for waxing-up, the beginning of the restoration should simulate the condition provided in cases where there is a pre-waxing, i.e., the construction of the palatine surface 5,7,15,16. This procedure must be performed with the digital technique, which the convexity of the palatine surface is simulated with the interposition of a polyester or Teflon strip or with the aid of the forefinger. Care must be taken during this step to maintain the correct anatomy of the palatal surface and especially its inclination to provide the adequate space for the stratification of composite resin layers for dentin and then enamel. From the preparation of this surface, preferably with a more translucent or enamel resin, the restorative protocol becomes simpler, similar to a veneer that is, laminating resins with different opacities, mimicking the adjacent teeth, so that the restauration becomes indistinguishable.
Another possibility for simplifying the restorative technique consists of making an impression and waxing-up diagnosis of the fractured tooth with subsequent preparation of an addition or condensat ion silicone matrix. However, this technique demands one more appoint, making it impractical when the case is an esthetic emergency due to dental fracture.
This case report showed a restoring sequence of a maxillary central incisor fractured using the modified immediate technique to obtain the shape of the palatal surface. In this case, rather than first construct the palatal layer with enamel resin, we started by making the dentin layer. The rationale behind the use of this technique was that large Class IV cavities and large fractures, the immediate technique with digital support results in a palatal enamel layer usually very labially tipped , making difficult to obtain restorations with opacity compatible to that of the surrounding teeth.
An important question is the use of composites in the resolution of these cases, since it is a highly aesthetic restoration that requires a very accurate technique. It is noteworthy that the restorative technique with these materials, despite being more dependent on the professional skills, is more conservative and faster than an indirect restoration, providing long-term satisfactory results, due to the appropriate optical and mechanical properties of the current composite resins 6-8,11,17. However, the composites have limitations regarding the maintenance of the superficial characteristics and color stability, since it is known that the resins are subject to staining 4.
For the restoration of anterior teeth is essential the use of more opaque resin to simulate dentin. In general, it is recommended that such resin covers approximately half of the bevel made on enamel to disguise the fracture line 13. It is important noting that the bevel made on enamel improves the esthetics of the restoration and increases the area available for adhesion 10,12-14,16.
References
1. Almeida SB, Leonardi DP, Tomazinho FSF, Coelho BS, Giovanini AF, Pizzato E et al. The relationship of a clinical protocol and emergency treatment success of dental trauma running head: clinical protocol in dental trauma. RSBO. 2013 Oct-Dec;10:313-7. [ Links ]
2. Andreasen JO, Bakland LK, Flores MT, Andreasen FM, Andersson L. Traumatic dental injuries – a manual. 3. ed. Oxford: Wiley-Blackwell; 2011.
3. Collins CL, McKenzie LB, Ferketich AK, Andridge R, Xiang H, Comstock RD. Dental injuries sustained by high school athletes in the United States, from 2008/2009 through 2013/2014 academic years. Dent Traumatol. 2015 Sep 26. doi: 10.1111/edt.12228.
4. Cunha LF, Santana LOC, Baratto SSP, Mondelli J, Haragushiku GA, Gonzaga CC et al. Staining susceptibility of methacrylate and silorane-based materials: influence of resin type and storage time. RSBO. 2013;10(2):161-6.
5. Cunha LF, Valeretto TM, Pirolo R, Mondelli J, Gonzaga CC, Furuse AY. Free-hand stratification with composite resins for the closure of anterior diastema. RSBO. 2012 Jul-Sep;9(3):334.
6. Devoto W, Saracinelli M, Manauta J. Composite in everyday practice: how to choose the right material and simplify application techniques in the anterior teeth. Eur J Esthet Dent. 2010 Spring;5(1):102-24.
7. Eden E, Taviloglu E. Restoring crown fractures by direct composite layering using transparent strip crowns. Dent Traumatol. 2015 Oct 8. doi: 10.1111/edt.12233.
8. Ferracane JL. Resin composite – state of the art. Dent Mater. 2011 Jan;27(1):29-38.
9. Golai S, Nimbeni B, Patil SD, Baali P, Kumar H. Impact of untreated traumatic injuries to anterior teeth on the oral health related quality of life as assessed by video based smiling patterns in children. J Clin Diagn Res. 2015 Jun;9(6): Zc16-9.
10. Heintze SD, Rousson V, Hickel R. Clinical effectiveness of direct anterior restorations – a metaanalysis. Dent Mater. 2015 May;31(5):481-95.
11. Manauta J, Salat A, Putignano A, Devoto W, Paolone G, Hardan LS. Stratification in anterior teeth using one dentine shade and a predefined thickness of enamel: a new concept in composite layering – part II. Odontostomatol Trop. 2014 Sep;37(147):5-13.
12. Mizuno SK, Rizzante FAP, Cunha LF, Furuse AY, Mondelli RFL, Mondelli J. Effect of beveling on the marginal leakage of class IV composite resin restorations. RODYB. 2015 Jan-Apr;4(1):43-9.
13. Mondelli J. Fundamentos de dentística operatória. São Paulo: Santos; 2006.
14. Ozel E, Kazandag MK, Soyman M, Bayirli G. Two-year follow-up of fractured anterior teeth restored with direct composite resin: report of three cases. Dent Traumatol. 2008 Oct;24(5):589-92.
15. Pontons-Melo JC, Pizzat to E, Furuse AY, Mondelli J. A conservative approach for restoring anterior guidance: a case report. 2012 Jun;24(3):171-82.
16. Romero MF. Esthetic anterior composite resin restorations using a single shade: step-by-step technique. J Prosthet Dent. 2015 Jul;114(1): 9-12.
17. Villarroel M, Fahl N, Sousa AM, Oliveira Jr. OB. Direct esthetic restorations based on translucency and opacity of composite resins. J Esthet Restor Dent. 2011 Apr;23(2):73-87.
 Corresponding author:
Corresponding author:
Adilson Yoshio Furuse
Universidade de São Paulo
Departamento de Dentística da Faculdade de Odontologia de Bauru
Alameda Dr. Octávio Pinheiro Brisola, 9-75
CEP 17012-901 – Bauru – São Paulo – Brasil
E-mail: furuse@usp.br
Received for publication: January 20, 2016
Accepted for publication: February 14, 2016













