Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.13 no.1 Joinville Jan./Mar. 2016
Case Report Article
Crown lengthening surgery and transurgical restoration
Isabô Hayná Gomes Tortoriello I; Luana Kelle Batista Moura I; Raphael Camargo Costa I; Milena Salete de Souza Pinto I; Vivian Colucci I; Andrea Marcia Marcaccini I
I Department of Dentistry, University of Ribeirão Preto – Ribeirão Preto – SP – Brazil
ABSTRACT
Introduction: The crown lengthening surgery and the transurgical restoration are alternative procedures to enable the restoration of teeth inaccessible to the conventional techniques and restore the lost biological space. Objective: This study aimed to present clinically the reconstruction of a right maxillary second molar through crown lengthening surgery associated with transurgical restoration with composite resin in a patient treated in the Integrated Clinics of the University of Ribeirão Preto. Case report: Patient E.H.C.V., female, aged 51 years, attended the dental clinic of the University of Ribeirão Preto. The anamnesis showed a favorable health history and the clinical examination showed great tooth crown destruction of tooth #17. The treatment planning included the crown lengthening periodontal surgery with regularization of alveolar bone on the buccal surface of tooth #17, rubber dam isolation, the restauration of the compromised area with composite resin, and suture in the same session. After 7 days, the sutures were removed and the restoration polished. Conclusion: It can be concluded that the use of this technique is a viable, fast, and satisfactory solution, with good results, favoring the health and aesthetics, returning function and better social life to the patient.
Keywords: surgical restoration; crown lengthening surgery; biological space.
Introduction
Appropriate restorative procedures do not always provide optimal clinical conditions for its implementation. Thus, suboptimal clinical conditions may prevent the expected and desired procedures through technical and biological standards 3,19,18. Different protocols must be designed to access to the cervical cavit y wall, in addition to a dry operative field free of contamination by blood and saliva 5.Thus, among the alternatives of restorative treatment planning and implementation in some of these situations, only the surgical periodontal procedures may create favorable technical conditions 15.
To restore the biological space and obtain better access to the lesion, it is necessary to choose periodontal surgeries as clinical crown lengthening and/or transurgical restorations 1,5,16. The transurgical restorations are restorative procedures performed in combination and common periodontal-surgical access. They comprise the convenience form in situations where the full access of the injury cannot be obtained more conservatively. The transurgical procedures may be indicated for subgingival cavities, crown-root fractures, perforations, external root resorption and in some cases associated with the recovery of the periodontal biological space 8.
However, the indication of this approach should undergo a careful clinical examination, both for the general health of the patient and the specific clinical case 13. Some preliminary considerations should be evaluated to ensure the success of the treatment, such as radiographic/clinical evaluation, possible isolation conditions of the operative field, and restorative alternatives to the case in question 11,12,17.
In cases which subgingival restorations are necessary, it is important to maintain a distance of at least 3 mm from the edge of the crown and the top of the bone crest 6. When this distance is less than 3 mm, clinical crown lengthening with osteotomy is required aiming at removing the bone tissue until the biological space is recovered 6 This distance is determined by the need of the insertion of gingival fibers from the connective tissue, promoting the health of the surrounding periodontal tissue 4,15.
As in all minor oral surgery, crown lengthening followed by transurgical restoration requires a very critical planning to reach optimal conditions for the restoration 7. The choice of restorative material becomes imperative. Thus, the composite resins are the most suitable material to maintain direct contact with the periodontium, since they have a smooth surface, fully satisfactory polishing, reducing the plaque accumulation 9,12.
With the justification and importance of the need for proper restorative procedure, this case report aimed to present the clinically reconstruction of a right maxillary second molar through crown lengthening associated with transurgical composite resin restoration, emphasizing the clinical relevance of this procedure today.
Case report
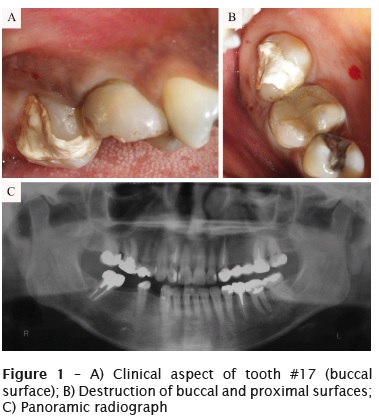
Patient, female, aged 51 years, attended to the Dental Clinics of the School of Dentistry of Ribeirão Preto with chief complaint of "destruction of one of the right upper teeth". After the clinical examination, it was observed that the entire buccal and proximal surfaces of the right maxillary second molar were extensively destroyed ending subgingivally at buccal surface.
The other teeth were sound. During anamnesis, the patient reported no use of medication, no trauma or other factor related to the tooth destruction (figures 1A and 1B). A panoramic radiograph was requested aiming to comprehensive observation of the case (figure 1C).
Based on the clinical and radiographic examinations, we opted for transurgical composite resin restoration. As pre-operative procedure, no prophylact ic medicat ion was needed. All surgical procedures were performed under strict biosecurity standards. Next, the patient rinsed 0.12% chlorhexidine solution and extraoral antisepsis was performed with iodized alcohol (mixture of 50% alcohol and 0.1% iodine) on the lower face of the patient.
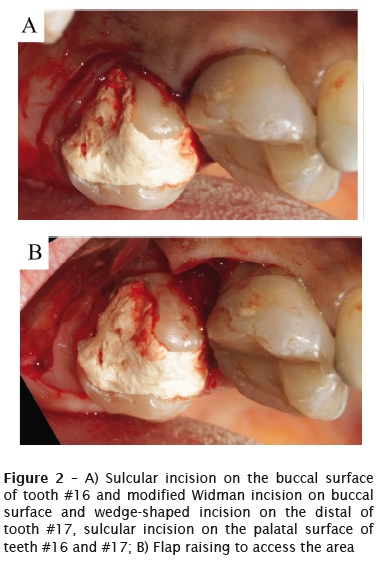
Next, local anesthesia comprised blockage of the greater palatine nerve and infiltrative anesthesia of right upper posterior and medium alveolar nerves. Then, with the aid of scalpel (Golgran, São Cateano do Sul, SP, Brazil) and size 15 blade (Solidor, Barueri, SP, Brazil), the wedge-shaped incision was performed on the posterior edentulous area of tooth #17, with approximately 3 mm from the two incisions comprising the wedge. We opted to perform the modified Widman incision 10 from the distal buccal area to the medium of the buccal surface, approximately 2 mm far from the gingival sulcus. Sulcular incision extended from the half of the buccal surface to the mesial surface of tooth #16, as seen in figure 2A. At the palatal surface, the sulcular incision extended from the distal surface of tooth #17 to the distal surface of tooth #15.
After the flap raising (figure 2B), the attached gingival tissue was removed with the aid of size 4 Goldman-Fox periodontal curette (Golgran, São Cateano do Sul, SP, Brazil), allowing a clear view of the bone tissue.
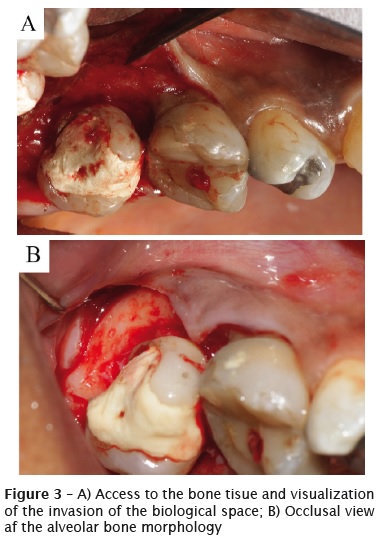
By observing the bone tissue and the attached gingival fibers, we performed root scaling and polishing through Gracey curettes sizes #7-8, #11- 12, and #13-14 (Hu-Friedy Mfg. Co., LLC, Chicago, IL, USA) around all teeth and roots exposed by total flap raising (figure 3A).
The measurement from the lesion terminus to the bone crest was performed with the aid of a periodontal probe (15 UNC/CP 11,5B, Hu-Friedy Mfg. Co., LLC, Chicago, IL, USA), on all flap extension aiming to verify which areas the bone contour should be modified for crown lengthening. Those measurements below 3 mm received great care. The distal-buccal and buccal surfaces lost the space for the insertion of collagen gingival fibers, thus, receiving crown lengthening. The osteotomy of these surfaces was performed through high-speed handpiece (Silent, Dabi Atlante, Ribeirão Preto, SP, Brazil) with round diamond bur (1011HL, KG Sorensen, Cotia, SP, Brazil), followed by ogival diamond bur (3118, KG Sorensen, Cotia, SP, Brazil) and constant irrigation with saline solution (figure 3B). At the ending of the surgical procedures, the operative field underwent rubber dam isolation (W8A clamp, Duflex, Rio de Janeiro, RJ, Brasil).
All provisional material (zinc oxide and eugenol - IRM, Dentsply, Petrópolis, RJ, Brazil) were removed with the aid of high-speed handpiece (Silent, Dabi Atlante, Ribeirão Preto, SP, Brazil), and round diamond bur (1014HL, KG Sorensen, Cotia, SP, Brazil) and constant irrigation. The preparation comprised the removal of the provisional material. The tooth was vital and the dentin-pulp complex was lined with calcium hydroxide cement (Hidro C, Dentsply, Petrópolis, RJ, Brazil) and glass ionomer cement liner (Vidrion F, SS White Artigos Dentários Ltda., Rio de Janeiro, RJ, Brazil).
The right maxillary second molar was etched for 15 seconds on enamel with 37% phosphoric acid (Condicionador Dental Gel; Dentsply Ind. e Com. Ltda., Petrópolis, RJ, Brazil) with the aid of a disposable brush (Brush regular, KG Sorensen, Cotia, SP, Brazil).
After water rinsing, the excess was removed with he aid of absorbent paper. The adhesive system Single Bond Universal (3M ESPE, St. Paul, MN, USA) was applied with other disposable brush (Brush, KG Sorensen, Cotia, SP, Brazil), followed by light-curing for 20 seconds (Ultraled; Dabi Atlante, Ribeirão Preto, SP, Brazil).
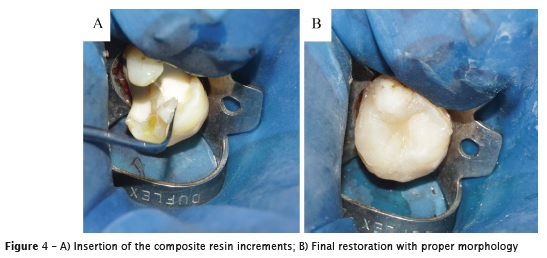
The micro-hybrid composite resin shade A2 (Herculite Classic; Kerr, Orange, CA, USA) was inserted in increments of 2 mm thickness (figure 4A) and light-cured for 40 seconds on each increment. The rationale behind the use of shade A2 form Vita scale (Wilcos do Brasil Indústria e Comércio Ltda., Petrópolis, RJ, Brazil) was that this shade was the most compatible with the shades of the lost tooth structures.
After the restoration conclusion (figure 4B), rubber dam was removed and we observed the proper morphology of the buccal surface close to the surgical area. The flaps were suture with silk suture size 4.0 (Ethicon, Johnson & Johnson, São Paulo, SP, Brazil). Immediate restoration finishing was performed with sandpaper polyester strips (KG Sorensen, Cotia, SP, Brazil) to restore the contact point with the surrounding tooth.
Occlusal adjustment was performed with the aid of diamond finishing bur (KG Sorensen, Cotia, SP, Brasil) at high speed and constant irrigation. After one week, sutures were removed and restoration polishing was accomplished with fine and extra fine abrasive silicone points (KG Sorensen, Cotia, SP, Brazil) associated with diamond paste (Diamond Gloss 1 and 2 - KG Sorensen, Cotia, SP, Brazil) to achieve a better finishing. At that moment, the gingival tissue showed proper aspect with adequate healing and no inflammation.
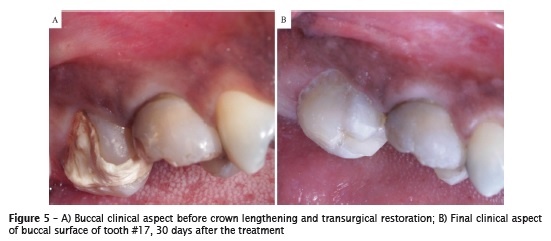
The patient was followed-up for polishing the other restorations. At 30 postoperative days, the dental tissues showed good aspect (figures 5A and 5B) and the patient was satisfied with the obtained result.
Discussion
The dentist should apply specific criteria to decide the best treatment proposed for each case. These criteria should involve mechanical, functional, biological, and aesthetic aspects. Restorations are dependent on the rate, extent, failure type, and the quality of the site where they will be performed. The advantages of this procedure are to minimize loss of tooth structure and increase longevity at a low cost without compromising the involved tooth 2.
The success of the restorative procedure depends, among other factors, on the maintenance of pulp vitality and periodontal health. In cavities that invade the biological space, the surgery recovering this space is of fundamental importance to obtain the adequate restoration 6.
Maintaining periodontal health is paramount to the long-term success of the restored teeth. One of the factors that may cause the loss of a restored tooth is the invasion of the biological space, which can have the restoration subgingivally invading the structures. This invaded space can lead to the occurrence of inf lammation of the periodontal tissues, the ability to promote some complications such as clinical attachment loss, increased probing pocket depth, increased visual signs of inflammation, and bone loss 8.
Faced with the options available in dentistry under graduation clinics, in this case report, we specifically opted to accomplish transurgical restoration. This approach is not the most suitable in most cases, since crown lengthening allows for a better placement of the gingival tissue and facilitates the restorative procedure. However, in this case report, the unknown origin of the injury associated with the lack of clinical viewing of the end of the lesion corroborated for choosing the technique. The access to bone tissue through total flap enabled to view the end of the injury and perform crown lengthening. During the measurements, we observed distances smaller than 3 mm, indicating the need for bone osteotomy followed by osteoplasty. Obtained the minimum distance of 3 mm between the bone crest and cervical limit of the injury, rubber dam isolation of the operative field was performed. This is extremely important in any restorative procedure for control of moisture. This control is essential to restore the adhesiveness of the restoration 20. In the case described herein, the isolation involved only the treated tooth, also effective for adequate control of bleeding that occurs during surgery, since the suturing of the flaps had not been performed.
The cavity preparation comprised only the removal of temporary filling material that was in the tooth. We opted to perform a direct restoration with composite resin, because it is a simpler approach with lower cost, but with adequate and satisfactory results 2. Also, the choice was due to the limited occlusion of the patient on that area. The surrounding teeth had short crowns, which would hinder the choice for partial crown.
Its importance becomes even more apparent when we consider that much of the population has no access to dental procedures, especially those with expensive cost and operating time, for example, ceramic restorations, implants or orthodontic devices 14. The use of direct restoration with composite resin proved to be a viable option with good aesthetic and functional results.
By choosing the transurgical restoration, the choice for composite resin is an excellent alternative, always remembering that a correct and proper polishing should be performed to reduce the plaque accumulation. This type of intervention has great accessibility for patients of both public and private health, increasing the range of restorative dentistry. However, a multidisciplinary approach to restorative procedure is of paramount importance in clinical success, preserving periodontal health and pulp vitality.
Conclusion
The restorative procedure with composite resin carried out during the clinical crown lengthening may be a viable and fast alternative for providing rehabilitation in cases of severe loss of tooth structure.
References
1. Almeida ALPF, Esper LA, Sbrana MC, Cunha MJS, Greghi SLA, Carrilho GPB et al. Relationship between periodontics and restorative procedures: surgical treatment of the restorative alveolar interface (RAI) – case series. J Indian Prosthodont Soc. 2013 Dec;13(4):607-11.
2. Bacchi A, Cavalcanti LMA, Schneider LFJ, Consani RLX. Reparos em restaurações de resina composta. Rev Facul Odontol UFP. 2010 Sep/ Dec;15(3):331-5.
3. Bajaj P, Chordiya R, Rudagi K, Patil N. Multidisciplinary approach to the management of complicated crown-root fracture: a case report. J Int Oral Health. 2015 Apr;7(4):88-91.
4. Carvalho PFM, Silva RC, Joly JC. Aumento de coroa clínica estético sem retalho: uma nova alternativa terapêutica. Rev Assoc Paul Cir Dent. 2010 Jan;1(2):26-33.
5. Dantas AAR, Silva ERC, Sako JS. Tratamento estético periodontal: revisão de literatura sobre alguns tipos de cirurgia. Rev Odontol Univ Cid São Paulo. 2012 Sep/Dec;24(3):226-34.
6. Elias MG, Carvalho W, Barboza EP. Localização da margem dos preparos em restaurações estéticas: uma discussão em relação à saúde periodontal. Rev Gaúcha Odont. 2013 Jul/Dec;61(0):441-5.
7. Faria-e-Silva AL, Moura AS, Silva AM, Rodrigues JL, Caldeira-Brant L. Restauração transcirúrgica de pré-molar com lesão extensa idiopática: relato de caso. Clínica e Pesquisa em Odontologia. 2010 Jan;2(1):53-9.
8. Ferreira Junior CD, Reis MMGC, Barboza ESP. Recuperação do espaço biológico: uma discussão das medidas utilizadas nas cirurgias de aumento de coroa clínica com osteotomia. Rev Gaúcha de Odontol. 2013 Jul/Dec;61(0):519-22.
9. Garcia RN, Silva CS, Silva GG, Mocellin G, Ozelame J, Fracasso L et al. Bonding performance of a self-adhering flowable composite to indirect restorative materials. RSBO. 2014 Jul;11(1):6-12.
10. Mailoa J, Lin G-H, Khroshkam V, MacEachern M, Chan H-L, Wang H-L. Long-term effect of four surgical periodontal therapies and one non-surgical therapy: a systematic review and meta-analysis. J Periodontol. 2015 Oct;86(10):1150-8.
11. Masioli MA, Pimentel FL, Louro RL, Masioli DLC. Reparo em restaurações de resina composta: procedimento simples e conservador. Rev Bras Pesq Saúde. 2006 Sep/Dec;8(3):38-43.
12. Michelon C, Hwas A, Borges MF, Marchiori JC, Susin AH. Restaurações diretas de resina composta em dentes posteriores – considerações atuais e aplicação clínica. Rev Faculdade Odontologia UPF. 2009 Sep/Dec;14(3):256-61.
13. Muncinelli EAG, Pini NIP, Ferrari WF, Nunes MCP. Tratamento reabilitador integrado no restabelecimento funcional e estético: relato de caso. Rev Flum Odontol. 2011 Jul/Dec;17(36):44-6.
14. Pinho T, Neves M, Alves C. Multidisciplinary management including periodontics, orthodontics, implants, and prosthetics for an adult. Am J Orthod Dentofacial Orthop. 2012 Aug;142(2):235-45.
15. Rissato M, Trentin MS. Aumento de coroa clínica para restabelecimentos das distâncias biológicas com finalidade restauradora – revisão da literatura. Rev Facul Odontol UFP. 2012 May/ Aug;17(2):234-9.
16. Sharma A, Rahul GR, Poduval ST, Shetty K. Short clinical crowns (SCC) – treatment considerations and techniques. J Clin Exp Dent. 2012 Oct;4(4):230-6.
17. Sobreira FMS, Azevedo CR, Freitas Filho LHS, Vidal APV, Barros LF, Ferreira MP. Métodos de reparo em resina composta: uma revisão. Odontol Clín-Cient. 2008 Apr/Jun;7(2):123-8.
18. Sousa SJB, Magalhães D, Silva GR, Soares CJ, Soares PFB, Santos-Filho PCF. Cirurgia plástica periodontal para correção de sorriso gengival associada a restaurações em resina composta: relato de caso clínico. Rev Odontol Brasil Central. 2010 Aug;19(51):362-6.
19. Tomar N, Bansal T, Bhandari M, Sharma A. The perio-esthetic-restorative approach for anterior rehabilitation. J Indian Soc Periodontol. 2013 Jul;17(4):535-8.
20. Trinta CC, Costa JF, Carvalho RCC, Leite SAM, Conde DM, Carvalho AS. Effect of substrate and adhesive system type on composite resin restorations. RSBO. 2013 Oct/Dec;10(4):306-12.
 Corresponding author:
Corresponding author:
Andrea Marcia Marcaccini
Universidade de Ribeirão Preto – Unaerp
Avenida Costábile Romano, n. 2201 – Ribeirânia
CEP 14096-900 – Ribeirão Preto – SP – Brasil
E-mail: amarcaccini@hotmail.com
Received for publication: February 21, 2016
Accepted for publication: March 16, 2016













