Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.13 no.2 Joinville Abr./Jun. 2016
CASE REPORT ARTICLE
Diagnosis and clinical management of pre-eruptive intracoronal resorption – a case report
Bianca Fiorentin MouraI; Gustavo Ricardo SilveiraII; Sinval Adalberto Rodrigues-JuniorI,III
I School of Dentistry, Universidade Comunitária da Região de Chapecó – Chapecó – SC – Brazil
II Private clinic – Chapecó – SC – Brazil
III Health Sciences Postgraduate Program, Universidade Comunitária da Região de Chapecó – Chapecó – SC – Brazil
ABSTRACT
Introduction: The pre-eruptive intracoronal resorption is a carieslike lesion frequently located in dentin underneath the dentinenamel junction in the occlusal face of the tooth crown. Due to the resemblance with carious lesions, this lesion is often referred to as 'pre-eruptive caries', although its pathogenesis has no correlation with the carious mechanism. Objective: This case report describes the diagnosis and clinical management of a permanent second molar presenting intracoronal pre-eruptive resorption, highlighting the possible clinical conducts associated.Case report: Diagnosis of the condition was accidental, through routine panoramic radiograph taken for orthodontic reasons. The therapeutic option involved the surgical exposure of the non-erupted tooth, exposure of the lesion and removal of the tissue from the resorbed area. Restoration was performed using glass ionomer cement followed by composite resin. At the 9-month follow-up the patient presented no further clinical symptom of recurrence of the resorption or pain. Conclusion: Despite being a relatively rare condition, clinicians should be aware of the possibility of PEIR occurrence and perform a cautious radiographic examination.
Keywords: case reports; childhood; oral health.
Introduction
Pre-eruptive intracoronal resorption (PEIR) is a condition characterized by the presence of a radiolucent lesion with varying depths located at the coronal dentin of non-erupted teeth, adjacent to intact enamel 1. In most cases, a single tooth is affected, although cases involving several teeth have also been reported 15. Due to the resemblance with carious lesions, this lesion has been referred to as 'pre-eruptive caries' 4, although the correct term used to characterize its nature is 'pre-eruptive intracoronal resorption' – PEIR 1,9.
The pathogenesis of the PEIR is not clear, since the non-erupted tooth is not susceptible to be infected with cariogenic microorganisms 14. Normally a single tooth is affected and approximately half the lesions extend to more than two thirds of the dentin thickness 1,10. No association has been found between the PEIR and gender, race, medical conditions, systemic conditions or fluoride supply 10,11,14.
The diagnosis is usually based on routine bitewing or panoramic radiographs. Nevertheless, most lesions remain hidden until there is pulpal involvement or fracture of cusps due to extensive cavitation 13. PEIR may be an important cause of uncommon pulpal abscesses in children whose teeth present a short eruption time span 1.
The aim of this case report is to describe the diagnosis and clinical management of a manifestation of PEIR in a non-erupted lower second molar, including a 9-month follow-up.
ature review
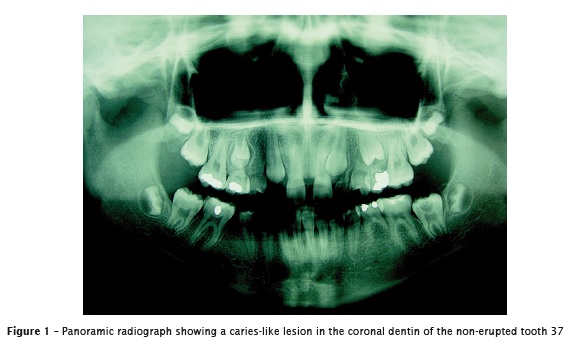
A 14-year-old female patient searched for pediatric dental treatment in Chapecó, Southern Brazil, presenting no relevant clinical symptoms or complaints. A panoramic radiograph, taken for orthodontic reasons (figure 1) revealed the presence of an extensive radiolucent lesion in occlusal dentin underneath the enamel-dentin junction in the nonerupted permanent mandibular left second molar.
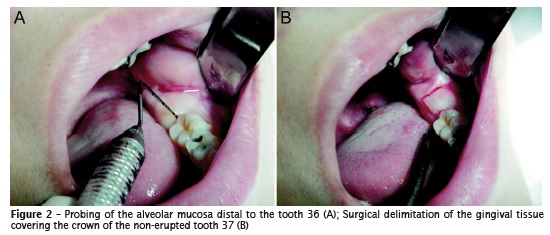
Medical history revealed no systemic disease or allergy. However, the patient presented agenesis of the maxillary lateral incisors and mandibular second premolars. The clinical exam revealed that the alveolar mucosa distal to the first molar presented normal color, texture, and contour (figure 2.A). The presence of a radiolucent area in the occlusal dentin of the non-erupted mandibular second molar was confirmed with a periapical radiograph.
The lesion was diagnosed as a pre-eruptive intracoronal resorption that did not involve the periapical region of the tooth. Therefore, the treatment decision involved surgical access for removal of the tissue present in the reabsorbed area, followed by restoration of the coronal cavity.
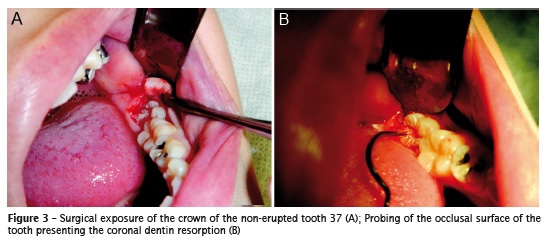
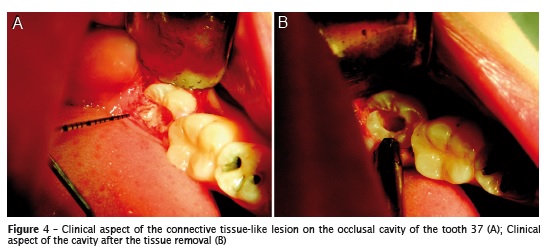
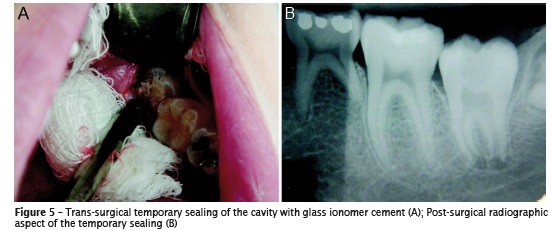
Local anesthesia was administered in the region (2% lidocaine solution with 1:100.000 adrenaline). The gingival tissue over the non-erupted second molar was surgically delimited (figure 2.B) and, following, removed, revealing the occlusal surface of the second molar (figure 3.A). The occlusal surface was probed (figure 3.B) and, then, a cavity was opened with high speed bur. The tissue found in the cavity was non-bleeding and pale-pink colored, similar to the conjunctive tissue (figure 4.A), and was removed with an excavator. The cavity floor was hard to probing and white-colored and no contact with the pulp tissue was identified (figure 4.B). The cavity was filled with conventional glass ionomer cement (Maxion R, FGM, Joinville, SC, Brazil) (figure 5.A). After the procedure, a periapical radiograph was taken to verify the marginal adaptation of the glass ionomer cement (figure 5.B).
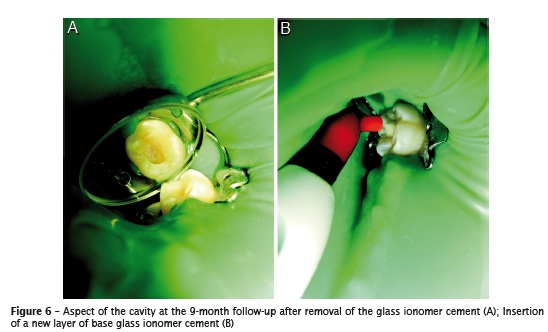
Nine months after the surgical procedure and with the tooth completely erupted, vitality test was repeated and accused pulp vitality. Following, rubber dam isolation was performed and the temporary filling was totally removed using a diamond bur at high speed under water cooling. The option for removing the glass ionomer cement was due to the fact that it was inserted during surgery with no visual certainty of lack of contamination. The cavity was visually inspected and the glass ionomer cement was inserted as liner material (figure 6.A and B).
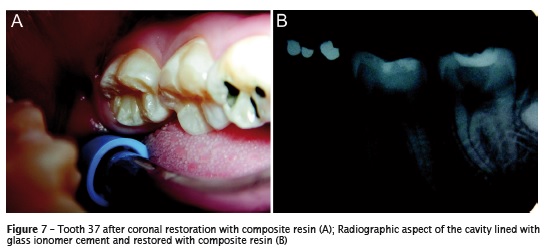
Enamel and dentin were etched with phosphoric acid gel for 30 and 15 seconds, respectively. The phosphoric acid was washed out for 30 seconds with water jets and the two-step etch-and-rinse adhesive system Adper Single Bond 2 (3M/ESPE, St. Paul, MN, USA) was applied according to the manufacturer's instructions. After having its solvent evaporated for 30 seconds with the aid of gentle air jets, it was light cured using a LED light-curing unit producing more than 300 mW/cm2 (Emitter C, Schuster, Santa Maria, RS, Brazil). The restorative composite Charisma (shade A2, Heraeus Kulzer, Hanau, Germany) was incrementally inserted and each layer was light cured for 20 seconds. figure 7shows the clinical and radiographic aspect of the final restoration.
Discussion
This case report described the accidental diagnosis of an asymptomat ic pre-erupt ive intracoronal resorption occurring in a permanent mandibular second molar through a panoramic radiograph taken for orthodontic reasons. Younger subjects are more prone to have this condition diagnosed in panoramic radiographs, since nonirrupted teeth are assessed radiographically more often in such age due to orthodontic planning 12. According to Uzun et al. 16, these lesions have no obvious predilection for race or gender; another study revealed that the most commonly affected teeth were the lower second molars 8. Lesions of this nature often progress asymptomatically and, hence, are difficult to diagnose, strongly depending on the dental professional awareness during radiographic examination 16.
Dental literature has reported a prevalence of PEIR lesions varying from 1.55% to 6% 8,11. Most recently, though, a large scale multicenter study involving a population of almost 30,000 people identified a 0.7% prevalence of PIER 16. According to the authors, the discrepancy in prevalence values may derive from diagnosis standards of what is assumed to be PEIR in different radiographic techniques. In spite of that, it is fair to assume that there is little information on the epidemiology of PEIR in dental literature, as well as on factors, if any, that might favor its appearance 6.
Typically, ostensibly intact superficial enamel is observed in the radiograph, resembling the characteristics of 'occult caries' or 'hidden caries' 12. Regardless, prior evidence reveals that the it is not likely that these lesions occur due to infection and demineralization of the non-irrupted tooth 6,11. Histology of the tissue present in the lesions showed a soft tissue containing spindleshaped cells that resemble fibrous connective tissue cells and resorptive cells, such as multinucleated osteoclasts and macrophages 6. Other differential diagnosis could include enamel hypoplasia or Turner´s hypoplasia; however, both conditions would present other signs, such as prior infection or other hypoplastic teeth1, which were not observed.
The natural course of PIER is usually slow before the tooth's eruption and is hardly associated to pain or any other clinical symptom until the lesion reaches the pulp 12. On the other hand, these lesions tend to be rapidly colonized by microorganisms when the tooth erupts and to evolve into carious lesions of rapid progression with potential to cause pulpal abscesses 1. Therefore, it has been recommended that the management of PIER should focus on the early diagnosis and treatment 12, including the surgical exposure of a non-irrupted tooth as soon as the lesion is recognized aiding at the arrestment of the resorption and the restoration of the tooth´s crown 2,5,9. The decision for the surgical treatment in this case was taken considering that, even though the lesion did not compromise the pulp at the moment of discovery, it was deep and could evolve causing pain.
Removal of the resorptive tissue in this case was followed by filling of the cavity with conventional glass ionomer cement, due to benefits this material provides as temporary filling, namely, minimal tooth preparation, adequate viscosity for insertion using a centrix syringe and quick adjustment 2. Additionally, the quelation reaction to the tooth calcium provides adhesion to the tooth structure and the low molecular weight of the polyalkenoic acid provides sufficient biocompatibility for medium to deep cavities 3. Fluoride release was not considered a benefit in this case, since the remaining cavity floor was sufficiently hard at probing and there was no cariogenic challenge to fight against.
The restorative treatment was finished by confection of a composite resin restoration in the occlusal face of the tooth using a two-step etchand- rinse adhesive system. One of the limitations of glass ionomer cements as restorative materials is the low mechanical resistance when inserted in stress-baring areas. This behavior becomes clear when one considers the 7.2% annual failure rate of this material in stress-baring posterior restorations7. Comparatively, the 2.2% annual failure rate of composite restorations reinforces the indication of composite resins in posterior restorations 7. No clinical or radiographic symptom was observed at the 6-month or the 9-month follow-up, confirming the short-term success of the treatment.
The treatment prognosis relies on the size of the lesion when discovered and on the tooth maturation; these factors will determine whether it may compromise the pulp and the development of the root canal system.
Conclusion
Pre-eruptive intracoronal resorption is a rare condition. Therefore, dentists should be aware about its occurrence and examine carefully dental radiographs involving non-erupted teeth, since the early diagnosis is of utmost importance for determination of the treatment plan and prognosis.
References
1. Ari T. Management of "Hidden Caries": A case of severe pre-eruptive intracoronal resorption. J Can Dent Assoc. 2014;80:e59. [ Links ]
2. Davidovich E, Kreiner B, Peretz B. Treatment of severe pre-eruptive intracoronal resorption of a permanent second molar. Pediatr Dent. 2005 Jan-Feb;27(1):74-7.
3. Francisconi LF, Scaffa PMC, Barros VRSP, Coutinho M, Francisconi PAS. Glass ionomer cements and their role in the restoration of noncarious cervical lesions. J Appl Oral Sci. 2009 Sep-Oct;17(5):364-9.
4. Guinta JL, Kaplan MA. "Caries-like" dentin radiolucency of unerupted permanent tooth from developmental defects: case report. J Pedod. 1981 Spring;5(3):249-55.
5. Holan G, Eidelman E, Mass E. Pre-eruptive coronal resorption of permanent teeth: Report of three cases and their treatments. Pediatr Dent. 1994 Sep-Oct;16(5):373-7.
6. Klambani M, Lussi A, Ruf S. Radiolucent lesion of an unerupted mandibular molar. Am J Orthod Dentofacial Orthop. 2005 Jan;127(1):67-71.
7. Manhart J, Chen H, Hamm G, Hickel R. Buonocore memorial lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent. 2004 Sep-Oct;29(5):481-508.
8. Ozden B, Açikgoz A. Prevalence and characteristics of intra-coronal resorption in unerupted teeth in the permanent dentition: a retrospective study. Oral Radiology. 2009;25:6-13.
9. Seow WK, Hackley D. Pre-eruptive resorption of dentin in the primary and permanent dentitions: case reports and literature review. Pediatr Dent. 1996 Jan-Feb;18(1):67-71.
10. Seow WK, Lu PC, Mcallan LH. Prevalence of pre eruptive intracoronal dentin defects from panoramic radiographs. Pediatr Dent. 1999 Sep- Oct;21(6):332-9.
11. Seow WK, Wan A, Mcallan LH. The prevalence of pre-eruptive dentin radiolucencies in the permanent dentition. Pediatr Dent. 1999 Jan- Feb;21(1):26-33.
12. Seow WK. Diagnosis and management of unusual dental abscesses in children. Aust Dent J. 2003 Sep;48(3):156-68.
13. Seow WK. Multiple pre-eruptive intracoronal radiolucent lesions in the permanent dentition: case report. Pediatr Dent. 1998 May-Jun;20(3): 195-8.
14. Seow WK. Pre-eruptive intracoronal resorption as an entity of occult caries. Pediatr Dent. 2000 Sep-Oct;22(5):370-6.
15. Spierer WA, Fuks AB. Pre-eruptive intra-coronal resorption: controversies and treatment options. J Clin Pediatr Dent. 2014 Summer;38(4):326-8.
16. Uzun I, Gunduz K, Canitezer G, Avsever H, Orhan K. A retrospective analysis of prevalence and characteristics of pre-eruptive intracoronal resorption in unerupted teeth of the permanent dentition: a multicentre study. Int Endod J. 2014 Oct. [Epub ahead of print].
 Corresponding author:
Corresponding author:
Sinval Adalberto Rodrigues-Junior
Universidade Comunitária da Região de Chapecó
Área de Ciências da Saúde
Caixa postal 1141
Av. Senador Atílio Fontana, n. 591-E – Efapi
CEP 89809-000 – Chapecó – SC – Brasil
E-mail: rodriguesjunior.sa@unochapeco.edu.br
Received for publication: August 4, 2015
Accepted for publication: March 4, 2016













