Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.13 no.3 Joinville Jul./Set. 2016
ORIGINAL RESEARCH ARTICLE
Preemptive analgesia – evaluation of the effect of paracetamol and dipyrone after tooth whitening
Sandro Dias Rocha Mendes CarneiroI; Ana Julieta Almeida RodriguesI; Sarah Valentim DinizI; Danilo Lopes Ferreira LimaI; Fernando André Campos VianaI
I Dentistry Course, University of Fortaleza – Fortaleza – CE – Brazil
ABSTRACT
Objective: To evaluate the effect of preemptive analgesia of paracetamol and dipyrone in vital teeth professionally whitened in office. Material and methods: This was a pilot study of a blinded, paired sample, randomized clinical trial. Twenty volunteers requiring dental whitening, received, after the randomization, one of the formulations under study, one hour before the procedure: paracetamol 500 mg or dipyrone 500 mg as preemptive medications. Data collection was conducted by using two instruments: a record of research evaluation and visual analog scale (VAS), in which the patient was asked to score a value to the pain experienced before, during, 1 hour and 6 hours after the whitening procedure. Results: Most participants were female (75 %), of the age group between 18 and 27 years (75%). During the measurement of pain at pre- and trans-operative periods, VAS showed no statistically significant differences. At the post-operative period, immediately after, one and 6 hours after, clinically and statistically significant differences were observed, thus evidencing the superiority of treatment with Dipyrone 500 mg over the treatment with paracetamol 500 mg (p = 0.042, p = 0.003 and 0.0017, respectively). Conclusion: Dipyrone 500 mg exhibited higher effectiveness than Paracetamol 500 mg in the study population, as a technique of preemptive analgesia in tooth whitening procedure.
Keywords: preemptive analgesia; dipyrone; paracetamol; tooth whitening.
Introduction
The new esthetic pattern is white, wellcontoured, well-aligned teeth 17. Alterations in appearance may affect the psychological and social behavior of the humans. The changes may range from the problem camouflage to the total individual's introversion. Consequently, the search for tooth whitening is increasing; tooth whitening is a safe and effective procedure providing good esthetic outcomes within its limitations and indications 3. Currently, the main tooth whitening agents used are carbamide peroxide and hydrogen peroxide, at different concentrations 13.
The sensitivity after the whitening of vital teeth has been considered the main side effect of this procedure 5. Generally, the pain reported in most of the studies is transitory and disappears just after the treatment or some days later. Moreover, tooth sensitivity intensively differs among individuals. The mechanism involved in sensitivity after tooth whitening is still not fully understood; but the hydrodynamic theory is the most accepted hypothesis to explain the sensitivity occurrence. Currently, the hypothesis that the whitening gel application on the tooth may directly activate the nerves inside the pulp, which is mediated by the gel components and would be related to post-whitening sensitivity 15.
The great variety of drugs available in the market and the knowledge in Pharmacology would help the dentists provide comfort and demystifying the pain and fear of dental treatment. An adjuvant therapy is the preemptive analgesia, which is a drug regimen prior to the nociceptive stimulus, aiming at preventing hyperalgesia and the subsequent pain amplification 1. The term "preemptive" means to eliminate the problem before the appearance. The concept behind this idea is based on the fact that the nociceptive fiber stimulation promotes neural and behavioral changes that may persist after the ending of the noxious stimulus. This posttraumatic pain may be the result of changes in the peripheral (hyperalgesia) or central nervous system (hyperexcitability) 18.
In Dentistry, three drug groups are commonly employed to control pain: local anesthetics, nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids, and analgesic drugs of central and/or peripheral action 14. The use of dipyrone to control pain in dental treatment is based on the diverse mechanism with little effect on the gastrointestinal tract and blood coagulation 16. Rockemann et al. 19 demonstrated that dipyrone use prior to surgical incision reduces the consumption of morphine per hour, evaluated through the method of analgesia controlled by the patient. This highlights the preemptive effectiveness of dipyrone and the possible effect on central sensitization. Despite of the many behavioral, neurochemical, and electric-physiological studies, the analgesic mechanism of dipyrone is still not fully clarified and it is believed that the effect is on the level of the peripheral and central system, as well as on different levels of pain processing 21. The analgesia and anti-inflammatory effects of dipyrone are different from those of the corticosteroids, because dipyrone blocks COX 1 and 2, while the latter block Phospholipase A2. The analgesia provided by dipyrone depends on the peripheral (prostaglandins and nitrous oxide) and central effect (peptidergic and serotonergic synergism and glutamatergic antagonism) 2.
Paracetamol is a drug with analgesic properties, but without clinically significant antiinflammatory properties. With antipyretic action, paracetamol is considered an alternative in cases of hypersensitivity to acetylsalicylic acid. Paracetamol inhibits the arachidonic acid cascade, preventing the synthesis of tissue prostaglandins; and minimally of central action, it inhibits the pro-inflammatory cell mediators accounting for inflammation, such as pain appearance. Currently, paracetamol is one of the most used analgesic drug, but it is highly hepatotoxic and the daily dose should not exceed 4,000 (8 tablets of 500 mg) 12.
This study aimed to evaluate the effect of preemptive analgesia of paracetamol and dipyrone on vital teeth submitted to in-office whitening.
Material and methods
This study was submitted and approved by the Institutional Review Board regarding ethical aspects (protocol #45/12).
This was a pilot study of a blinded, paired sample, randomized clinical trial on the use of pre-operative medication with either paracetamol 500 mg or dipyrone 500 mg. Twenty volunteers were randomly divided into the final sample of 40 hemiarches. The method to determine which the two drugs would be used first was raffle associated with randomization, which enabled that this happened at random and without any interference from the examiner.
All patients had the esthetic indication for tooth whitening. The sample selection was directed to a planning that comprised tooth whitening procedure at two steps, that is, one hemiarch per time, enabling the use of the two tested drugs, after wash out period. The inclusion criteria were: patients aged above 18 years, without esthetic restorations on the anterior teeth, without any report of tooth hypersensitivity and periodontal problems, without allergy to the tested drugs.
Data collection was accomplished by to instruments: identification form and visual analogic scale (VAS). VAS is composed of a line scored from 0 to 10. The patient should score a value to the pain experienced before, during, just after, and one and six hours after the tooth whitening procedure.
We also quantified the rescue medication, that is, the negative of antalgic effect and the need of using different drugs from those of the study. The rescue medication measurement consisted of a 0-cm line with anchors on the endings. One anchor is marked with "no pain"; the other ending is marked with "the worst pain possible", or similar phrases. According to Sousa and Silva 21, this is a sensible, simple, reproducible, and universal instrument that could be understood in different situations even with cultural and language differences between the examiner and the patient. These authors 21 also observed the line position (horizontal or vertical) of the scale. Patients with low back pain have understood the line as their cervical spine consequently marking the line on the same position of their pain, instead of scoring the pain intensity. Notwithstanding, the same authors reported the increasing evidence of the reliability of this method 21.
At the first clinical period, according to the raffle and randomization, the volunteer used either dipyrone 500 mg or paracetamol 500 mg (Farmácias Pague Menos), one hour before the procedure. Accordingly, if the volunteer took paracetamol as preemptive drug at the first appointment, at the second appointment he/she took dipyrone, and vice versa.
The whitening procedure followed the manufacturer's instructions. All volunteers were treated at the same clinical environment, without the direct dental chair light. The whitening agent Whiteness HP Maxx (Dentscare Ltda., Joinville, SC), com had the expiration date until November, 2014. The first appointment comprised the three applications of the whitening agent on the right maxillary hemiarch, for 15 minutes each, followed by photoactivation (Gnatus) for 2 minutes, and washing. At the second appointment (48 hours later), the same procedure was repeated on the left maxillary hemiarch.
Descriptive analysis obtained the absolute, percentage, and mean values. ANOVA was used to analyze the data with level of significance of 5.0% (0.05). All data was analyzed by Bioestat 5.3 software for Windows.
Results
The sample comprised 20 volunteers selected according to the inclusion and exclusion criteria and submitted to prior medication with dipyrone 500 mg and paracetamol 500 mg, at alternated inoffice whitening, between March and April, 2013. Of the 20 volunteers, 70% (n=14) were female and 30% (n=6) were male.
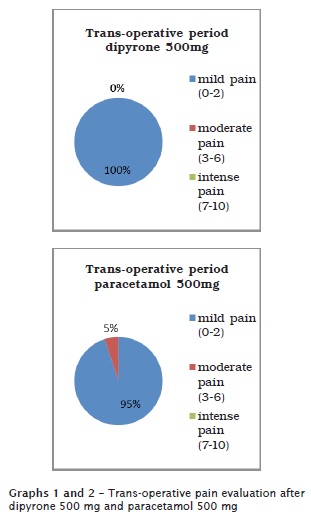
All volunteers, at the two appointments, did not have spontaneous pain prior to the inclusion and tooth whitening, according to VAS. The analysis of preemptive analgesia trans-operative effectiveness, 100% (n=20) of the volunteers who took dipyrone 500 mg only reported mild pain; 95% (n=19) of the volunteers who took paracetamol 500 mg reported mild pain and 5% (n=1) intense pain, but without statistically significant differences (graphs 1 and 2).
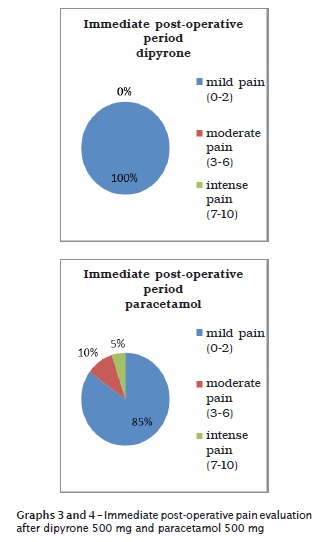
After all post-operative period, preemptive analgesia with dipyrone 500 mg was higher than that of paracetamol 500 mg, with statistically significant differences. Just after the ending of tooth whitening, 17 volunteers had mild pain, two had moderate pain, and one had intense pain, after taking paracetamol. After dipyrone use, all volunteers had mild pain, showing the superiority of the pirazolonic- derived drug (p = 0.042) (graphs 3 and 4).
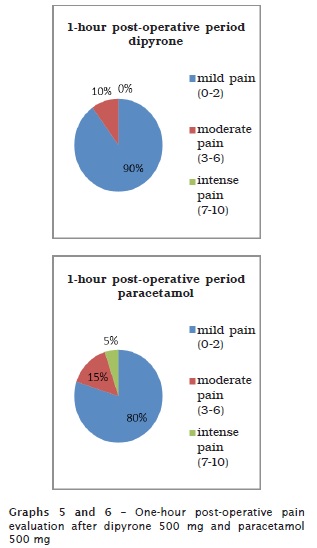
Maximum (n = 01) and moderate (n = 03) pain scores were reported for paracetamol group, one hour after the appointment. At this same period, the volunteers taking dipyrone reported moderate pain (n = 02) and mild pain (n = 18) with statistically significant differences (p = 0.003) (graphs 5 and 6).
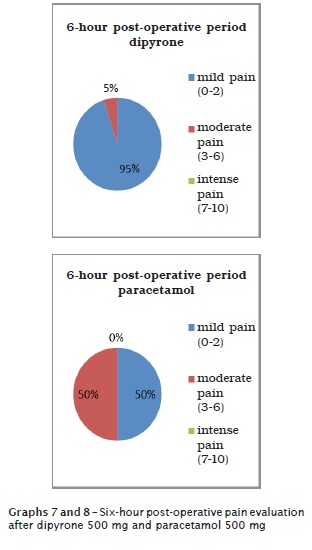
Six hours after the drugs' use, the effectiveness decrease is already expected because of the phenomena of metabolizing and elimination. Only one volunteer reported moderate pain after taking dipyrone and the others reported mild pain. For paracetamol, ten volunteers reported moderated pain and ten mild pain, with statistically significant differences (p = 0.0017) (graphs 7 and 8).
Discussion
The results of this present study match those of Queiroz et al. 16, who evaluated the analgesic effectiveness of dipyrone 500 mg and paracetamol 500 mg to treat post-operative pain after the extraction of included third molars; dipyrone showed a better post-operative effectiveness.
Similar outcomes were reported by Lacerda 12, who clinically compared the analgesic action of dipyrone 500 mg and paracetamol 750 mg after the installation of dental implants. Again, dipyrone showed higher effectiveness than paracetamol.
On the other hand, the results of this present study were different from those found by Gurgel and Noronha 10, who tested dipyrone, paracetamol, Lysine clonixinate to control the post-operative pain after the extraction of included third molars. These authors did not find statistically significant differences in the post-operative pain scores among the groups and between genders.
Conclusion
The use of dipyrone 500 mg significantly reduced the pain after tooth whitening compared to paracetamol 500 mg. Dipyrone has an analgesic action on pain of dental nature. With the use of preemptive analgesia with dipyrone, we observed an improvement in the whitening procedure quality, because the pain level after the procedure reduced or even stopped in some cases.
References
1. Aida S, Baba H, Yamakura T. The effectiveness of preemptive analgesia varies according to the type of surgery: a randomized, double-blind study. Anesth Analg. 1999;89:711-6. [ Links ]
2. Andrade ED. Terapêutica medicamentosa em odontologia. 2. ed. Artes Médicas; 2006.
3. Baratieri LN, Monteiro Jr S, Andrada MAC, Vieira LCC. Clareamento Dental. 1993;4: 89-136.
4. Brasil. Ministério da Saúde, Agência Nacional de Vigilância Sanitária. ANVISA "P I D" 3 4 j 2001. Brasília: Ministério da Saúde; 2001.
5. Costa CAS, Ribeiro A, Dias P, Sacono NT. Clareamento dentário: princípios e efeitos biológicos. Rev Assoc Paul Cir Dent. 2010;(1):68-77.
6. Daftary SN. A controlled comparison of dipyrone and paracetamol in post-episiostomy pain. Curr Med Res Opin. 1980;6:614-8.
7. De Lacerda JT, Simionato EM, Peres KG, Peres MA, Traebert J, Marcenes W. Dor de origem dental como motivo de consulta odontológica em uma população adulta. Rev Saúde Pública. 2004;38(3):453-8.
8. Fernandes CET, Koslowsky JRV. Avaliação da eficácia analgésica da dipirona sódica versus paracetamol e cloridrato de benzidamida no tratamento da dor pós-operatória em cirurgia odontológica. Amb Odontol. 1995;24:15-9.
9. Goodman AG. As bases farmacológicas da terapêutica. 8. ed. Rio de Janeiro: Guanabara Koogan; 1991.
10. Gurgel GS, Noronha VRAS. Avaliação da ação analgésica do clonixinato de lisina em comparação com o paracetamol e dipirona em cirurgia de dentes inclusos: estudo clínico duplo cedo randomizado. Monografia. Belo Horizonte.
11. Hadzic A. Textbook of Regional Anesthesia and Acute Pain Management. 2007.
12. Lacerda EJR. Comparação clínica da ação analgésica da dipirona e paracetamol em cirurgia de instalação de implantes odontológicos. Campinas; 2009.
13. Minoux M, Serfaty R. Vital tooth bleaching: biologic adverse effects – a review. Quintessence Int. 2008;39:645-59.
14. Neidle EE, Yagiela JA. Farmacologia e terapêutica para dentistas. 4. ed. 2000.
15. Pinheiro MLP, Taminato RL, Moreira A, Andrade ED. Analgesia preemptiva em odontologia. Braz J Oral Sci. 2004;3(10).
16. Queiroz TP, Santos PL, Esteves JC, Stellin GM, Shimuzi AS, Betoni Junior W et al. Dipirona versus paracetamol no controle da dor pós-operatória. Revista de Odontologia da UNESP. 2013:78-82.
17. Rheinheimer L. Sensibilidade no clareamento dental. Passo Fundo; 2008.
18. Rocha RG, Tortamano N, Adde CA, Simone JL, Perez FEG. O controle da dor em odontologia através da terapêutica medicamentosa. In: Anais do 15. Conclave Odontológico Internacional de Campinas; 2003 Mar/Apr; Campinas.
19. Rockemann MG, Seeling W, Bischof C. Prophylatic use of epidural mepivacaine/morphine: systemic diclofenac and metamizole reduces postoperative morphine consumption after major abdominal surgery. Anesthesiology. 1996:1027- 34.
20. Scott DS, Hirchman R. Psycological aspects of dental anxiety in adults. Journal of the American Dental Association. 2008;104:27-31.
21. Sousa FF, Silva JA. A métrica da dor (dormetria): problemas teóricos e metodológicos. Revista DOR. 2005;6(1):469-513.
 Corresponding author:
Corresponding author:
Sandro Dias Rocha Mendes Carneiro
Av. Antonio Sales, n. 3.525, apto 1801
Dionísio Torres
CEP 60135-102
Fortaleza – CE – Brasil
E-mail: sandrodiasr@hotmail.com
Received for publication: May 13, 2016
Accepted for publication: June 8, 2016













