Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.13 no.4 Joinville Out./Dez. 2016
ORIGINAL RESEARCH ARTICLE
Epidemiological profile of ameloblastoma at Erasto Gaertner Hospital
Daniela Cristina LunelliI; Fernando Luiz ZanferrariI; Juliana Lucena SchusselI; Laurindo Moacir SassiI; Sérgio Ossamu IoshiiII
I Department of Oral and Maxillofacial Surgery, Erasto Gaertner Hospital – Curitiba – PR – Brazil
II Department of Pathology, Erasto Gaertner Hospital – Curitiba – PR – Brazil
ABSTRACT
Introduction: Ameloblastoma is the most common benign tumor of odontogenic origin, and represents about 11% of all odontogenic tumors. It is characterized by being locally aggressive and having high recurrence rates. Objective: To evaluate the occurrence of ameloblastoma in the Erasto Gaertner Hospital in patients from 1972 to 2012. In addition, to assess the main treatments, the most prevalent histological variants, the recurrence rate, the anatomical location of the lesion and patient profile. Material and methods: A retrospective study of patients diagnosed with ameloblastoma at the Erasto Gaertner Hospital between the years 1972-2012 was performed. Epidemiological data were collected such as gender, age, race, lesion location, type of surgical procedure, follow-up and recurrence rate; and analyzed using descriptive statistics. Results: A total of 40 patients were selected for the study. The most affected age group was between the third and fifth decade of life, with 19 cases (47.5%), followed by the second and fourth decade, with 14 cases (35%); the sixth decade, with 5 cases (12.5%) and seventh decade with 1 case (2.5%). The patients' ages ranged from 13 to 66 years, with an average age 34.9 years. The mandible was the most affected site, with 38 cases (95%) of cases, and maxilla had only 2 cases (5%). Thirty-eight patients were treated with radical surgery and 5 patients presented recurrence after 1 year of follow-up. Both cases that occurred in maxilla presented recurrence. Conclusion: Recurrence of ameloblastoma decreases significantly when surgery is performed properly, with wide excision and margin. Combination of full tumor resection and reconstruction was the best approach observed in this study. In addition, we recommend a long period of clinical and radiographic follow-up.
Keywords: ameloblastoma; jaw; odontogenic tumors.
Introduction
The ameloblastoma is the most common benign tumor of epithelial odontogenic origin, and represents about 11% of all odontogenic tumors 3. It originates from epithelial remnants of intra and/or extra-osseous location 6. Characterized by slow and painless swelling is often diagnosed due to increased local volume or by means of routine radiographs 11.
Radiographically it can appear as unilocular or multilocular radiolucent images, with bone erosion. It may be associated with impacted teeth and cause radicular resorption 19. The most frequent location is posterior mandible, but it is rarely found in the maxilla, where the prognosis is much worse due to increased infiltration of trabecular bone and anatomic location 4. The peak incidence occurs at the third and fourth decades of life with equal gender distribution 14.
The high recurrence rates remain problematic, and several factors have been identified, such as clinicopathologic variant and anatomical location 12. The occurrence in maxilla, due bone porosity, facilitates the spread of the tumor 4, that behaves more aggressively than in the mandible 2.
Treatment for ameloblastoma may be conservative or radical. The conservative technique includes enucleation and/or curettage. The radical treatment includes partial or marginal resection associated with chemical (Carnoy's solution) or thermal (cryotherapy)adjuvant treatment.
While conservative therapies may be presented as less morbid for patients, there are increased risk of recurrence in such treatment. For that reason, radical treatments have lower rates of recurrence and constitute the vast majority of cases 15, but this choice often requires bone reconstruction to restore function and aesthetics 24.
The aim of this study was to establish an epidemiological profile of ameloblastoma in the hospital, between the years of 1972 and 2012, assess the main treatments, the relapse rate, anatomic location of the lesion, and the patient's profile.
Material and methods
A retrospective study was conducted with patients with diagnosis of ameloblastoma referred to the Service of Oral and Maxillofacial Surgery of the Erasto Gaertner Hospital between the years of 1972-2012. Epidemiological data were collected such as gender, age, race, lesion location, type of surgical procedure, follow-up and recurrence rate. The study excluded patients with follow-up less than 12 months.
Results
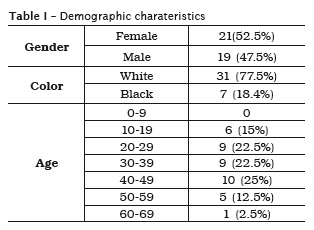
Between the years of 1972 and 2012, 54 patients were diagnosed with ameloblastoma. Fourteen patients were excluded because they had a follow-up lower than 12 months. From the 40 cases included in the study, 52.5% were women and 47.5% were men between the second and seventh decade of life. The patients' ages ranged from 13 to 66 years, with an average age of 34.9 years (table I). Most patients were white (77.5%) and the most frequent site was the posterior region of the mandible (90%). Maxilla presented only 2 cases (5%), both in posterior region.
Forty-four patients had larger lesions with large involvement of the mandible region: body and angle (15.8%), body and ramus (18.4%), symphysis and body (5.3%), symphysis and ramus (2.6%); and one case with involvement of the right and left side of the mandible (2.6%) (table II).
All patients underwent surgical treatment, 38 (95%) were subjected to a surgical treatment in the mandible, with resection of the lesion with peripheral osteotomy and 2 cases (5%) underwent surgery in the maxilla. The mandibular reconstruction, when indicated, was performed with microvascular fibular graft or iliac crest bone graft.
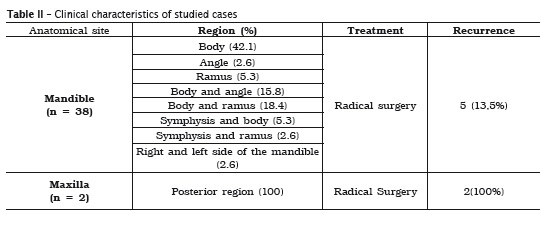
Five patients presented recurrence in the mandible, and both cases that occurred in the maxilla also relapsed. The time for recurrence ranged from 10 months to 9 years, with a mean of 5.11 years. One patient, who had ameloblastoma in the maxilla, died from aggressiveness of the tumor and complications of the treatment.
Discussion
The ameloblastoma is a benign tumor, locally aggressive, with odontogenic origin 25. Most patients have between 30 and 60 years at time of diagnosis. Clinically, it is characterized by slow growth, painless enlargement and expansion involving the maxillary bones, leading to a facial deformity 18. There is no predilection for sex 9. In the present study gender distribution showed no preferences, as most reports in literature 1,6-8,21.
The location of the tumor is related to the individual's ethnicity, with the posterior region most frequently involved in Caucasian and Japanese; while in black, especially those of African origin, the anterior region is most common site of the disease 16. This study had a high prevalence of white individuals.
Our study has identified that the mandible was the most affected site, posterior region with 36 cases (90%), the anterior with 2 cases (5%), which is in agreement with almost studies 4,6,8,17.
The ameloblastoma is an odontogenic tumor with a strong tendency to recurrence after treatment 20. There are many treatment protocols, the most appropriate being surgery. Cryotherapy, radiotherapy and chemotherapy are also reported, although the effectiveness of these procedures have not been established by controlled studies. Ameloblastomas inadequately treated enables greater chance of relapse 26.
It is believed that the recurrence rate is related to many factors such as tumor subtype, methods of treatment and tumor behavior 5. Nakamura et al. compared the long-term results of 78 cases of ameloblastoma, obtained a recurrence rate of 7.1% after radical surgery and 33.3% after conservative treatment. They recommended wide jaw resection as the best treatment for ameloblastoma 13. Our study had a 17.5% recurrence rate after radical surgical treatment.
Sassi et al. 24 evaluated 43 patients, 31 who had no previous treatment were submitted to surgical treatment with a recurrence rate of 4 (13%) of cases. Of those who relapsed, 2 performed only partial resection, 1 curettage and cryotherapy; and 1 wide resection. Lower recurrence rate is observed with radical surgical treatment.
According to Doenja Hertog et al.. 10 all pat ients in whom preoperative diagnosis of ameloblastoma was available were advised to radical surgery. However, in the 28 patients who were treated by enucleation, the recurrence rate reached about 60% over a mean follow-up of 8.3 years.
The reconstruction of large defects, caused by radical surgery with microvascular fibular graft favors patient in functional, aesthetic aspects for fast reintegration into society and minimize psychological effects arising from surgery 22.
Sassi et al..23 confirmed the successful outcome of the functional rehabilitation of the stomatognathic system with titanium cylinder implants in microvascular fibular graft for reconstruction of mandible.
Ameloblastomas have a greater tendency to relapse when surgery is not performed properly, with wide excision and margin of safety, thus, its treatment requires full resection with broad safety margin and immediate reconstruction whenever possible. The microvascular fibular graft is a good alternative for reconstruction of segments or even entire jaw, which restores the function, the aesthetics of the stomatognathic system, and allow implant-prosthetic rehabilitation. In addition, it is recommended that a long period of clinical and radiographic follow-up, because recurrence may occur after a long period after treatment.
References
1. Anjos ED, Andrade ESS, Pinto LP, Souza LB. Estudo clínico-patológico de ameloblastomas: an á l i se de c asos. Rev Bras Odon t o l . 2003;60(4):224-8. [ Links ]
2. Barnes L, Eveson JW, Reichart P, Sidransky D. Pathology & genetics: head and neck tumours. World Health Organization Classification of Tumours; 2005.
3. Barros SSLV, Freitas RA, Galvão HC, Souza LB. Avaliação imuno-histoquímica do antígeno nuclear de proliferação celular (pcna) e da proteína p53 em ameloblastomas tratados pela técnica da marsupialização. Ciênc Odontol Bras. 2006;9(1):32-7.
4. Bueno JM, Bueno SM, Romero JP, Atín MSB, Redecilla P, Martin GR. Mandibular ameloblastoma. Reconstruction with iliac crest graft and implants. Med Oral Patol Oral Cir Bucal. 2007;12:73-5.
5. Siar CH, Lau SH, Han K. Ameloblastoma of the jaws: a retrospective analysis of 340 cases in a Malaysian population. J Oral Maxillofac Surg 2012; (70):608-615.
6. Costa DOP, Ecard MB, Oliveira SP, Silva LE. Estudo retrospectivo dos casos diagnosticados como ameloblastoma no Serviço de Anatomia Patológica do Hospital Universitário Antônio Pedro entre 1997 e 2007. J Bras Patol Med Lab. 2008;44(6):441-7.
7. Costa C, Pereira FM, Mailart D, Panella J. Aspectos radiográficos de um caso de ameloblastoma. RPG Rev Pós-Grad. 1994;1(2):28-30.
8. Dhanuthai K, Chantarangsu S, Rojanawatsirivej S, Phattarataratip E, Darling M, Boeters LJ et al.. Ameloblastoma: a multicentric study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(6):782-8.
9. Hertog D. Histopathology of ameloblastoma of the jaws; some critical observations based on a 40 years single institution experience. Med Oral Patol Oral Cir Bucal. 2012 Jan;17(1):76-82.
10. Hertog D, Waal IVD. Ameloblastoma of the jaws: a critical reappraisal based on a 40-years single institution experience. Oral Oncology. 2010;(46):61-4.
11. Jaber KY, Sassi LM, Franzi AS. Tratamento de ameloblastoma. Rev Bras Cir Cabeça Pescoço. 2009;38(2):124-8.
12. Mendonça JCG, Pagliarelli PRS, Bento LA, Oliveira JGP, Benaglia MB, Santos AA. Ameloblastoma letal de maxila: relato de caso. Rev Bras Cir Craniomaxilofacial. 2009;12(2):85-8.
13. Nakamura N, Higuchi Y, Mitsuyasu T, Sandra F, Ohishi M. Comparisonof long-term results between different approaches to ameloblastoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(1):13-20.
14. Oteri G, Ponte SF, Pisano M, Cicciú M. Fiveyear follow-up of implant-prosthetic rehabilitation on a patient after mandibular ameloblastoma removal and ridge reconstruction by fibula graft and bone distraction. Dental Research Journal. 2012;9:2.
15. Paiva LCA, Santos MESM, Silva DN, Heitz C, Sant'Ana Filho M. Potencial de recidiva do ameloblastoma: relato de caso. Rev Cir Traumatol Buco-maxilo-facial. 2010;10(1):27-34.
16. Pereira FAC, Melo LA, Gurgel CAS, Cangussu MCT, Azevedo RA, Santos JN. Clinicopathological and demographic characteristics of ameloblastomas in a population from Bahia, Brazil. Rev Odonto Ciênc. 2010;25(3):250-5.
17. Rastogi V, Pandilwar PK, Maitra S. Ameloblastoma: an evidence based study. J Maxillofac Oral Surg. 2010;9(2):173-7.
18. Raldi FV, Guimarães Filho R, Moraes MB, Neves ACC. Tratamento de ameloblastoma. RGO. 2010;58(1):123-6.
19. Regezi JA, Sciubba JJ. Patologia bucal, correlações clínico-patológicas. Rio de Janeiro: Guanabara Koogan; 1991.
20. Sammartino G, Zarrelli C, Urciuolo V. Effectiveness of a new decisional algorithm in managing mandibular ameloblastomas: a 10- years experience. Br J Oral Maxillofac Surg. 2007;(45):306.
21. Santos, JN, Pinto L, Figueiredo CRLV, Souza LB. Odontogenic tumors: analysis of 127 cases. Pesqui Odontol Bras. 2001;15(4):308-13.
22. Sassi LM, Dissenha JL, Simette RL, Rodrigues E, Silva AB, Pedruzzi PAG et al.. Reconstrução com enxerto microvascularizado de fíbula em mandíbula com duplo segmento em porção anterior em edentados, variante – I. Rev Brasileira de Cirurgia de Cabeça e Pescoço. 2005;34(1):37-41.
23. Sassi LM, Oliveira BV, Radaelli RL, Rodrigues E, Silva AB, Ramos GHA. Oral rehabilitation post mandible tumor excision with titanium osseointegrated implants in a microvascularised fíbula graft. Int J Oral Maxillofac Surg. 2001;30(suppl A):S15.
24. Sassi LM, Ramos GHE, Calderari GT, Biazolla ER, Freitas SEM, Oliveira BV. Ameloblastoma: análise de 43 casos. Revista Brasileira de Cirurgia e Implantodontia. 2001;8.
25. Shakya H, Khare V, Pardhe N, Mathur E, Chouhan M. Basal cell ameloblastoma of mandible: a rare case report with review. Case Reports in Dentistry. 2013;2013.
26. Silva BF, dos Santos Júnior JF, Abrahão M, Cervantes O, Miranda SL. Ameloblastoma: revisão de literatura. Revista Brasileira de Cirurgia de Cabeça e Pescoço. 2004;33:1.
 Corresponding author:
Corresponding author:
Daniela Cristina Lunelli
Rua Espanha, n. 97, apto 301 – Das Nações
CEP 89130-000 – Indaial – SC – Brasil
E-mail: daniela_lunelli@hotmail.com
Received for publication: June 17, 2016
Accepted for publication: August 24, 2016













