Services on Demand
Article
Related links
Share
RSBO (Online)
On-line version ISSN 1984-5685
RSBO (Online) vol.13 n.4 Joinville Oct./Dec. 2016
CASE REPORT ARTICLE
How to avoid legal problems in cases of nerve injury due to dental implants
Talita Lima de CastroI; Mário Marques FernandesII; Renato Oliveira RosaIII; Rogério Nogueira de OliveiraIV; Eduardo Daruge JúniorV
I Department of Morphology, Anatomy Division, Piracicaba Dental School, University of Campinas – Piracicaba – SP – Brazil
II Public Prosecution of Rio Grande do Sul State – Porto Alegre – RG – Brazil
III Department of Prosthodontics, Dental School, Pontifical Catholic University of Rio Grande do Sul – Porto Alegre – RS – Brazil
IV Department of Social Odontology, Forensic Dentistry Division, Dental School, University of São Paulo – São Paulo – SP – Brazil
V Department of Social Odontology, Forensic Dentistry Division, Piracicaba Dental School, University of Campinas – Piracicaba – SP – Brazil
ABSTRACT
Introduction: During the surgical and implant procedures, there is considerable risk of injury to oral nerves. The dental surgeon must recognize clinical signs of the main nerve lesions that might occur following surgical or dental implant procedures, and take the necessary precautions to prevent them. Objective: The aim of this manuscript was to describe a legal case of clinical paresthesia due to alveolar nerve compression following an implant placement, revising the types of nerve lesions of surgical-implant etiology, and advise the dental professional against clinical and legal flaws.Case report: In this case, a female patient underwent oral rehabilitation, including the placement of an osseointegrated implant in the lower left first molar region. After the setting of the device, the patient presented paresthesia on the left mentonian region and buccal mucosa of elements 34, 33 and 32 and, dissatisfied with the situation, she appealed to justice and requested the responsibility of the professional. Conclusion: It is important to discuss that prevention continues to be the key issue when it comes to avoiding clinical, ethical or legal repercussions. Practicing adequate diagnosis and treatment planning and conducting the necessary complementary exams are essential, allied to previously patients' signed consent.
Keywords: nervous system trauma; dental implantation; forensic dentistry.
Introduction
Although surgical and dental implant techniques are usually precise and predictable, the risk of complications and failure should always be considered by the clinician. The contact or damage to nervous fibers is common due to the proximity of such structures to the oral surgeon´s field of work. Nerve lesions are characterized by injury to the neural structure caused by any type of trauma, resulting in failure to transmit nervous impulses, yielding temporary or permanent symptoms 7.
Such injuries might result in malpractice lawsuits against the dental surgeon, since the responsibility of the dentist during dental services is associated to several obligations at all stages of treatment, including correct indication of the surgery, treatment plan, patient orientation and professional conduct during treatment and after the occurrence of any complication 4,15.
The dental surgeon must recognize clinical signs of the main nerve lesions that might occur following surgical or dental implant procedures, and take the necessary precautions to prevent them. Therefore, the aim of this manuscript is to describe a legal case of clinical paresthesia due to alveolar nerve compression following an implant placement, revising the types of nerve lesions of surgical-implant etiology, and advise the dental professional against clinical and legal flaws.
Case report
This study was submitted and approved by the Ethical Research Committee of the Piracicaba Dental School (UNICAMP), adhering to ethical standards.
The present case describes a 64-year old white female, smoker, who underwent oral rehabilitation, including the placement of an osseointegrated implant. During treatment planning, clinical and image examinations were performed, including a CBCT-scan, and a two-millimeter safety margin was predicted. The patient signed an informed consent giving awareness of the associated risks inherent to the procedure.
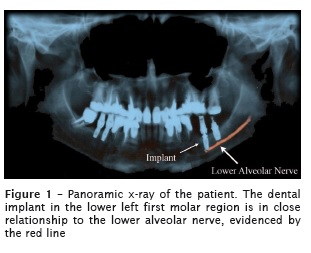
After implant placement in the lower left first molar region, the patient presented paresthesia on the left mentonian region and buccal mucosa of elements 34, 33 and 32. The implantodontist began clinical follow-up, and after a radiographic exam, close relation was perceived between implant and lower alveolar nerve (figure 1), supposedly compressed by the device positioned on that site.
The surgeon in charge recommended the implant removal, but the patient was resistant towards another surgical intervention and then she sought the legal system, filing for malpractice. The patient required a dental forensic examination to anticipate proof, as well as a neurological report, which identified possible nerve compression by a foreign body. Patient demanded payout of approximately R$ 73.000,00 Brazilian Reais for moral and material losses.
During litigation, all consulted experts and the legal examiner identified implant removal as the only option to resolve the paresthesia, although the plaintiff, despite being oriented and having signed an informed consent, chose not to remove it, maintaining the cause of nerve injury. Over the litigation process, the judge thus understood the plaintiff became responsible for the cause-in-fact, because the problem could have been resolved if she had not opted to maintain the dental implant. Case was dismissed on the basis that claim could not be granted due exclusively to victim's fault. After review in a court of appeal, sentence was maintained and patient's claim was denied.
Discussion
One of the most commonly used classifications of nerve injuries is Seddon's 14, which divides them into three different degrees: neurotmesis, axonotmesis, and neurapraxia. The first of them, neurotmesis, refers to the interruption or separation of the completely severed nerve. This injury leads to complete lesion, with sensorial loss or motor paralysis, making nerve regeneration difficult, below ideal or unlikely to occur. Axonotmesis occurs after nervous fiber injury, especially by crushing, resulting in loss of endoneurium's continuity, the connective layer involving the axon, but the nerve is not completely divided, preserving some tissue continuity. In turn, neurapraxia is the term used to describe a short-term paralysis, associated to a local block of nervous impulse, resulting in motor or sensorial deficiency. In this case, nerve´s structure remains intact, but axon conduction is interrupted. It is caused by a lesion or compression that does not divide the nervous structures, usually of low intensity. Recovery is usually fast, can be safely foreseen if the exam confirms this syndrome, but the rehabilitation process is irregular.
Nerve damage produces characteristic aspects and can hamper the individual, considering the remarkable precision of oral sensitivity. Paresthesia, anesthesia, and hypoesthesia are symptoms frequently related to traumatic lesion of sensory nerves present in the oral cavity, after surgical or dental implant procedures. The most common symptom, paresthesia, identified by scratching, numbness and pricking, is present in 70 to 73% of patients with a permanent nerve injury. Anesthesia and hypoesthesia are present in more than half the patients who underwent some sort of nervous lesion in lip or tongue, and one in five patients refer pain in the affected area. In almost all cases, injuries are unilateral 13.
Recovery from nerve damage depends on the type and etiology of the lesion, and can be either be spontaneous or result from micro neurosurgical anastomosis or through decompression techniques, which should only be attempted at least four months after clinical follow-up, since the rate of recovery is faster in the first six months after the injury 7. When spontaneous recovery is witnessed, symptoms of nerve compression seem to diminish after approximately 4 to 6 months, and of nerve severing, after around 8 months 12.
However, in cases such as nerve compression, dental implant removal should be indicated. This aims to guarantee local tissue recovery and nervous regeneration, by removing the cause to the problem 5. This situation often increases patient´s dissatisfaction with the dentist, affecting the patient-professional relationship.
It is important to know that a great percentage of sensorial alterations can be avoided if the dentist in charge carries out an adequate, individualized treatment plan, starting from a specific anamnesis associated to radiographic exams, that shows a view of the region and its adjacent structures, as well as to install dental implants with adequate length, in the appropriate position and location 17. The performance of correct diagnosis and planning, based on current scientific evidence, decreases the number of interventions, reducing the risk of sequelae to soft and hard tissues 1. Following rigid criteria, the professional can offer excellent results with minimal risk of damage to the nerves present in the oral cavity.
The informed consent is fundamental, especially in implantology, and must contain all the peculiarities inherent to each clinical case, including the clarification of risks, benefits and alternatives of treatment being proposed 11.
As a safeguard, the dental implant professional should keep all patient records under ethical and legal precepts, which includes clinical examination and anamnesis files, image records (X-rays and CT-scans), treatment plan previous to the surgical procedure and signed by the patient, informed consent, and finally, a dental service contract, important especially in complex and extensive procedures 9.
Bartling et al..2 advise that a functional evaluation of the mandibular nerve should be carried out, as well as of other related nerves, previously to dental implant placement, in order to account for any preexisting condition, thus avoiding complaints against the dentist for preceding problems. Authors also alert that when planning dental implant placement in the posterior region of the mandible, radiographic identification of the mandibular canal is mandatory. For similar reasons, the anatomy of the mentonian nerve should be considered while determining implant position in the anterior portion of the mandible.
Some measures should be taken whenever faced with a complication during a surgical procedure. The treatment protocol to be adopted in case of paresthesia is patient follow-up during the first four weeks after the procedure, and then every six months until two years are complete. A large number of patients recover, referring no symptoms at the end of this period 8,16.
Patients with persisting paresthesia after a two-year period are considered with permanent nerve damage. They are submitted to an additional X-ray to evaluate the integrity of the mandibular canal (lower alveolar nerve) and surgical exploring with decompression or nerve reparation are considered 8.
However, there are cases of nerve compression where recovery is unlikely until the dental implant is not removed from its intimate relation to the nerve. Elian et al.. 5 recommend implant removal in such cases, from the moment the symptoms are identified, in order to guarantee the return of sensitivity. The authors describe the case of a patient who presented sensorial alterations for 4 years and 5 months, without signs of improvement. After an evaluation, it was decided that implant should be removed, resulting in significant recovery even after such a long-time lapse since the initial injury. Therefore, when images evidence intimate contact between the implant and the nerve, the device should be removed, preferably in an atraumatic manner, being lightly luxated and removed with forceps to avoid further damage to adjacent nervous 5,10.
Another aspect that should be highlighted is patient notification on the occurrence. Any professional of the field can be faced with dental implant complications, and patients should be aware of this risk. Informing it previously avoids complaints and malpractice lawsuits during treatment. Patient should be notified of the inherent risks and possibilities of failure, and post-operative instructions should be revised in every case, as a means of avoiding such consequences, keeping physical records of such notifications 4.
It is wise to remember that dental implant treatments involve high costs, great expectations from the patient, and demands time for its full conclusion. However, it stands that professional obligation towards the dental implant patient should always be of means, by which the dentist uses all the available resources to treat the patient, but depends on specific biological conditions of each individual 9.
According to recent studies, the main reason for malpractice suits against implantodontists has been patient dissatisfaction with undesired and often painful results which differ from the expected, hampering the patient-professional relationship 3.
In case of complications, the dentist should talk to the patient and explain the occurrence, searching for the best solution to the case. The good relationship and trust established between patient and professional are essential for treatment success. It is necessary to respect patient autonomy as a consumer, who must decide the way treatment should be conducted, after having been oriented and informed by the clinician. These steps should be well documented, printed and stored with the patient's records 9,6.
Conclusion
Final ly, it can be concluded that, when considering the types of clinical intercurrences that might affect patients submitted to surgical procedures of preparation or actual installation of dental implants, prevention continues to be the key issue when it comes to avoiding clinical, ethical or legal repercussions. Practicing adequate diagnosis and treatment planning and conducting the necessary complementary exams are essential, allied to previously informing and obtaining a signed consent from the patient.
References
1. Andreiuolo R, Vasconcellos F, Andrade A, Groisman M, Vidigal Júnior GM. Immediate implant in the anterior region: surgical and prosthetic aspects. Rev Bras Odontol. 2016;73(1):84-8.
2. Bartling R, Freeman K, Kraut R. The incidence of altered sensation of the mental nerve after mandibular implant placement. J Oral Maxillofac Surg. 1999;57:1408-10.
3. Bortman M, Scandiuzzi RJ. Civil cases in implantology. Brazilian J Forensic Sci Med Law Bioeth. 2014;4(1):24-9.
4. Castro TL, Fernandes MM, Rosa RO, Daruge Júnior E. Responsabilidade profissional e lesões nervosas: caso judicial relacionado a enxertos cirúrgicos. Odonto. 2013;21(41-42):71-5.
5. Elian N, Mitsias M, Eskow R, Jalbout ZN, Cho S-C, Froum S et al.. Unexpected return of sensation following 4.5 years of paresthesia: case report. Implant Dent. 2005;14(4):364-7.
6. Garbin CAS, Garbin AJI, Gonçalves PE, Gonçalves SH. Term of informed consent: their importance in the brasilian dentistry. Arq Odontol. 2008;44(4):42-4.
7. Hillerup S. Iatrogenic injury to the inferior alveolar nerve: etiology, signs and symptoms, and observations on recovery. Int J Oral Maxillofac Surg. 2008;37(8):704-9.
8. Jerjes W, El-Maaytah M, Swinson B, Banu B, Upile T, D'Sa S et al.. Experience versus complication rate in third molar surgery. Head Face Med. 2006;2:14.
9. Kichler A, Fernandes MM, Oliveira RN. Failure factors in implantology and their importance in preventing lawsuits. Brazilian J Forensic Sci Med Law Bioeth. 2014;4(1):147-61.
10. Muroff FI. Removal and replacement of a fractured dental implant: case report. Implant Dent. 2003;12(3):206-10.
11. Novaes LCM, Pinheiro AR, Corvino MPF, Duarte CL, Cardoso A, Gouvêa CVD. Informed consent form in implantology. Rev Bras Odontol. 2011;68(1):16-9.
12. Robinson PP. Observations on the recovery of sensation following inferior alveolar nerve injuries. Br J Oral Maxillofac Surg. 1988;26:177-89.
13. Sandstedt P, Sörensen S. Neurosensory disturbances of the trigeminal nerve: a long-term follow-up of traumatic injuries. J Oral Maxillofac Surg. 1995;53(5):498-505.
14. Seddon HJ. A classification of nerve injuries. Br Med J. 1942;2(4260):237-9.
15. Silva RF, Barbieri L, Portilho CDM, Prado MM, Daruge Júnior E. Importance of the information provided to patient before, during, and after endodontic treatment considering the Consumer's Defense Code. RSBO. 2010;7(4):481-7.
16. Walton JN. Altered sensation associated with implants in the anterior mandible: a prospective study. J Prosthet Dent. 2000;83(4):443-9.
17. Zani SR, Berton DA, Rivaldo EG, Frasca LCF. Impossibility of prosthetic rehabilitation leading to the removal of dental implant – case report. RSBO. 2009;6(3):321-6.
 Corresponding author:
Corresponding author:
Talita Lima de Castro
Avenida Limeira, 901
CEP 13414-903
Piracicaba – SP – Brasil
E-mail: talitalima01@hotmail.com
Received for publication: August 25, 2016
Accepted for publication: September 27, 2016













