Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.13 no.4 Joinville Out./Dez. 2016
CASE REPORT ARTICLE
Chronic maxillary osteomyelitis secondary to chronic maxillary sinusitis in nonimmunocompromised patient – a rare case report and its management
Sulabha A. NarsapurI; Sameer ChoudhariII; Zameer PashaII
I Department of Oral Medicine and Radiology, Al-Ameen Dental College and Hospital, Rajiv Gandhi University – Bijapur – Karnataka – India
II Department of Oral and Maxillofacial Surgery, Al-Ameen Dental College and Hospital Rajiv Gandhi University – Bijapur – Karnataka – India
ABSTRACT
Introduction: Osteomyelitis is an inflammation of medullary portion of bone along with cortex and periosteum. It is one of most difficult infectious diseases to treat. Facial bones are prone to osteomyelitis due to various predisposing condition. Osteomyelitis of maxilla is rare disease and less frequently encountered. Objective: The aim of the article is to present an unusual case of chronic maxillary osteomyelitis secondary to rhinogenic which are rarely clinically causes. Case report: We hereby report a case of chronic maxillary osteomyelitis in 70-year-old non-immunocompromised patient secondary to chronic maxillary sinusitis. Complete resolution of chronic maxillary osteomyelitis was achieved by combination of antimicrobial therapy and surgical treatment. Conclusion: Clinician should identify such risk and provide the aggressive treatment modalities to avoid subsequent dreaded consequences.
Keywords: maxillary osteomyelitis; maxillary sinusitis; surgical treatment.
Introduction
Osteomyelitis is probably as old as mankind 6. It is defined as inflammatory condition of bone which begins as an infection of medullary cavity, rapidly involves the periosteum of the affected area 12. It is one of the most difficult infectious diseases to treat 11. In the orofacial regions, lower jaw is more frequently affected 4. Osteomyelitis of maxilla is a rare condition 13. In upper jaw, there is a cancellous bone tissue with greater vascular supply which hinders bacterial colonization, since cellular response is enhanced and it has greater blood flow that counteracts bone invasion; osteomyelitis is less frequently encountered in maxilla 4.
We report case of left chronic maxillary osteomyelitis in 70-year-old non-immunocompromised patient secondary to chronic maxillary sinusitis.
Case report
A 70-year-old male pat ient from poor socioeconomic status reported to us with complaint of brownish discolored area in left maxillary region since one to two months. It was associated with pus discharge and foul smell. Past medical history revealed a history of nasal discharge and chronic maxillary sinusitis on left side since two to two and half years for which he consulted Ear-nose-throat (ENT) surgeon and has taken medication for the same on and off. There was no history of any surgical treatment for the same. Extraoral examination revealed tenderness on the left maxillary sinus. Patient was on antimicrobial therapy for 8-10 days which was prescribed by ENT surgeon for complaint of pus discharge in the oral cavity before reporting to us.
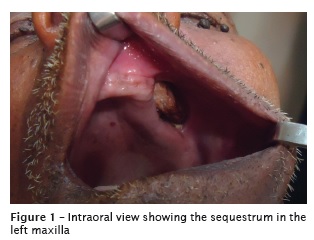
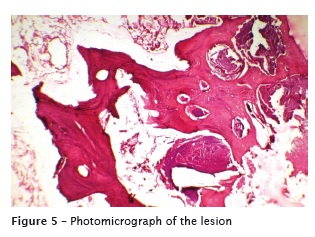
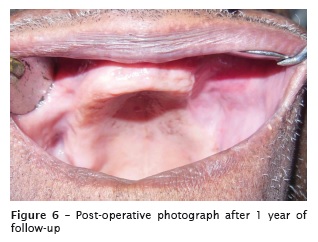
Intraoral examination revealed brownishdiscolored, loose, exposed sequestrum extending from left canine to first molar region along with scanty pus discharge from the same area (figure 1). There was tenderness along the region of the sequestrum. Panoramic view showed irregular osteolysis extending from left canine to left second premolar region on left maxilla extending superiorly to involve the left maxillary sinus (figure 2). As patient could not afford CT scan and as it was out of reach from patient's place, CT was not done in the present case. Complete hematological examination along with fasting blood sugar and postprandial blood sugar were done to rule out common immunocompromised condition such as diabetes, anemia, leukemia etc. Patient was seronegative for HIV and hepatitis. There was no history of any steroid therapy. His blood test showed elevated leukocyte count and Erythrocyte sedimentation rate (ESR) with all other parameters within normal limit. Culture of pus yielded no growth. With these findings, a clinical diagnosis of chronic suppurative osteomyelitis of left maxilla was made. Under sedation complete loose necrotic and lytic bone which was extending to involve the left antral floor, anterior wall of left antrum, and maxillary alveolar ridge from left canine to first molar was completely removed with through curettage of underlying bone. (figure 3). Through curettage and irrigation of the left maxillary sinus was done. As unhealthy sinuses can disseminate the infection to remaining bone and to relieve the symptoms of sinusitis, sinus lining was removed which was completely thickened followed with nasal antrostomy on left side. As part of that, maxillary bone was removed with direct access to sinus, oro-antral communication closure was done using buccal advancement flap (figure 4). Patient was kept on 1.2 gr. of (Amoxillin + Clavulanic acid) twice/ day, (metrogyl) 400 mg thrice/day, (gentamycin) 80 mg twice/day intravenously for 5 days along with analgesics followed by oral Amoxillin + Clavulanic acid 625 mg twice a day, metrogyl 400 mg thrice a day along with analgesics for next seven days. Histopathological examination of the specimen showed areas of trabeculae of bone devoid of osteocytes interspersed in loose connective tissue with microbial colonies confirming the diagnosis of chronic suppurative osteomyelitis (figure 5). Special stains like (PAS / H and E) did not reveal any fungal strains on histopathological examination. (Postoperatively Bismuth iodide paraffin (BIP)) antral pack was given which was removed on fifth post-operative day. Postoperative healing was uneventful. Follow up of 1 year did not show recurrence (figure 6).



Discussion
Osteomyelitis of maxilla is rare disease which was first described by Rees in 1847 6,11. Since then scattered case reports have appeared in the literature 6. Maxillary Osteomyelitis is more frequently seen in younger patients, infants, and at age range of 40-60 years 6,5. The chronic osteomyelitis may be classified as primary chronic osteomyelitis where the disease always evidenced chronic symptoms and secondary chronic osteomyelitis is evolution of previous acute osteomyelitis or local dissemination of chronic odontogenic infection 5.
Major predisposing factor for osteomyelitis is systemic condition that alters the host resistance due to immunosuppression 12. Examples of systemic conditions that decreases host defense are diabetes, autoimmune diseases, agranulocytosis, leukemia, anemia, nutrit ional deficiencies, cancer, chemotherapy, radiotherapy, alcohol and tobacco consumption, viral fevers, osteoporosis, osteopectoris, Paget's disease, FCOD, and so forth that decreases the vascularity of bone and therefore cause predisposition to the infection 1,4,9. However, the predisposing factors for osteomyelitis of maxilla also includes traumatic conditions following the injury or surgery teeth, antrum or mouth, odontogenic infections and rhinogenic causes along with systemic immunosuppression 10,13.
The pathogenesis of these may be linked to hematogenous dissemination of microorganism, contiguous spread of infection or direct inoculation of microorganism into intact bone11. Osteomyelitis caused by maxillary sinusitis is clinically rare and unusual entity 3. Spontaneous spread of the infection from the antrum is very rare; however, postoperative rhinogenic cases are more common 13. Indrizzi et al.. 7 presented a case of maxillary osteomyelitis secondary to chronic intranasal polyp. Wolfowitz 13 reported a case of osteomyelitis of maxilla secondary to trauma to facial bones and maxillary sinus. Manimaran et al.. 8 reported a case of bilateral osteomyelitis of maxilla in diabetic patient. Prasad et al.. 10 in their study showed contiguous infection such as maxillary sinusitis and odontogenic infections were main cause of maxillary osteomyelitis followed by trauma. The present case may be secondary chronic osteomyelitis due to local dissemation of chronic rhinogenic infection in non-immunocompromised patient without any trauma which is clinically very rare and makes this unusual entity.
Infection is more likely to occur in the spongy bone of the alveolar arch than in the relatively hard compact bony walls of the antrum. Maxillary derives its arterial supply almost entirely from the internal maxillary artery and its branches being anatomizing arcades. Sequestrum may therefore be localized, but when internal maxillary artery is itself thrombosed, the whole maxilla sequestrates. In the present case, the sequestrum was localized involving the maxillary alveolar bone but extending to involve the floor and anterior wall of the left antrum 13.
Specific infectious agent responsible for chronic osteomyelitis is difficult to identify. 80- 90% of chronic osteomyelitis cases demonstrate Staphylococcus aures and Staphylococcus epidermis. Most of the infections are as result of polymicrobial oral flora which includes Facultative streptococci, Peptococcus, Peptostreptococci, Bacteroides, Hemolytic streptococci, Pnemococci, Escheriquia coli, Actinomyces, etc. 1,4.
Functional imaging of the craniofacial skeleton is necessary for a complete treatment regimen in patients with the osteomyelitis. Conventional radiographs, CT, MRI, SPECT scans can be used for the detection of the lesion 9. Radiographically spotty osteolytic changes are more frequently observed in chronic osteomyelitis of the maxilla while osteosclerosis is rare 13. Sometimes shows opaque focal areas. Lesions are normally quite extended, often with undistinguishable borders 4. Progressive bony destruction and formations of sequestrations are hall marks of the osteomyelitis 11.
The differential diagnosis includes maxillary necrosis secondary to viral infect ions such as herpes zoster and secondary to fungal infections such as mucormycosis, aspergillosis, etc. Appearance of vesicular mucocutaneous lesions with other investigations for presence of herpes virus rules out maxillary necrosis secondary to herpes zoster. Maxillary necrosis secondary to fungal infection can be ruled out by histopathological examination of fungal strains by special stains 2,11.
The goal of the treatment is eradication of the infection and restoration of the function. Osteomyelitis treatment requires antibiotics and surgical treatment 11. The main treatment consists of stabilizing the systemic condition of the immune-compromised patient, culture of the associated microorganism, sensitivity tests, image assessment to determine the lesion extension, empiric administration of antimicrobials drugs to combat predominant microorganism, removal of septic foci such as teeth and bone sequestrations, debridement, decortications or resection according to the case. Hyperbaric oxygen, bisphosphonates, corticosteroids have been used as adjuvant treatment for chronic osteomyelitis 4. Nasal endoscope has also been used in the treatment of chronic osteomyelitis of the maxilla and zygoma 1. Surgical debridement with antimicrobial therapy along with non-immunocompromised condition of the patient was most important factors for successful out comes in our case.
To conclude osteomyelitis of jaw is challenging infectious disease both for the clinician and the patient, despite many advances in diagnosis and treatment. Spread of inflammation or infection with involvement of the surrounding structure represents important risk as seen in the present case. Dentist should identify such risk and provides the aggressive treatment modalities to avoid subsequent dreaded consequences.
References
1. Arunkumar JS, Naik AS, Prasad KC, Santosh SG. Role of the nasal endoscopy in chronic osteomyelitis of maxilla and zygoma: a case report. Case Reports in Medicine. 2011;2011:1-3. [ Links ]
2. Auluck A. Maxillary necrosis by mucormycosis. A case report and literature review. Med Oral Patol Oral Cir Bucal. 2007;12:E360-4.
3. Chae SR, Kim JH, Park SY, Kim BG. Oroantral fistula originating from osteomyelitis accompanied by maxillary sinusitis. J Rhinol. 2011;18(2):146-50.
4. Fish AO, Espinosa CJI, Parra VR, Quezada SR. Upper jaw chronic osteomyelitis. Report of four cases. Revista Odontologica Mexicana. 2012:16(2):105-11.
5. Gaetti-Jardim Jr E, Ciesielski FIN, Possagno R, Castro AL, Marqueti AC, Gaetti-Jardim EC. Chronic osteomyelitis of the maxilla and mandible: microbiological and clinical aspects. Int J Odontostomat. 2010;4(2):197-202.
6. Greenberg AM, Prein J. Craniomaxillofacial reconstruction and corrective bone surgery: principles of internal fixation using the AO/ASIF technique. New York: Springer; 2002.
7. Indrizzi E, Terenzi V, Renzi G, Bonamini M, Bartolazzi A, Fini G. The rare condition of maxillary osteomyelitis. J Craniofac Surg. 2005;16(5):861-4.
8. Manimaran K, Suresh K, Kannan R. Osteomyelitis of maxillae bilateral involvement: a case report. JIADS. 2011;2(2):57-8.
9. Pincus DJ, Armstrong MB, Thaller SR. Osteomyelitis of craniofacial skeleton. Semin Plast Surg. 2009;23(2):73-9.
10. Prasad KC, Prasad SC, Mouli N, Agarwal S. Osteomyelitis in head and neck. Acta Oto Laryngol. 2007;127:194-205.
11. Singh M, Singh S, Jain J, Singh KT. Chronic suppurative osteomyelitis of maxilla mimicking actinimycotic osteomyelitis: a rare case report. Natl J Maxillofac Surg. 2010;1(2):153-6.
12. Topazian RG, Goldberg MH, Hupp JR. Oral and maxillofacial infections. 4. ed. Philadelphia: WB Saunders and Company; 2002.
13. Wolfowitz BL. Osteomyelitis of the maxilla. SA Medical Journal. 1971 June:632-33.
 Corresponding author:
Corresponding author:
Sulabha. A. Narsapur
Department of Oral Medicine and Radiology
Al-Ameen Dental College and Hospital, Athani Road
Bijapur-586108
Karnataka – India
E-mail: sulabha595@rediffmail.com
Received for publication: August 3, 2016
Accepted for publication: October 28, 2016













