Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.14 no.1 Joinville Jan./Mar. 2017
ORIGINAL RESEARCH ARTICLE
Secondary alveolar bone graft in patients with bilateral cleft lip and palate submitted to premaxilla repositioning: retrospective study
Tuanny Carvalho de Lima do Nascimento I,II; Fernando Luiz Zanferrari I; Juliana Lucena Schussel I; José Luís Dissenha I; Laurindo Moacir Sassi I; João Luiz Carlini II
I Department of Oral and Maxillofacial Surgery, Erasto Gaertner Hospital – Curitiba – PR – Brazil
II Oral maxillofacial surgery Staff, Cleft Lip and Palate Integral Care Center – Curitiba – PR – Brazil
ABSTRACT
Introduction and Objective: This study aimed to analyze the effectiveness of the closure of oronasal communication, to report the importance of secondary alveolar bone graft repositioning of the premaxilla in patients with bilateral complete cleft lip and palate. Material and methods: This retrospective study analyzed the medical records obtained from the Cleft Lip and Palate Integral Care Center/ Association of Rehabilitation and Social Development of Cleft Lip and Palate Patients (CAIF/AFISSUR), Curitiba – Paraná – Brazil, to obtain statistical data involving 26 records of patients who underwent this surgery in the period between January/2010 – January/2014. Results and Conclusion: The benefits observed were: premaxilla stability, aided by the union of pre-maxillary segments; integrity of oronasal structure; aesthetic improvement; better bone support for the teeth adjacent to the cleft; support for the bridge of the nose reducing facial asymmetry and facilitating future rhinoplasty; orthodontic treatment without the limitation of the bone defect; closure of oronasal communication in 88% of patients.
Keywords: cleft lip; cleft palate; alveolar bone grafting.
Introduction
Cleft lip and palate (CLP) occurs at the intrauterine period due to congenital malformation caused by the absence of fusion of the palate. CLP is the most prevalent congenital abnormality of the face worldwide.
In Brazil, the incidence of cases is 1 at 650 individuals and it is estimated that there are around 225.000 people with this type of cleft, with more prevalence in men 2,8. Many authors follow the classification adopted by Spina 27 that uses, as reference element, the incisive foramen, which is characterized by the boundary between the primary and secondary palates - prolabium, premaxilla and cartilaginous septum - dividing the clefts into three types: pre-foramen, post-foramen and trans-foramen 2,7,27. In this sense, pre-foramen cleft may be unilateral, bilateral and median; the post-foramen cleft is characterized as mainly median cleft palate, that may involve only in the uvula and soft palate, or all hard palate 7,27.
Still according to Spina's classification, both unilateral and bilateral trans-foramen clefts are more severe, since they affect the lip, alveolar process and palate 6,7,27. The complete bilateral cleft is the most severe and extensive one, with a prevalence of 14-18% 23. In patients with bilateral trans-foramen cleft with the pre-maxilla poorly positioned by severe anterior projection, the replacement of the premaxilla is indicated together with the secondary alveolar bone graft 6,17.
The indications of alveolar bone graft (ABG) are related to the need for bone support to erupted or non-erupted teeth adjacent to the cleft; premaxilla stabilization in the case of bilateral clefts; continuity of the alveolar ridge; support of the alar base; nasolabial contour; and the elimination of oronasal fistula. Patients not submitted to ABG may progress to periodontitis in the tooth adjacent to the cleft due the absence of bony septum on that region 20.
According to the time is performed, ABG is divided into primary, secondary and tertiary bone graft. The primary bone graft is held early at the first years of life, causing, from our point of view, the major disadvantages to the patient, mainly the deficit of maxillary growth. The secondary alveolar bone grafting is performed before the eruption of the permanent canine, while the tertiary ABG occurs after canine eruption. The secondary ABG has better results than the tertiary ABG by providing better periodontal conditions for teeth adjacent to the cleft 25.
This retrospective study evaluated 26 patients with transforamen bilateral clefts who underwent surgical replacement of the premaxilla concomitantly with bone graft to promote reformatting of the maxillary arch, premaxilla stability and allow the eruption of the canines, returning facial aesthetics and reintegrating the patient into society.
Material and methods
The study was developed in the Cleft Lip and Palate Integral Care Center/ Association of Rehabilitation and Social Development of Cleft Lip and Palate Patients (CAIF/AFISSUR), located in Curitiba, PR, with a retrospective method, analyzing medical records to obtain statistical results regarding the use of the surgical technique of secondary alveolar bone grafting in patients with bilateral cleft lip and palate, submitted to reposition of the premaxilla. The study was approved by the Institutional Review Board regarding ethical aspects.
Inclusion criteria comprised records selected from January/2010 to January/2014 properly treated by the multidisciplinary team. Exclusion criteria included incomplete records or records of patients with incomplete cleft lip and palate, unilateral complete cleft lip and palate and those who only underwent ABG without repositioning of the premaxilla.
The medical records were evaluated according to the following variables: gender, age, donor area of bone graft, date of surgery and the transoperative and postoperative complications. Data analysis was performed using specific software, SPSS 23 - Statistical Package for Social Sciences, which allows the measurement of success-failure rates of the surgical procedure in question.
Results
Of 109 records, 26 met the inclusion criteria. The survey data allowed to report the importance of secondary alveolar bone graft with the premaxilla replacement to restore the closure of oronasal communication on patients with bilateral transforamen cleft lip and palate. Based on the reported complications, we obtained the rates for transoperative and postoperative complication, successful and unsuccessful procedures. Table I shows the data collected from medical records.
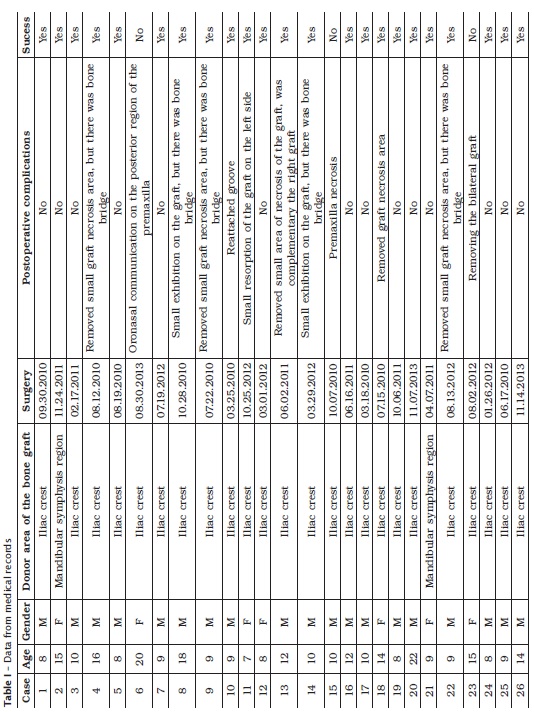
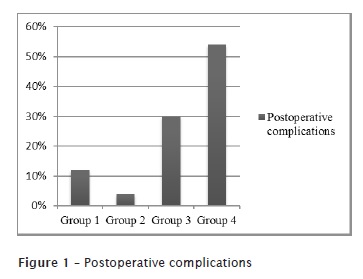
The sample age ranged from 07-22 years, with predominance of males (73%) over females (27%). Most of the bone graft donor area were obtained from the iliac crest (92%) rather than from the mandibular symphysis region (8%). According to figure 1, the postoperative complications were distributed into 4 groups:
• Group 1: serious complications, such as pre-jaw necrosis, removal of bilateral graft and oronasal communication on the posterior region of the premaxilla = 12%;
• Group 2: complications solved with new surgical act, such as removal of small graft necrosis area with complementary graft = 4%;
• Group 3: patients who had a small resorption of the graft but with the presence of bone bridge, but with no need for a new surgery, and who required replacement of the surgical guide = 30%;
• Group 4: 54% of patients had no postoperative complications.
The closure of the oronasal communication were achieved in in 88% of patients undergoing surgery, without transoperative complications.
Discussion
There is a consensus among authors that the clefts are a congenital malformation with a multifactorial etiology, which occurs in the embryonic period (3rd to 8th week of intrauterine life) and early fetal period (7th to 12th week of intrauterine life), due to disability or lack of fusion between primary and secondary facial and palatal processes 5,9,21-23,29.
The left unilateral complete cleft lip and palate is the most common type 5. Bilateral complete clefts are the most serious and extensive anomaly with prevalence between 14-18% 23. This percentage is very close to the prevalence observed in CAIF / AFISSUR.
Patients with CLP require a surgery to restore the esthetics and increase the self-esteem by the oronasal closure, allowing mechanical and functional characteristics 2,6-8,12,15,17,27. One of these solutions is the repositioning of the premaxilla with alveolar bone graft.
Some facial features are observed in these patients, such as exaggerated convexity, significant reduction of nasal columella and lowering of the nasal apex, resulting from a projection of premaxilla which differs according to its positioning 23. It is observed in the sample selected for this study that, in addition of these features, premaxilla positioning greatly affect the format of the maxillary arch, causing significant cosmetic change. Some factors such as cleft width, size of the bone segments and its position will influence on the prognosis 23.
The benefits observed with secondary bone graft with the premaxilla replacement were: stability to premaxilla; aid in the union of pre-maxillary segments; integrity of oronasal structure; aesthetic improvement; better bone supporting to the teeth adjacent to the cleft; support for the bridge of the nose; decreased facial asymmetry that facilitates future rhinoplasty; orthodontic treatment without the limitation of the bone defect; closure of oronasal fistulas; and placement of dental implants in the cleft region 23,29.
The success of alveolar graft is based on the use of effective surgical techniques so there is no mucoperiosteal buccal tension and suitable recoating with keratinized gingiva on the graft 3,4,10,13,14,16,22,24,26,28.
The secondary alveolar bone graft should be performed prior to eruption of the permanent canines. When carried out early, it prevents the anteroposterior growth of the maxilla and, after its eruption, in most cases, there is poor periodontal status 2,6-8,15,17,27. According to our study, most of the patients had the surgical procedure at the ages of 9, 8, and 10 years old.
Concerning to the preoperative preparation, Albuquerque 1 and the protocol adopted in CAIF / AFISSUR suggest that previously to the secondary alveolar bone graft, the patients should undergo orthodontic treatment and maxillary expansion is the most common treatment type.
The most common donor area is the iliac crest, since it is easily accessible and provide sufficient bone amount, allowing orthodontic movement. According to Ibrahim et al. 15, Silva Filho et al. 26 and Kortebein et al. 18, iliac crest graft achieved better results than skullcap graft (89.9% versus 63%). This was observed in this study, in which 92% of bone grafts were obtained from the iliac crest and 8% from the mandibular symphysis region.
The surgical technique for the reposition of premaxilla with bone graft indicated by Fakin-Gomez 15 is extremely complex, requiring perfect closure of the mucosa of the nasal cavity and bone osteotomy of premaxilla and osteotomy reducing the vomer-premaxilla suture to achieve a better fixation of the premaxilla in the arch. These observations are also consistent with the surgical technique adopted by CAIF / AFISSUR. Another author suggests a procedure in two surgical times to ensure blood supply to the premaxilla 19. We disagree with this approach because the perfect closure of the nasal mucosa requires the displacement of the pre-jaw for a better view, concluding that to perform the procedure in a single time is more beneficial for the patient.
This study sample showed no transoperative complications, but in relation to postoperative complications, 4% of the patients had premaxilla necrosis, oronasal communication on the posterior region of the premaxilla and loss of bilateral bone graft. The remaining cases showed a slight resorption of the graft, but with formation of bone bridge. These findings are similar to those of the study of Ibrahim et al. 15, who affirms that the complications of the surgical procedure may include necrosis of the palatal tissue, resorption of the grafted bone, suture dehiscence, necrosis of tissue and contamination of the graft caused by the characteristics of difficult access to the cleft, deficient blood supply, fibrotic tissue, cleft amplitude, presence of oronasal fistula of varying sizes, minimum amount of healthy tissue to cover the bone graft, and the surgeon's skill.
This present study showed that the prognosis of oronasal communication closure was high with 88% of the patients had excellent closure of oronasal communication and 12% did not. Fakih-Gomez et al. 11 on the other hand, observed no complications, including loss of premaxilla. Other authors studied the oronasal closure as Albuquerque 1 and Gomes et al. 12, stating that to occur complete rehabilitation of the patient with lip and palate cleft, the intervention of a multidisciplinary team is required.
Conclusion
Based on this study results, it can be concluded that the secondary alveolar bone graft with pre-maxilla replacement promoted the premaxilla stability, helped the union of pre-maxillary segments and closed the oronasal fistulas in 88% of patients. Therefore, the surgery has a good rate of effectiveness and the results are close to those presented by the literature available on this subject.
References
1. Albuquerque MVP. Enxerto ósseo alveolar secundário. Monograph – Hospital de Reabilitação de Anomalias Craniofaciais, Universidade de São Paulo, Bauru; 1998.
2. Alonso N, Tanikawa DYS, Lima Junior JE, Rocha DL, Sterman S, Ferreira MC. Fissuras labiopalatinas: protocolo de atendimento multidisciplinar e seguimento longitudinal em 91 pacientes consecutivos. Rev Bras Cir Plást. 2009;24:176-81.
3. Behnia H, Mesgardzadh A, Tehranchi A, Morag G, Samieerad S, Younessian F. Stabilization of premaxilla repositioned during secondary bone grafting in complete bilateral cleft lip and palatepatients. J Craniofac Urg. 2014;25:1554.
4. Boyne PJ, Sands NR. Secondary bone grafting of residual alveolar and palatal clefts. J Oral Surg. 1972;30:87-92.
5. Capelozza Filho L, Cardoso Neto J, Silva Filho OG. Non-surgically assisted rapid maxillary expansion in adults. Int J Adult Orthod Orthognat Surg. 1996;11:57-66.
6. Carlini JL. Utilização da cortical da crista ilíaca para fixação da pré-maxila na reconstrução dos pacientes fissurados lábio-palatais bilaterais. Colégio Brasileiro de Cirurgia e Traumatologia Buco-Maxilo-Facial. Capítulo VIII. 2011;1.
7. Carlini JL, Biron C, Gomes KU, Silva RM. Surgical repositioning of the premaxilla with bone graft in 50 bilateral cleft lip and palate patients. J Oral Maxillofac Surg. 2009;67:760-6.
8. Carlini JL, Zétola AL, Souza RP, Denardin OVP, Rapoport A. Enxerto autógeno de crista ilíaca na reconstrução do processo alveolar em portadores de fissura labiopalatina – estudo de 30 casos. Revista do Colégio Brasileiro de Cirurgiões. 2000;27:389-93.
9. Carreirão S, Lessa S, Zanini AS. Embriologia da face. In: Tratamento das fissuras labiopalatinas. 2. ed. Rio de Janeiro: Revinter; 1996. p. 1-12.
10. Dempf R, Teltzrow T, Kramer FJ, Hausamen JE. Alveolarbone grafting in patients with complete clefts: a comparative study between secondary and tertiary bone grafting. Cleft Palate Craniofac J. 2002;39:18-25.
11. Fakih-Gomez N, Sanchez-Sanchez M, Iglesiais-Martin F, Garcia-Perla-Garcia A, Belmonte-Caro R, Gonzalez-Perez LM. Repair of complete bilateral cleft lip with severely protruding premaxilla performing a premaxillary setback and vomerine ostectomy in one stage surgery. Med Oral Patol Oral Cir Bucal. 2015 Jul 1;20:500-7.
12. Gomes KU, Rapaport A, Lehn CN, Denardin OVP, Carlini JL. The life quality impact after surgical pre maxilla repositioning in patients with bilateral lip palatal cleft – study of 50 cases. Rev Col Bras Cir. 2009;35.
13. Heidbuchel KL, Kuijpers-Jagtman AM, Kramer GJ, Prahl-Andersen B. Maxillary arch dimensions in bilateral cleft lip and palate from birth until four years of age in boys. Cleft Palate Craniofac J. 1998;35(3):233-9.
14. Horswell BB, Henderson J. Sencondary osteoplasty of the alveolar cleft defect. J Oral Maxillofac Surg. 2003;61:1082-90.
15. Ibrahim D, Faco EFS, Santos Filho JHG, Faco RAS. Enxerto ósseo alveolar secundário em pacientes portadores de fissuras lábio-palatais: um protocolo de tratamento. Rev Fac Odontol. 2004;16:13-8.
16. Kawakami S, Hiura K, Yokozeki M, Seike T, Nakanishi H, Moriyama K. Prognostic Implications of nasal cavity and cleft morphology in secondary bone grafting. Cleft Palate J. 2002;6:575-81.
17. Kokai S, Fukuyama E, Sato Y, Hsu JC, Takahashi Y, Hayarada K et al. Comprehensive treatment approach for bilateral cleft lip and palate in an adult with premaxillary osteotomy, tooth autotransplantation, and 2-jaw surgery. Am J Orthod Dentofacial Orthop. 2015;147:114-26.
18. Kortebein MJ, Nelson CL, Sadove AM. Retrospective analysis of 135 secondary alveolar cleft grafts using iliac or calvarial bone. J Oral Maxillofac Surg. 1991;49:493-8.
19. Lino M, Sasaki T, Kochi S, Fukuda M, Takahashi T, Yamaguchi T. Surgical repositioning of the premaxilla in combination with two-stage alveolar bone grafting in bilateral cleft lip and palate. Cleft Palate Craniofac J. 1998;35:304-9.
20. Lisa LYS, Lui WWK. Alternative donor site for alveolar bone grafting in adults with cleft lip and palate. Angle Orthod. 1996;66:9-16.
21. Nagem Filho H, Moraes N, Rocha RGF. Contribuição para o estudo da prevalência das malformações congênitas labiopalatais na população escolar de Bauru. Fac Odontol Univ São Paulo. 1968;6:111-28.
22. Rodrigues APGM, Castro CHBC. Implications and treatment of cleft lip and palate in patients with an autognenous bone graft. Revista Brasileira de Cirurgia Buco-Maxilo-Facial. 2010;10:91-6.
23. Rodrigues RM, Costa B, Gomide MR, Neves LT. Fissura completa bilateral: características morfológicas. Revista de Odontologia da UNESP. 2005;34:67-72.
24. Russel KA, Mcleod CE. Canine eruption in pacients with complete cleft lip and palate. Cleft Palate J. 2008;45:73-80.
25. Semb G. Effect of alveolar bone grafting on maxillary growth in unilateral cleft lip and palate patients. Cleft Palate J. 1988;25:288-95.
26. Silva Filho OG, Freitas JAS, Okada T. Fissuras labiopalatinas: diagnóstico e uma filosofia interdisciplinar de tratamento. In: Pinto VG. Saúde bucal coletiva. 4. ed. São Paulo: Santos; 2000. p.481-527.
27. Spina V. A proposed modification for the classification of cleft lip and palate. Cleft Palate J. 1973;10:2512-6.
28. Takahashi T, Fukuda M, Echigo S. Long-term follow-up of dental implants placed in a grafted alveolar cleft: evaluation of alveolar bone height. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:297-302.
29. Wolford LM, Stevao ELL. Corretion of jaw deformities in pacients with cleft lip and palate. Proc. 2002;15:250-4.
 Corresponding author:
Corresponding author:
João Luiz Carlini
Av. Iguaçu, 2820, apto 901
CEP 80240-030
Curitiba – PR – Brasil
E-mail: joaoluizcarlini@gmail.com
Received for publication: January 17, 2017
Accepted for publication: February 24, 2017













