Services on Demand
Article
Related links
Share
RSBO (Online)
On-line version ISSN 1984-5685
RSBO (Online) vol.14 n.1 Joinville Jan./Mar. 2017
Case Report Article
Oral rehabilitation with removable dental prosthesis in a six-year-old patient with hypohidrotic ectodermal dysplasia
Mariana Dalledone I; Fernanda Mara de Paiva Bertoli II; Ana Paula Sponchiado II; Estela Maris Losso II; João Armando Brancher II; Juliana Feltrin de Souza III
I Clinical Dentistry, Positivo University – Curitiba – PR – Brazil
II Dentistry Department, Positivo University – Curitiba – PR – Brazil
III Dentistry Department, Federal University of Paraná – Curitiba – PR – Brazil
ABSTRACT
Introduction: Ectodermal dysplasia is an abnormality of the ectoderm and its derivatives, phenotypically expressed in males and genetically inherited from mothers. Objective: To report the efficacy of the prosthetics treatment of severe ectodermal dysplasia in a 6-year-old boy with hypohidrotic ectodermal dysplasia (HED). Case report: The boy had difficulty in speaking and eating and the condition also affected his self-esteem. Prosthetic treatments included the construction of acrylic custom trays, determination of the vertical dimension of occlusion (VDO), construction of upper and lower dentures, and palatal expansion procedure. Conclusion: Significant improvements in the patient's stomatognathic function and self-esteem were evident.
Keywords: ectodermal dysplasia (ed); child; denture partial removable.
Introduction
Ectodermal dysplasia is an abnormality of the ectoderm and its derivatives. It is a rare, X-linked genetic trait that affects approximately 1 in 10,000 live-born males and 1 in 100,000 live-born females 3,10, at a male to female ratio of 5:1, respectively. Generally, it has phenotypic expression in males and can be genetically inherited from mothers. Classification is determined by the combination and severity of the following affected traits: hair follicles, teeth, and sweat glands. These factors contribute to an intolerance towards heat, causing the body temperature to rise 10. Furthermore, the etiology considers the phenotypic severity of the affected sweat glands 2,4,13,14. Hypohidrotic (anhidrotic) ectodermal dysplasia (HED), which is a recessive, X-linked disorder, has a more severe presentation in individuals than its hidrotic form, which follows an autosomal dominant mode of inheritance, and shows only a minor presentation 7.
According to a study in 2007 14, HED, which is also known as Christ-Siemens-Touraine syndrome, is the most common form of ectodermal dysplasia. The oral-facial features of HED include: agenesis or hypodontia, affecting both deciduous and permanent dentition; conical or peg-shaped teeth; the stunted development of alveolar ridges; and a decreased, lower facial height resulting in a reduced, vertical dimension. This gives the appearance of a more senile facial profile with dry and protuberant lips 4,10,14, a prominent forehead, a saddle-shaped nose, small cranial base width, and hypotrichosis. Hummel and Guddack 9 emphasized the importance of early action in the oral rehabilitation of dysplastic patients; they considered the minimum resorption or atrophy of the alveolar ridges and the restoration of the vertical dimension of occlusion (VDO).
This study describes the rehabilitation and restoration of the VDO in a 6-year-old child with HED. Only four anterior, deciduous teeth were used as abutments for the removable prosthesis.
Case report
The male patient, aged 6 years, arrived at the Positivo University clinic, accompanied by his mother; she was concerned by her child's "lack of teeth and difficulties in feeding and speech". The patient's medical history showed no significant physical alterations. During extraoral examination, the following characteristics of ectodermal dysplasia were identified: scarcity of eyelashes and eyebrows, periorbital pigmentation, protuberant lips, shrunken lower third of the face, and a mandibular profile with marked retrognathism. These features contribute to a more senile appearance (figure 1(a), 1(b), 1(c) and 1(d)).
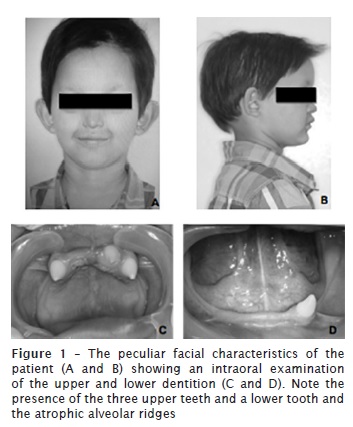
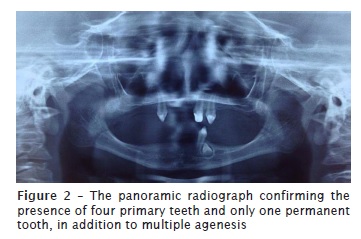
The intraoral examination revealed the presence of only three upper teeth (#53, #62, #63) and one lower tooth (#73), all of which were conoid-shaped. Atrophy in the maxillary and mandibular alveolar ridges was also evident (figure 1(c) and 1(d)). Radiographic confirmation (Figure 2) also revealed the presence of these teeth and of only one permanent, conoid-shaped tooth (#33). Based on these examinations, and the signs and symptoms of the patient's condition, the clinical diagnosis and treatment plan considered prosthetic and functional rehabilitation, and the restoration of the VDO via removable tooth-mucosa-supported dentures. These dentures would preserve the existing dentition until the patient had adequate bone growth enabling rehabilitation with a fixed support system, such as the use of implants. The patient's mother consented to the treatment plan and was made aware of the following limitations: the scarcity of teeth capable of supporting the prosthesis; the long treatment process, involving both clinical and laboratory components; and the patient's crucial collaboration and satisfaction.
Firstly, a study cast was obtained through the impression using alginate (Cavex Colorchange, Netherlands) to verify the load-bearing capacity of the teeth; the teeth would function as pillars for the prosthesis and allow for the fabrication of the custom tray. To reestablish the aesthetic, tooth #62 underwent a direct restoration with composite resin. Additionally, to increase the mesiodistal space for the stock tooth, a light wear of the mesial face was performed, to account for the establishment of the midline.
An acrylic custom tray that accommodated the patient's lips was constructed followed by the aid of a low fusion Godiva (Kerr, Brazil). Functional impression was performed using an elastic polyether material (3M- Impregum, Germany) and adhesive (polyether adhesive 3M, Germany). Owing to the presence of teeth, it was not possible to use a zinc-enolic paste to perform a traditional impression. The VDO was determined in accordance with the Willis method; a Willis compass was used (figure 3(a)), the VDO should be 2 mm shorter than the vertical dimensions measured at rest.
Subsequently, the intermaxillary relationship was determined, which included the following factors: the VDO (using the Willis compass), the presence of a high smile line, the line of canines, the Spee curvature and the presence of parallelism with the bipupilar plane (the latter two was measured using a Fox strip [Bioart]). The fixation of the upper and lower orientation planes was performed after the patient's mandible was positioned into a centric relation. Additionally, the wax ridges were fixed to maintain the height of the VDO in a stable position (figure 3(b)).
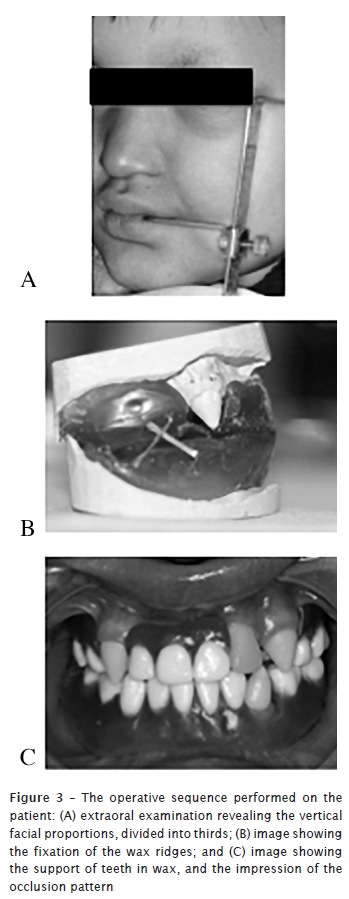
The teeth were fitted in wax for the final adjustments and alignments, including both the upper and lower prostheses. Emphasis was placed on the midline and aesthetic principles, including tooth height and smile line, as well as the checking of the occlusion. This verified the need to attach circumferential clamps to the two upper canines to improve the retention of the prosthesis. The upper prosthesis was divided near the line of the palatine raphe to place an expander that would prevent any bone growth restrictions. This avoids the necessity of frequently replacing the prosthesis because of alterations in bone anatomy. The expander would be fastened by a ¼ turn at two-month intervals, or as needed, based on periodic appointments; vigilance was required for signs of bone growth, such as marks of the prosthesis on the patient's palate.
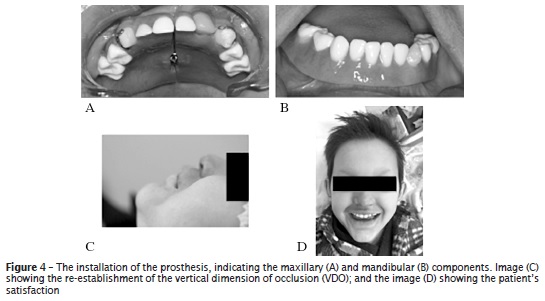
During the initial fitting, a retention was fabricated using composite resin on the upper canine's labial region to improve the retention of the upper prosthesis. The lower prosthesis was adapted; however, stability could not be maintained due to the presence of a single supporting tooth and the lack of an alveolar ridge (figure 4(a-d)). For the first month, during the adaptation phase, the patient returned for follow-up every 7 days. During this period, improvements in speech and swallowing were evident, but the use of the lower prosthesis caused difficulties with chewing and caused lacerations on the mucosa. Prosthesis adjustments were made in relation to the patient's lip and the prosthesis was re-coated with Silagum material (DMG, Germany).
The patient was instructed to discontinue the use of the lower prosthesis, until eight years of age, following the many unsuccessful attempts to improve its adaptation. At the age of eight, the patient would be eligible for the insertion of implants in the anterior region of the jaw, and the placement of an overdenture 1,8.
After 6 months, no lacerations were reported, and the upper prosthesis was well adapted. This assisted the patient in speaking, chewing, and swallowing. The expansion of the upper prosthesis was performed with a ¼ turn of the thread. Tooth functioning was retained in the lower ridge.
Discussion
Hypohidrotic ectodermal dysplasia has the most severe presentation of all forms of ectodermal dysplasia. It is characterized by reduced sweat gland function and is clinically comorbid with hypotrichosis, hypohidrosis, and either hypodontia or anodontia 1,6. It is a hereditary, X-linked trait in which genetic counseling is beneficial for both parent and child, because of the possibility of reoccurrence within the family 16. Most of patients with HED has multiple comorbidities, and aside from the health-related issues with dentition, include ocular, infectious and dermatological issues. This requires a multidisciplinary approach from healthcare professionals to achieve its global treatment 6.
The range of treatments for hypodontia/anodontia include partial or complete prostheses that are either fixed or removable, as well as implant-supported prostheses. Treatment should be initiated as early as possible so that the increased resorption or atrophy of the alveolar ridges, attributable to the complete or partial absence of teeth, can be reversed. Additionally, early treatment allows for the VDO to be controlled or stabilized 11,15. The psychological and esthetic-related issues become more apparent to the patient as they progress through the stages of childhood development. Therefore, the initiation of prosthetic treatment for these patients has been strongly recommended 9. In the present study, the approach of using a removable prosthesis was based on the child and mother's preference. The emphasis on the esthetic properties of the prosthesis and the restoration of masticatory and phonetic functions showed clear and rapid improvements in these areas, and aided the patient's psychosocial development. The conoid-shaped teeth assisted in the retention of the prostheses, even after the creation of a "stop" on the composite resin. The child adapted well to the upper prosthesis, expressing great personal satisfaction. The absence of many of the lower teeth and the presence of severe resorption of the alveolar ridges, contributed towards the instability and the discomfort of the lower prosthesis. The lacerations that occurred during the first month influenced the child's negative and non-cooperative behavior regarding its use.
In this study, the prostheses needed to be renewed periodically to accommodate the child's bone growth and development. Franchi et al. 5 analyzed the cephalometry of various patients with ectodermal dysplasia, and showed that the use of conventional prostheses could assist in the satisfactory growth of the maxilla and mandible, in addition to stimulating the growth of the alveolar ridges to enable further treatment with implant-supported prostheses. This is a fixed alternative that can maintain the esthetic and result in a greater rate of acceptance among patients. This method will be offered to the patient in the future 5,9. Additionally, significant improvement in the patient's self-esteem was evident.
Competing interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
1. Abadi B, Herren C. Clinical treatment of ectodermal dysplasia: a case report. Quintessence Int. 2001 Oct;32(9):743-5. [ Links ]
2. Corrêa MSNP, Ulson RCB, Rodrigues CRMD, Azevedo AM. Displasia ectodérmica hereditária: revisão da literatura com relato de um caso clínico. Rev Paul Odontol. 1997;19(1):30-2.
3. Della Valle D, Chevitarese AB, Maia LC, Farinhas JA. Alternative rehabilitation treatment for a patient with ectodermal dysplasia. J Clin Pediatr Dent. 2004;28(2):103-6.
4. Echeverria SR, Fernandes AL, Politano GT, Imparato JCP. Reabilitação estético-funcional em paciente com síndrome da displasia ectodérmica hereditária hidrótica. J Bras Clín Odontol Integr. 2003;7(41):417-20.
5. Franchi L, Branch R, Tollaro I. Craniofacial changes following early prosthetic treatment in a case of hypohidrotic ectodermal dysplasia with complete anodontia. ASDC J Dent Child. 1998 Mar-Apr;65(2):116-21.
6. Gorlin RJ, Cohen MM, Hennekam RC. Hypohidrotic ectodermal dysplasia. in syndromes of the head and neck. 4. ed. Oxford: Oxford University Press; 2001.
7. Guckes AD, Roberts MW, Mccarty GR. Patten of permanent teeth present in individuals with ectodermal dysplasia and severe hypodontia suggests treatment with dental implants. Pediatr Dent. 1998 Jul-Aug;20(4):278-80.
8. Heuberer S, Dvorak G, Mayer C, Watzek G, Zechner W. Dental implants are a viable alternative for compensating oligodontia in adolescents. Clin Oral Implants Res. 2015 Apr;26(4):22-7.
9. Hummel P, Guddack S. Psychosocial stress and adaptive functioning in children and adolescents suffering from hypohidrotic ectodermal dysplasia. Pediatr Dermatol. 1997 May-Jun;14(3):180-5.
10. Kupietzky A, Houpt M. Hypohidrotic ectodermal dysplasia: characteristics and treatment. Quintessence Int. 1995;26(4):285-91.
11. Mankani N, Chowdhary R, Patil BA, Nagaraj E, Madalli P. Osseointegrated dental implants in growing children: a literature review. J Oral Implantol. 2014 Oct;40(5):627-31.
12. Mishra SK, Chowdhary N, Chowdhary R. Dental implants in growing children. J Indian Soc Pedod Prev Dent. 2013 Jan-Mar;31(1):3-9.
13. Ortega KL, Almeida CEAL, Natalino NRS. Displasia ectodérmica anidrótica hereditária. Rev Assoc Paul Cir Dent. 1995;49(6):473-5.
14. Rad AS, Siadat H, Monzavi A, Mongoli AA. Full mouth rehabilitation of a hypohidrotic ectodermal dysplasia patient with dental implants: a clinical report. J Prosthodont. 2007 May-Jun;16(3):209-13.
15. Sadashiva KM, Shetty NS, Hegde R, Karthik MM. Osseointegrated supported prosthesis and interdisciplinary approach for prosthodontic rehabilitation of a young patient with ectodermal dysplasia. Case Rep Med. 2013;13:1-5.
16. Shekhar G, RamaRaju A, Rao C, Sarada. Prosthetic rehabilitation for a patient with hypohidrotic ectodermal dysplasia: a clinical case. Braz J Oral Sci. 2010 Jan-Mar;9(1).
 Corresponding author:
Corresponding author:
Mariana Dalledone
Rua Pedro Viriato Parigot de Souza, 5300 – Campo Comprido
CEP 81280-330 – Curitiba
Paraná – Brasil
E-mail: mari.pediatria@gmail.com
Received for publication: November 1, 2016
Accepted for publication: December 19, 2016













