Services on Demand
Article
Related links
Share
Revista Odonto Ciência (Online)
On-line version ISSN 1980-6523
Rev. odonto ciênc. (Online) vol.25 n.3 Porto Alegre Jul./Sep. 2010
CASE REPORT
The importance of early diagnosis and an accurate tumoral evaluation in the treatment of mandibular osteossarcoma
Importância do diagnóstico precoce e de uma precisa avaliação tumoral no tratamento de um osteossarcoma em mandíbula
André Luis Ribeiro RibeiroI,II,III; Rafaela Moutinho NobreIII; Sérgio de Melo Alves JuniorIV,V; Patricia de A. R. da Silva e SouzaVI,VII; Newton Guerreiro da Silva JúniorVIII; João de Jesus Viana PinheiroVI
IDepartment of Oral and Maxillofacial Surgery, School of Dentistry, University Center of Pará (CESUPA), Belém, PA, Brazil
IIDepartment of Oral and Maxillofacial Surgery, Hospital Metropolitano de Urgência e Emergência, Belém, PA, Brazil
IIIGraduate Program, School of Dentistry, Federal University of Pará (UFPA), PA, Belém, Brazil
IVDepartment of Oral and Maxillofacial Pathology ,School of Dentistry, Federal University of Pará (UFPA), Belém, PA, Brazil
VDepartment of Oral and Maxillofacial Pathology, School of Dentistry, University Center of Pará (CESUPA), Belém, PA, Brazil
VIDepartment of Endodontology, School of Dentistry, Federal University of Pará (UFPA), Belém, PA, Brazil
VIIDepartment of Endodontology, School of Dentistry, University Center of Pará (CESUPA), Belém, PA, Brazil
VIIIDepartment of Oral and Maxillofacial Surgery, School of Dentistry, Federal University of Pará (UFPA), Belém, PA, Brazil
ABSTRACT
PURPOSE: Osteosarcoma is a malignant bone neoplasm with aggressive clinical evolution which is usually diagnosed in late stages of the disease, when primary tumor reaches significant dimensions. In many cases, an aggressive surgical treatment, which includes major bone resection and is sometimes associated with radiotherapy and chemotherapy, is required for better control of local recurrence and metastasis in such lesions.
CASE DESCRIPTION: This paper reports an early-diagnosed case of osteosarcoma in the left side of the mandible and an accurate evaluation of the tumor involvement by means of Cone Beam Computerized Tomography.
CONCLUSION: The early diagnosis of osteosarcoma is an uncommon condition that has good influence both on the treatment and prognosis of such tumor. This early diagnosis and an accurate evaluation of the tumor involvement were determining factors for conservative, curative surgical procedure with minimum sequelae. The pericementary space should be especially observed, since its thickness is a much more common feature in osteosarcomas. Studies that allow for identifying osteosarcomas in earlier stages should be conducted in order to enable longer survival and better quality of life.
Key words: Osteosarcoma; oral pathology; oral cancer; early diagnosis; prognostic factor
RESUMO
OBJETIVO: O osteossarcoma é uma neoplasia maligna do osso que possui um comportamento clínico agressivo, geralmente diagnosticado em estados tardios da doença, quando o tumor primário atinge dimensões significativas. Em muitos casos, tratamento cirúrgico agressivo com grandes ressecções ósseas e a necessidade de associação à rádio ou quimioterapia se fazem necessários para melhor controle de recidivas locais e metástases em tais lesões.
DESCRIÇÃO DO CASO: No presente trabalho os autores relataram um caso de osteossarcoma na região de corpo e ramo mandibular esquerdo diagnosticado precocemente e avaliado de forma precisa pela tomografia computadorizada tipo cone beam.
CONCLUSÃO: O diagnóstico precoce do osteossarcoma é uma condição pouco comum que afeta de forma favorável tanto o tratamento quanto o prognóstico deste tumor. A associação deste diagnóstico precoce com uma avaliação precisa do envolvimento tumoral foram determinantes na execução de um tratamento cirúrgico conservador e ainda assim com finalidade curativa, com um mínimo de seqüelas. O espaço pericementário deve ser especialmente observado, pois seu espessamento é muito mais comum em osteossarcomas. Estudos que possibilitem identificar esta lesão de forma mais precoce e precisa devem realizados, a fim de possibilitar uma sobrevida maior com melhor qualidade de vida.
Palavras-chave: Osteossarcoma; patologia oral; câncer oral; diagnóstico precoce; fator de prognóstico
Introduction
The term osteosarcoma refers to a heterogeneous group of primary malignant mesenchymal neoplasms showing evidence of osteogenic material (1). Osteosarcoma is a rare neoplasia, usually located in the metaphysis of the long bones, with an estimated incidence of around 0.7 new cases for every 100,000 people, out of which only 10% affect the jaw (2).
The World Health Organization recognizes some variations of osteosarcoma, which differ in location, clinical presentation and level of cell atypia. The typical presentation is the central osteosarcoma, which can be subdivided into osteoblast, chondroblast or fibroblast types, depending on the predo- minant type of cell. In addition to this classification, central osteosarcoma can be differentiated from low-grade osteo- sarcoma, which has lower level of atypia and higher cellular differentiation, and from periosteal osteosarcoma (1).
Osteosarcoma of the jaw differs from the ones in long bones (3). The osteosarcoma of long bones tends to affect young individuals and cause early metastasis. As to the osteosarcoma in the buccal cavity, they have two different peaks of incidence. The first occurs in the individuals' second decade of life, and the other peak affects individuals after the age of 50. The osteosarcoma of the buccal cavity tends to present a lower cell atypia, and metastasis occurs at later stages of the disease. Local recurrence is the most frequent complication (4).
Clinically, osteosarcoma is defined as a fast-growing lesion, its main symptom being an increase in volume with an expansion of the buccal and lingual cortical bone in the overwhelming majority of cases (4-6). The most common radiographic pattern is that of bone resorption with pathologic bone deposition. Due to the fast growth of such pathologic bone, the trend is for bone deposition to occur in sequential lines at a 90º angle to the new bone formation. This image pattern is commonly described as "sun-ray periosteal reaction" (4).
Despite of the classical pattern described above, it is not always observed, thus making the differential diagnosis by radiographic images difficult. This condition offers the potential for misdiagnosis as benign condition, most specifically fibrous dysplasia (3), which is a lesion with distinct clinical features and prognosis.
The treatment of choice in oral osteosarcomas is surgical resection (4), which is the only treatment that can eliminate the disease. Obtaining positive surgical margins with no tumor commitment is one of the main factors for local control (2). However, obtaining free osseous margins by means of major resections was not sufficient for local control of the disease, soft tissue involvement being a significant prognostic factor in local recurrence.
Early osteosarcoma diagnosis is poorly reported and analyzed as a prognostic factor in the literature. Because of its fast growth, the majority of cases are diagnosed after the first symptoms appear, at an average time of 4 to 6 months. At this stage, the tumor is already well-developed and involving surrounding tissues, thus requiring aggressive surgical intervention and adjuvant therapies such as chemotherapy and radiotherapy for better local and metastasis control. The authors present a case of a jaw osteosarcoma diagnosed at a very early stage after complaints of pericoronitis. An accurate assessment of tumor involvement by Cone-Beam Computerized Tomography (CBCT) allowed for a precise surgery planning and a more conservative resection, thus preserving the mandible with quite favorable prognosis.
Case Description
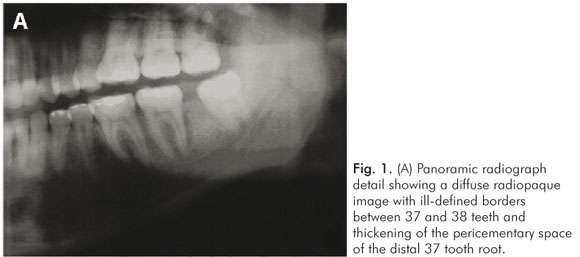
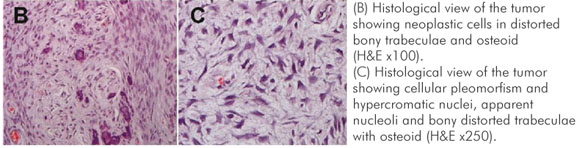
A 22-year-old healthy woman with a complaint of pain and swelling on the region of tooth 38 was evaluated and the clinical evaluation indicated a clinical situation compatible with pericoronitis. Clinical treatment was carried out for regression of the acute phase. A panoramic radiograph showed tooth 38 partially incrupted and 4 mm apart from tooth 37. The presence of a diffuse and ill-defined radiopaque area was observed, with abnormal bone trabeculate and enlargement of the pericementary space of the distal root of tooth 37 (Fig. 1A). Surgical extraction of tooth 38 was conducted and incisional biopsy of the pathologic tissue was obtained. In the postoperative period, the healing process followed a standard pattern. The oral mucosa healed normally and after 15 days post-surgery it showed normal clinical aspect with no sign of tumor involvement.
The histological findings revealed osteogenic neoplasm fragments characterized by high proliferation of cells featuring oval and spindle nuclear morphology and undefined limit cytoplasm. Pleomorphic and hyperchromatic cells were present, and varied numbers of nucleolus were also observed. Interlocked with these cells are calcified areas with distinct shapes and sizes that sometimes grow together. Also, an osteoid could be observed (Fig. 1B and 1C).
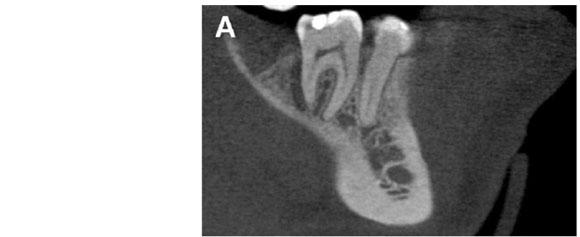
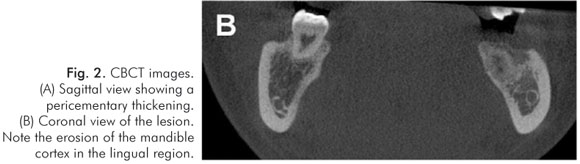
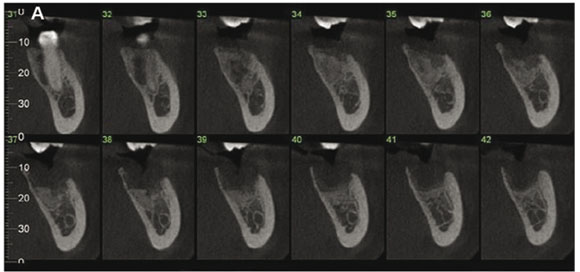
A CBCT examination was performed with axial cuts of the mandible to obtain a panoramic view (5.4 mm in thickness) and paraxial cuts (0.2 mm in thickness and 1mm distance increment). The sagittal cut CT scan examination revealed the presence of hyperattenuating images with imprecise limits in the region of teeth 38, increase in the pericementary space on the distal root of teeth 37 (Fig. 2A), and coronal cuts revealed lingual cortex invasions (Fig. 2B).
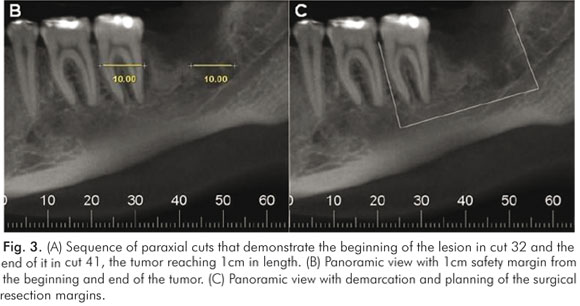
The sequence of paraxial tomographic cuts enabled the accurate assessment of the beginning and end of the lesion, the extension of which reached 1 cm (Fig. 3A). After establishing the boundaries of such lesion, the 1cm safety margin that was transferred for panoramic reconstruction can be set (Fig. 3B) and the ideal resection area can be planned (Fig. 3C).
The patient underwent segmental resection of the mandible involving a part of the left branch and mandible body partial body and branch of the left mandible (35x25 mm in length), including teeth 37 and the soft tissues around that region. The histological pattern observed was similar to that mentioned above, with free osseous margins and no involvement of surrounding tissues. The mandible base was maintained by preserving its pre-existing extension and occlusion. After 18 months of surgery, the patient showed no signs of local recurrence or metastasis (Fig. 4).
Discussion
Because osteosarcoma is a malignant bone tumor, being extremely rare in the jaw region, the development of longitudinal studies and other studies involving a large number of cases is difficult in dealing with osteosarcomas. Thus, any information, even from a single case, can provide an important scientific contribution.
Regarding sarcoma etiology, it is still indefinite, but morphologic and immunohistochemical trial studies suggest that most sarcoma cases stem from pluripontent mesenchymal cells that undergo differentiation in any type of cell during the neoplastic transformation process (7). By analyzing the factors related to the carcinogenesis of the osteosarcomas, those patients undergoing radiotherapy are observed to have a higher probability for neoplasm development (4), a situation that might be associated with a predisposing factor of the disease.
Early diagnosis is an important prognostic factor in the study of malignant neoplasia, a topic which is emphasized in the study of oral cancer (8). When the subject is osteosarcoma, early diagnosis is rarely discussed or included as a prognostic factor (4,9). Despite of some citations, the role of early diagnosis in treatment selection and results still require further studies. This condition can be explained by the clinical and biological behavior of the osteosarcoma, a fast-growing, painless lesion which has swelling as its main symptom upon diagnosis. At this stage, the tumor is well-developed and involving the surrounding tissues. In the case reported hereby an initial lesion was detected with minimal involvement of mandibular lingual cortex. Panoramic radiograph showed a diffuse radiopaque area that could be related to the majority kind of fibrous-osseous lesion of the mandible.
An important finding is the enlargement of the pericementary space appearing both in the panoramic and tomography images, and this condition has been associated to osteosarcoma (7). Enlargement of the periodontal ligament and radiographic pattern of periosteal reaction in the form of sun rays are the two image findings that could be used as differential in early diagnosis between the osteosarcomas and other fibrous-osseous lesions.
Asymptomatic cases of osteosarcoma diagnosed after routine panoramic radiographs are rare (7). In this case, a pericoronitis associated with the third molar was the reason why the patient sought treatment. However, it is not possible to determine whether the tumor had any relationship with the appearance of that symptom. Clinical course of pericoronitis and the appearance of the alveolar healing after tooth extraction developed without complications. Such condition could determine a minimum or no relationship between the symptoms and the lesion. Nevertheless, as previously explained, this relationship cannot be clearly identified.
Table 1 shows that most of the osteosarcoma cases are diagnosed in tumors with an average size equal to or bigger than 4.5 cm and average symptomatology time ranging up to several months. These findings cause the treatment to be varied according to a single author and in comparison to other authors. Due to the advanced tumor development stage, adjuvant therapies, such as radiotherapy and chemotherapy, are undertaken in order to provide a better local control, as free surgical margins are impossible to be obtained. In this case, the lesion was diagnosed as having a bigger diameter of 1cm after symptomatology related with pericoronitis and no volume increase, which is the most common symptom of mandibular osteosarcoma. A lesion with no symptoms associated with the tumor and 1 cm bigger extension, and when compared to cases reported in the literature, strengthens the condition of early diagnosis, as conducted in this case.
The treatment of choice for this case was segmental surgical resection of the mandible, involving the second molar and a part of the body and ramus of the left mandible. This more conservative procedure was possible because of the use of CBCT, which allowed for accurately determining the size of the tumor, assess the limits of invasion, and measure the extent of resection (7). The segmental resection was sufficient to obtain osseous margins without neoplastic cells, and the lack of invasion of surrounding tissues renders the adjuvant therapies, such as chemotherapy and radiotherapy, unnecessary.
Surgical resection is the best treatment of choice for tumor control, to be conducted whenever possible (3,5,10) and this was the treatment of the present case. The adjuvant therapies are not widely accepted in the literature, and should be considered in cases when complete resection cannot be achieved (11).
Conservative surgery provides better living quality to the patient because it reduces the necessity of complex reconstructive procedures in cases of wide resection as well as the side effects of radiotherapy and chemotherapy.
The early diagnosis of osteosarcoma is an uncommon condition that has good influence both on the treatment and prognosis of such tumor. Association between early diagnosis and an accurate evaluation of tumor extension provided for by the CBCT allow for a more precise and conservative surgical planning, still maintaining the healing objective through minimum sequelae. Osseous defects that suggest fibro-osseous lesions should be more closely evaluated in view of the similarity to the lesions observed in the osteosarcomas. The pericementary space should be especially observed, since its thickness is a much more common feature in osteosarcomas. Studies that allow for identifying osteosarcomas in earlier stages should be conducted in order to enable longer survival and better quality of life.
References
1. Schajowicz F. Histological Typing of Bone Tumours. 2 ed. Berlin: Springer-Verlag;1993. [ Links ]
2. Pellitteri PK, Ferlito A, Bradley PJ, Shaha AR, Rinaldo A. Management of sarcomas of the head and neck in adults. Oral Oncol 2003;39:2-12. [ Links ]
3. van Es RJJ, Keus RB, van der Waal I, Koole R, Vermey A. Osteosarcoma of the jaw bones: Long-term follow up of 48 cases. Int J Oral Maxillofac Surg 1997;26:191-7. [ Links ]
4. Bennett JH, Thomas G, Evans AW, Speight PM. Osteosarcoma of the jaws: A 30-year retrospective review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:323-32. [ Links ]
5. August M, Magennis P, Dewitt D. Osteogenic sarcoma of the jaws: factors influencing prognosis. Int J Oral Maxillofac Surg 1997;26:198-204. [ Links ]
6. Takahama Junior A, Alves FA, Pinto CAL, Carvalho AL, Kowalski LP, Lopes MA. Clinicopathological and immunohistochemical analysis of twenty-five head and neck osteosarcomas. Oral Oncol 2003;39:521-30. [ Links ]
7. Nakayama E, Sugiura K, Kobayashi I,Oobu K,Ishibashi H,Kanda S.The association between the computed tomography findings, histologic features, and outcome of osteosarcoma of the jaw. J Oral Maxillofac Surg 2005;63:311-8. [ Links ]
8. Petersen PE. Oral cancer prevention and control: The approach of the World Health Organization. Oral Oncol 2009;45: 454-60. [ Links ]
9. Granados-Garcia M, Luna-Ortiz K, Castillo-Oliva HA, Villavicencio Valencia V, Herrera-Gómez A, Mosqueda-Taylor A, et al. Free osseous and soft tissue surgical margins as prognostic factors in mandibular osteosarcoma. Oral Oncol 2006;42:172-6. [ Links ]
10. Mardinger O, Givol N, Talmi YP, Taicher S. Osteosarcoma of the jaw: The Chaim Sheba Medical Center experience. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;91:445-51. [ Links ]
11. Smeele LE, Kostense PJ, van der waal I, Snow GB: Effect of chemotherapy on survival of craniofacial osteosarcoma: A systematic review of 201 patients. J Clin Oncol 1997;15:363-7. [ Links ]
 Correspondence:
Correspondence:
André Luis Ribeiro Ribeiro
Avenida Marquês de Herval, 2359, Apt 1104
Belém-PA, Brazil
66085-310
Email: ribeiroalr@ig.com.br
Received: December 15, 2009
Accepted: June 22, 2010
Conflict of Interest Statement: The authors state that there are no financial and personal conflicts of interest that could have inappropriately influenced their work.