Services on Demand
Article
Related links
Share
Brazilian Journal of Oral Sciences
On-line version ISSN 1677-3225
Braz. J. Oral Sci. vol.14 n.2 Piracicaba Apr./Jun. 2015
ORIGINAL ARTICLE
Systemic and oral alterations associated with stress in nurses of public referral hospital
Danilo RodriguesI; Dagmar de Paula QueluzI
I Universidade de Campinas – UNICAMP, Piracicaba Dental School, Department of Community and Preventive Dentistry, Piracicaba, SP, Brazil
Abstract
Jobs that require great responsibility can cause serious damage to the body such as stress and its consequences. Stress can be one of the triggers of disease systemic and oral diseases in different professionals. Aim: To associate emotional stress with the systemic and oral alterations in the nurses of public referral hospital. Methods: All 60 nurses of both genders, with higher education level, different ethnicities and ages were invited to join this study. Nurses filled out the Inventory of Stress Symptoms for Adults (ISSL) and questionnaire of diseases/psychosomatic symptoms. Next, they were subjected to a stomatological examination of the oral cavity, according to the Boraks (1996) criteria. Stress was associated with most outstanding psychosomatic and oral variables by the Fisher's exact test for calculating the p value (0.05). Results: The sample was comprised of 37 nurses, most of them female (91.9%), young (83.7% are less than 36-years old), full range 22- 50 years old, white ethnicity (86.5%). The level of stress in level II (resistance) and III (exhaustion) was observed in 51.3% of the nurses. Symptoms of headache and gain of body weight lately were present in 48.6% of the nurses. With regard to oral alterations, 32.4% reported cold sore sometimes and 59.5% nibbled mucosa always. There was no significant association between the stress and psychosomatic and oral variables. Conclusions: Based on the results of this study it may be concluded that the nursing profession can lead to emotional stress, although no significant association between stress and disease/psychosomatic and oral symptoms was found. Future studies should be performed to evaluate this association.
Keywords: stress; occupational health; psychosomatic medicine; oral abnormalities.
Introduction
In analyzing an individual's needs as a whole, we should take into account his/her cultural universe and living conditions, i.e., his/her interaction with the environment and the reflection of this in everyday life.
According to Moreira (1985)1 and Arantes and Vieira (2002)2, the original concept of stress was introduced in 1936 by Hans Selye. From the 1980s, the number of jobs involving emotional stress increased significantly, possibly because of the very conditions of life and livelihood in big cities, but with its effects also being extended to smaller population groups, sometimes even specific as seen among students in test periods3-5.
The mental or psychological stress occurs daily in our lives. The ability to react physiologically and emotionally is a natural and necessary response. However, the heightened reactivity to mental stress identifies individuals at higher risk of developing hypertension and may cause cardiovascular events and sudden death6.
Nurses, bank employees and police officers as well as entrepreneurs are more exposed to factors that generate this kind of stress, which usually leads to a great intake of coffee, alcohol and tobacco. This fact usually favors the occurrence of circulatory, metabolic, immune or even emotional diseases contributing to an organic overload that produces emotional stress at different levels, according to the number of working hours, sector, and deal of responsibility7-8.
Considering the population as a whole, the frequency of systemic diseases directly or indirectly associated with emotional factors, may cause long bouts of tonsillitis at the start to more severe and difficult to control problems such as diabetes mellitus, hypertension and depression9-10.
Emotional stress in nurses due to the strain of everyday life can lead to risk of death for patients at their care, affecting this group of professionals not only psychologically but also generating serious health problems4,11-12. Allergy problems, asthma and cancer are linked to emotional factors. Traces of bitterness, sadness, depression and anger may be observed in people suffering from these diseases before organic manifestations become evident13.
With regard to oral lesions caused by stress, Godoy et al.9 (2005) reported canker sores, herpes simplex and nibbled mucosa. However, gingivitis is stands out with its multifactorial etiology. Despite being within a specific context, diseases and conditions related to general oral hygiene cannot be discarded because its etiology is associated with the immune system. The association between high levels of stress and changes in the oral mucosa has been reported in patients with immunosuppression resulting from a poor emotional status13.
The nursing professionals that are part of hospital medical staff in different functions subjected to stressful conditions of varying degrees by either superior demands or the operating area14-17. The body always tries to adapt to stress, using large amounts of adaptive energy for this18.
Several studies have investigated the impact of stress and Quality of Life at Work (QVT)12,19-27. The objective of the present study was to assess the association between emotional stress and systemic and oral alterations in nurses working at a public referral hospital in a Brazilian mid-sized city.
Material and methods
This cross-sectional, descriptive and quantitative study was approved by the Ethics Committee of the Piracicaba Dental School – UNICAMP (Protocol number 052/2013). The study was conducted in a public referral hospital with an installed capacity of 266 beds, located in Piracicaba - SP - Brazil, a mid-sized city of the southern region of Brazil.
The study population was the entire clinical nursing staff, consisting of 60 nurses of both genders, with higher education level, different ethnicities and ages, who signed an informed consent form, and responded to questionnaires. The data was collected between August and December 2013. The identity of the individuals was preserved.
Four instruments were used for data collection. The first was a questionnaire addressing the profile/demographic.information: age, gender, and ethnicity. The second was to obtain data of psychological character, with a selfadministered questionnaire on symptoms perceived by the respondent himself and applied for checking the level of stress (level I (alert), II (resistance), III (exhaustion)), according to the Lipp's Stress Symptoms Inventory for Adults (ISSL)28. The third was a self-administered questionnaire also referring to psychosomatic diseases or systemic symptoms, installed as a result of emotional stress. This instrument assessed organic and functional changes of neuro-endocrine-metabolic nature, caused by emotional stress, including diabetes mellitus, heart disease, depression, headache, weight gain, high blood pressure15,29-30. The fourth instrument consisted of an intraoral stomatological clinical examination performed by the researcher at the hospital31.
Data were statistically analyzed by descriptive and estimate analyses. The analyses were performed using SAS software version 9.1, using a significance level of 5% (p<0.05). The variable "stress" was classified as present or absent based on the existence of three levels/phases I (alert), II (resistance) and III (exhaustion), indicating presence of stress. The variable "psychosomatic events" (headache and weight gain) was classified as yes and no. The presence of cold sore, herpes and nibbled mucosa in the questionnaire was classified as always, never and sometimes, and then grouped into present (always or sometimes) or absent (never). These variables were combined to obtain the p-value by Fisher's exact test.
Results
From the total number of nurses, the final sample consisted of 37 (61.7%).
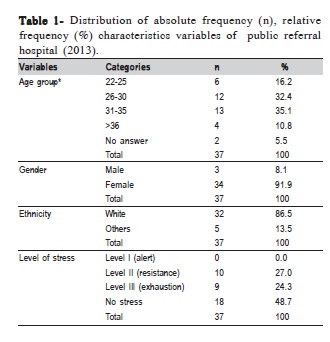
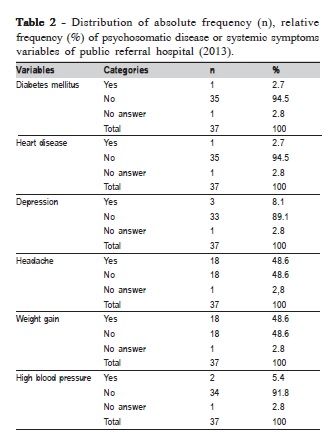
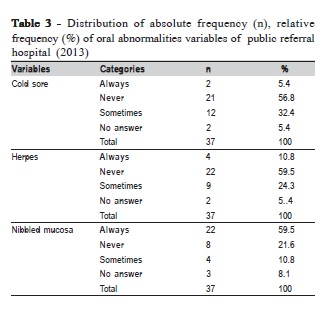
Tables 1-3 show the sample profile/stress level, the psychosomatic diseases or systemic symptoms, stomatological evaluation of the oral cavity (oral abnormalities), respectively. The most important data are: age group 31-35 (n=13, 35.1%), average 30.6 ± 5.59 years old, young (n=31, 83.7% are less than 36-years old), full range 22-50 years old, female predominance (n=34, 91.9%), white ethnicity (n=32, 86.5%), no stress (n=18, 48.7%), no diabetes mellitus (n=35, 94.5%), no heart disease (n=35, 94.5%), no depression (n=33, 89.1%). Considering headache, yes and no answers showed the same frequency (n=18, 48.6%). Yes and no answers showed the same frequency (n=18, 48.6%) for weight gain. No was the prevalent answer for high blood pressure (n=34, 91.85), never for cold sore (n=21, 56.8%), never for herpes (n=22, 59.5%), always for nibbled mucosa (n=22, 59.5%).
In tabulating the data and calculated the absolute and relative frequencies obtained: level II resistance (n=10, 27.0%), level III exhaustion (n=9, 24.3) (Table 1). However, 48.6% (n=18) reported having frequent headache as well; 48.6% (n=18) reported weight gain (Table 2). Sporadic presence of cold sore (sometimes) was observed in one group (n=12, 32.4%). Herpes was also another finding reported sometimes (n=9, 24.3%). Others (n=22, 59.5%) reported nibbled mucosa (Table 3).
Discussion
In the beginning, all 60 nurses were expected to participate. However, respecting the term of consent, only 37 nurses participated characterizing the sample. Considering the literature used for this study, several studies19,26-27,32 analyzed data from samples of similar size.
In this study, 91.9% of the participants were females with a mean age of 30 years. The female has a historical prevalence in nursing due to greater physical proximity to the patient and caregiver personality, as confirmed by several studies26-27,33. Similar work was carried out by Montes-Berges and Augusto-Landa27 (2014) reporting similar age and predominant proportion of females.
Considering the sample, emotional stress with 27.0% in level II (resistance) and 24.3% in level III (exhaustion) is a high stress level (total 51.3%). The hospital working environment involves many health professionals, with their different personalities, a fact that predisposes the emergence of emotional stress. Hooper et al.33 (2010) conducted a survey of emergency nurses and three other specialty units self selected to participate in a cross-sectional study. Participants completed a demographic profile and the professional quality of life, satisfaction, compassion and fatigue. About 82% of emergency nurses had moderate to high levels of burnout, and nearly 86% had moderate to high levels of fatigue. Differences between emergency nurses and those working in three other specialties: oncology, nephrology and intensive care, had the subscales: fatigue, satisfaction and compassion, but did not achieve a level of statistical significance. However, dozens of emergency nurses showed a risk to less compassion and satisfaction, while nurses in intensive care and oncology showed higher risk for burnout.
During the analysis of Stress Symptom18 in the present study, we observed the occurrence of symptoms of stress similar to those found by other authors when checking the items indicated in the Level II questionnaire26,32. The class of general nurses ends up being responsible for activities from the good reception of the patient and activities related to the handling, following his recovery or death to the end. This generates emotional and even professional instability. There are also the pressures due to the hierarchy of labor relations and the strong sense of charge both internal and external. Wright17 (2014) described that prolonged stress or work in situations where nurses feel trapped can cause stress levels that can have a lasting effect on health. The stressful condition caused by an imbalance between the demands placed on an individual and the resources he/she has available to deal with these demands. The requirements and the resources available to deal with are affected by skills, the individual thoughts and beliefs about himself/herself and work, available support structures and his/her personal life. The author concluded that managers have a duty to reduce stress in the workplace and provide structures and advice to ease and provide opportunities for nurses to regularly relax and relieve stress.
In the present study, it was observed that eating at work incorrectly or even due to stress, can lead to gained weight, where 48.6% said they had weight gain, 5.4% said they had high blood pressure, but taking proper medication. Han et al.15 (2011) conducted a survey of 2,103 female nurses in the United States and examined the relationship between working hours and stress associated with obesity. Stress at work and shift work are known risk factors for obesity. This finding was measured using the body mass index, and 55% of the sample reported being overweight. Factors such as nurse position, mental or emotional distress, behaviors and covariates related to the family were considered.
Regarding the oral alterations, 37.9% of the participants had some frequency of cold sore. Also, 35.1% said they had herpes at some point, and these two findings are commonly associated with immunosuppression and emotional stress. Similar data were also found by Lorette et al.34 (2006).
An abnormality usually associated with stress is the nibbled mucosa, which was present in this study in 70.3% of the cases. With respect to orofacial pain, 48.6% said they had headaches. Lacerda et al.35 (2008) investigated the prevalence of orofacial pain and its relation to absenteeism in workers of metallurgical and mechanical sector of the city of Xanxerê, SC, in the southern region of Brazil. Workers with severe pain reported higher absenteeism percentage (p<0.001), and the prevalence of orofacial pain was high in this population.
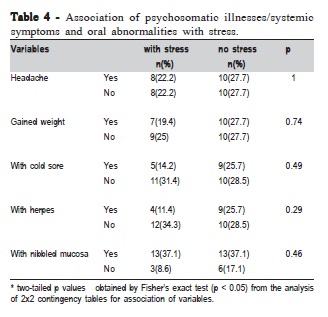
After general analysis of the results, Table 4 shows the most prominent associations between variables. Emotional stress was associated with headache and obesity as observed in other studies15,36. The same process was done with the variables cold sore, herpes and nibbled mucosa, aiming to calculate the p value10,37, but considering the sample size, the association was not considered statistically significant.
In view of the obtained and discussed data, there is need for further studies with larger samples in order to investigate possible association between emotional stress and systemic and oral diseases in nurses. Based on the results of this study, it may be concluded that the nursing profession can lead to emotional stress, although no significant association was found between stress and disease/ psychosomatic and oral symptoms. Future studies should be performed to evaluate this association.
References
1. Moreira MS. The stress syndrome. J Bras Med. 1985; 48; 19-32 Portuguese. [ Links ]
2. Arantes MAC, Vieira MJF. Stress: psychoanalytic clinic. São Paulo: Casa do Psicólogo; 2002 Portuguese.
3. Douglas CR. General pathophysiology. Mechanism disease. São Paulo: Robe; 2000. p. 827-85 Portuguese.
4. Silva MCM, Gomes, ARS. Occupational stress in health professionals: a study with portuguese doctor's and nurse practitioners. Estud Psicol. 2009; 14: 239-48 Portuguese.
5. Gibb J, Cameron IM, Hamilton R, Murphy E, Naji S. Mental health nurses' and allied health professionals' perceptions of the role of the Occupational Health Service in the management of work-related stress: how do they self-care? J Psychiatr Ment Health Nurs. 2010; 17: 838-45.
6. Nóbrega ACL, Castro RRT, Souza AC. Mental stress and systemic arterial hypertension. Rev Bras Hipertens. 2007; 14: 94-7 Portuguese.
7. Araújo TM, Aquino EM, Menezes GMS. Work psychosocial aspects and psychological distress among nurses. Rev Saude Publica. 2003; 37: 424- 33 Portuguese.
8. Lipp MEN , Malagris LEN. Stress management. In Range B, organizator. Behavioral and cognitive psychotherapy - research, practice, and application problems. Campinas: Psy II; 1995. p.279-92 Portuguese.
9. Godoy RNB, Nunes NA, Martinelli C, Lauris JRP, Nishidate SE. Evaluation of the buccal lesions caused for the emotional stress in camped patients and seated on the landless movement on the area of Promissão- SP. Rev ABO Nac. 2005; 13: 236-44 Portuguese.
10. Trombelli L, Farina R. A review of factors influencing the incidence and severity of plaque-induced gingivitis. Minerva Stomatol. 2013; 62: 207-34.
11. Montanholi LL, Tavares DMS, Oliveira GR. Stress: risk factors on hospital nurse's work. Rev Bras Enferm. 2006; 59: 661-5 Portuguese.
12. Wentzel D, Brysiewicz P. The consequence of caring too much: compassion fatigue and the trauma nurse. J Emerg Nurs. 2014; 40: 95-7.
13. Monti LM, Justi MM, Santos CT, Fajardo RS. Evaluation of the psychological and health conditions of patients with lichen planus. Rev Odontol Araçatuba. 2006; 27: 123-8 Portuguese.
14. Lipp M, organizator. Interpersonal relationships in the century XXI and the emotional stress. São Paulo: Sinopsys Editora; 2014 Portuguese.
15. Han K, Trinkoff AM, Storr CL, Geiger-Brown J. Job stress and work schedules in relation to nurse obesity. J Nurs Adm. 2011; 41: 488-95.
16. Anderson G, Hair C, Todero C. Nurse residency programs: an evidencebased review of theory, process, and outcomes. J Prof Nurs. 2012; 28: 203-12.
17. Wright K. Alleviating stress in the workplace: advice for nurses. Nurs Stand. 2014; 28: 37-42.
18. Lipp MEN, Guevara AJH. Empirical validation of the Inventory of Stress Symptoms (ISS). Estud Psicol. 1994; 11: 43-9 Portuguese.
19. Malagris LMN, Fiorito ACC. Stress level evaluation of technicians from the health area. Estud Psicol (Campinas). 2006; 23(4): 391-8 Portuguese.
20. Rossetti MO, Ehlers DM, Guntert IB, Leme IFAS, Rabelo ISA, Tosi SMVD, et al. Lipp's inventory of symptoms os stress for adults (ISSL) in federal civil servants of São Paulo. Rev Bras Ter Cogn. 2008, 4: 108-19 Portuguese.
21. Costa M, Accioly Jr H, Oliveira J, Maia E. Stress: diagnosis of military police personnel in a Brazilian city. Rev Panam Salud Publica. 2007; 21: 217-22 Portuguese.
22. Sadir MA, Bignotto MM, Lipp MEN. Stress and quality of life: the influence of some personal variables. Paideia. 2010; 20: 73-81 Portuguese.
23. Santos AFO, Cardoso CL. Mental health professionals: manifestation of stress and burnout. Estud Psicol. 2010; 27: 67-74 Portuguese.
24. Negeliskii C, Lautert L. Occupational stress and work capacity of nurses of a hospital group. Rev Latino-Am Enferm. 2011; 19: 606-13 Portuguese.
25. Moridi G, Khaledi S, Valiee S. Clinical training stress-inducing factors from the students' viewpoint: a questionnaire-based study. Nurse Educ Pract. 2014; 14: 160-3. 26.
26.Foureur M, Besley K, Burton G, Yu N, Crisp J. Enhancing the resilience of nurses and midwives: pilot of a mindfulness-based program for increased health, sense of coherence and decreased depression, anxiety and stress. Contemp Nurse. 2013; 45: 114-25.
27. Montes-Berges B, Augusto-Landa JM. Emotional intelligence and affective intensity as life satisfaction and psychological well-being predictors on nursing professionals. J Prof Nurs. 2014; 30: 80-8.
28. Lipp MEN. Inventory manual of stress symptoms Lipp (ISSL). São Paulo: Casa do Psicólogo; 2000. Portuguese.
29. Schmid OG. Stress. Induced endocrine and immunological changes in psoriasis patients and healthy controls. A preliminary study. Psychoter Psychosom. 1998; 67: 37-42.
30. Alves VLP, Lima DD, de Rivorêdo CRSF, Turato ER. Emotion and soma (dis)connected in magazine pages: the thematic categories of the prescriptive discourse on phenomena of life and illness. Cien Saude Colet. 2013; 18: 537-43 Portuguese.
31. Boraks S. Oral diagnosis. São Paulo: Artes Médicas; 1996. Portuguese.
32. McCabe TJ, Sambrook S. Psychological contracts and commitment amongst nurses and nurse managers: a discourse analysis. Int J Nurs Stud. 2012; 50: 954-67.
33. Hooper C, Craig J, Janvrin DR, Wetsel MA, Reimels E. Compassion satisfaction, burnout, and compassion fatigue among emergency nurses compared with nurses in other selected impatient specialities. J Emerg Nurs. 2010; 36: 420-7.
34. Lorette G, Crochard A, Minaud V, Wolkenstein P, Stalder JF, El Hasnaoui A. A survey on the prevalence of orofacial herpes in France: the instant Study. J Am Acad Dermatol. 2006; 55: 225-32.
35. Lacerda JT, Traebert J, Zambenedetti ML. Orofacial pain and absenteeism in workers of the metallurgic and mechanics industry. Saude Soc. 2008; 17; 182-91 Portuguese.
36. Schneider A, Wartner E, Schumann I, Hörlein E, Henningsen P, Linde K. The impact of psychosomatic co-morbidity on discordance with respect to reasons for encounter in general practice. J Psychosom Res. 2013; 74: 82-5.
37. Leentjens AF, Rundell JR, Wolcott DL, Guthrie E, Kathol R, Diefenbacher A. Reprint of: Psychosomatic medicine and consultation-liaison psychiatry: scope of practice, processes, and competencies for psychiatrists working in the field of CL psychiatry or psychosomatics. A consensus statement of the European Association of Consultation-Liaison Psychiatry and Psychosomatics (EACLPP) and the Academy of Psychosomatic Medicine (APM). J Psychosom Res. 2011; 70: 486-91.
 Correspondence:
Correspondence:
Dagmar de Paula Queluz
Departamento de Odontologia Social
Faculdade de Odontologia de Piracicaba - UNICAMP
Avenida Limeira, 901, CEP: 13414 900
Piracicaba, SP, Brasil
E-mail: dagmar@fop.unicamp.br
Received for publication: May 04, 2015
Accepted: June 26, 2015













