Services on Demand
Article
Related links
Share
RSBO (Online)
On-line version ISSN 1984-5685
RSBO (Online) vol.14 n.1 Joinville Jan./Mar. 2017
Case Report Article
Surgical correction of vertical maxillary excess associated with mandibular self-rotation
Michelle Nascimento Meger I; Fernanda Tiboni I; Felipe Silvério dos Santos I; Thalyta Verbicaro I; Tatiana Miranda Deliberador II; Rafaela Scariot II; Gleisse Wantowski III
I Post-graduation in Dentistry, Positivo University – Curitiba – PR – Brazil
II Post-graduation and graduation Program, Positivo University – Curitiba – PR – Brazil
III Specialization in Oral Maxillofacial Surgery, Positivo University – Curitiba – PR – Brazil
ABSTRACT
Introduction: The Class I skeletal deformity associated with vertical maxillary excess is a rare condition reported in the literature. Surgical impaction allows the correction of the long face and gummy smile. Objective: This case report aimed to evaluate the positioning of the condyle after Le Fort I osteotomy associated with mandibular selfrotation. Case report: The patient underwent orthognathic surgery for the correction of maxillary vertical excess. Tomography studies were performed to evaluate the initial and final position of the condyle. The patient improved mastication, breathing and phonetics, with esthetic benefit. Conclusion: After the Le Fort I osteotomy and mandibular self-rotation, the condyle remained stable occupying a new anterior-superior position in the glenoid fossa and patient's TMJ remained asymptomatic after 9 months of postoperative follow-up.
Keywords: orthognathic surgery; osteotomy Le Fort; temporomandibular joint.
Introduction
The orthognathic surgery is a procedure that aims at improvement of masticatory function, esthetic harmony and structural balance 1,3,4. The first Le Fort I osteotomy for correction of malocclusion was introduced by Wassmund in 1927. He performed a partial mobilization of the maxilla. Obwegeser was the first to mobilize the jaw fully, allowing sagittal and vertical adjustment. Bell, Epker and Wolford continued the development of the "down fracture" technique that made possible the mobility of the jaw for all regions 12. The Le Fort I osteotomy for the upper jaw repositioning is the most used for correction of vertical maxillary excess 14.
The surgical jaw impaction allows correction of the gingival smile, long face syndrome, certain types of skeletal open bite and labial sealing 12. The maxillary impaction results in self-rotation of the jaw, first described by Schendel and collaborators, in 1976; Bell and collaborators, in 1977 and Fish and collaborators, in 1978; such self-rotation is accompanied by skeletal and soft tissue changes observed in sagittal advance and vertical shortening of the lower face 5,12.
In facial analysis, the vertical maxillary excess has the following characteristics: elongated lower third of the face, relative to the upper and middle thirds; exaggerated display of upper incisors at rest; lip incompetence; tendency of type class II malocclusion, with or without open bite and marked gummy smile 9,10. The nose is elongated, the alar bases are narrow and the zygomatic are generally plane. The lower third of the face is long, resulting in a retrognathic appearance of the jaw 2.
The correction of the vertical problems with or without open bite usually involves mandibular deficiency associated with Le Fort I osteotomy for maxillary replacement with self-rotation of the mandible 11,13. The sagittal advancement of the mandible is especially favorable in patients with mandibular deficiency 13.
After the surgery of the maxillary impaction, the mandible self-rotates to a new anterior and superior position towards the original position. The magnitude of the rotation is an integral part of the treatment planning process 8.
The objective of this case report was to evaluate the positioning of the condyle after Le Fort I osteotomy associated the mandibular self-rotation to correct the vertical excess of the maxilla.
Case report
Patient C.C.S., female, aged 28 years, attended to the Oral and Maxillofacial Surgery and Traumatology Department of the Positivo University complaining about the esthetics of face long, gummy smile and difficulty of labial sealing.
The patient was subjected to previous orthodontic treatment for the alignment and leveling of the arches, correction of the left crossbite and extraction of maxillary and mandibular third molars to aid in the orthognathic surgery.
The extraoral clinical exam revealed at the frontal view the long face because of the predominantly vertical growth; with lip incompetence, excessive exposure of the vermilion of the lower lip, no facial asymmetry and gummy smile (figure 1).

The examination of the vertical proportions revealed an increase in the heights of the middle and lower third of the face contributing to an increased exposure of teeth and gums. In the lateral view, the patient has mandibular retrognathism, convex profile, shortened chin-neck distance, poor defined lower edge of the mandible and increased facial height.
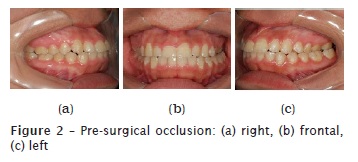
The intraoral examination showed right Class I molar relation; left posterior crossbite; and 1 mm maxillary midline deviation to the right (figure 2).
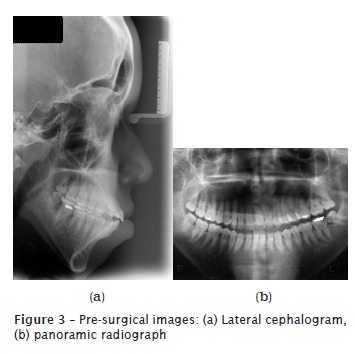
On the lateral cephalogram, we observed the vertical excess of the maxilla associated with lip incompetence. The panoramic radiograph revealed the presence of third molars and the clinical treatment to be performed prior to surgery (figure 3).
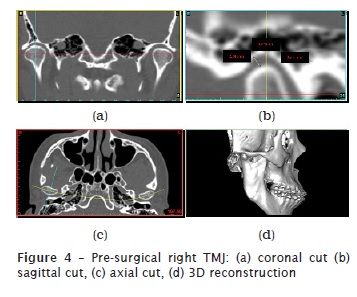
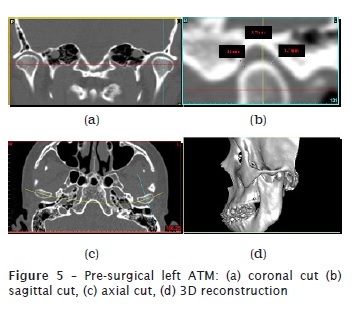
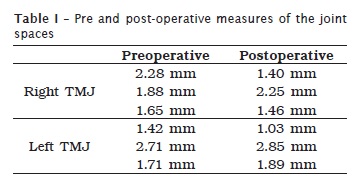
The reconstruction was achieved through the dycons sent from the orthodontic documentation using VistaDent 3D software (Compass3D®). On the preoperative CT, we measured three points from the condyle to the mandibular fossa. On the sagittal cut of the temporomandibular joint (TMJ), the following measures were obtained: right – 2.28 mm, 1.88 mm and 1.65 mm; and left – 1.42 mm, 2.71 mm and 1.71 mm (figures 4 and 5). The patient did not present articular symptoms.
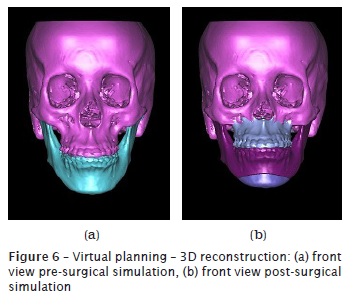
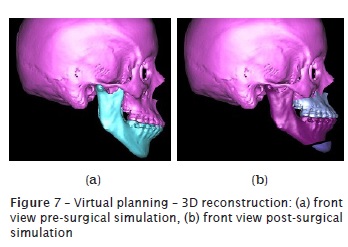
In this case, through virtual planning, we planned: Le Fort I osteotomy for impaction of 10 mm and advancement of 5 mm, in teeth #11 and #21; impaction of 6.5 mm, in the region of teeth #16 and #26; and mentoplasty for advancement of 8 mm associated with the mandibular self-rotation, with pre-and post-surgical orthodontics (figures 6 and 7). The treatment goal was to achieve racial harmony and condyle stability. The removal of third molars and the clinical management were performed before surgery.
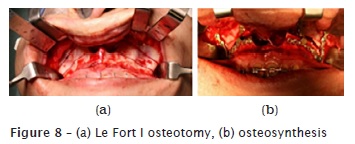
Surgically, Le Fort I osteotomy was performed using piezoelectric device for 10 mm impaction of the maxilla and 5 mm advancement in the region of teeth #11 and #21; 6.5 mm impaction in teeth #16 and #26, and mentoplasty was executed with reciprocating saw for 8 mm advancement. For osteosynthesis of the maxilla, we used two 1.5 mm pre-molded L-shaped plates with four holes, positioned on the zygomatic pillars, and two Le Fort plates with 11 holes; for mentoplasty, we used the advancement plate with five holes. Alar loop technique was used to control the width of the alar base and the closing of the vertical V-Y portion to increase the exposure of the upper lip vermillion (figure 8).
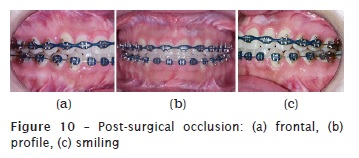
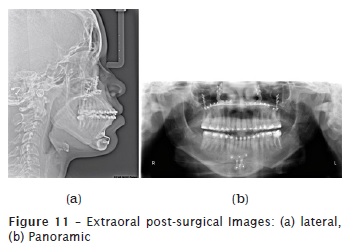
The orthodontic treatment was continued 60 days after surgery, after bone repair and stability of the surgical movement. Extra- and intraoral images of postoperative following-up and radiographic examinations are seen in figures 9, 10 and 11.

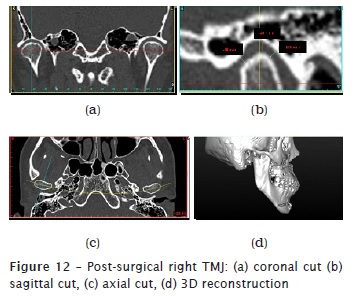
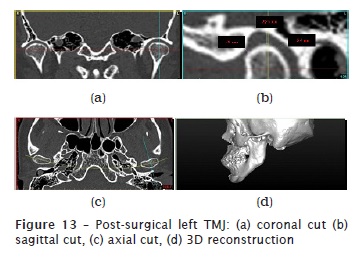
The postoperative CT was performed 6 months after surgery, and the measures taken from the right TMJ were 1.40 mm, 2.25 mm and 1.46 mm and from the left side were 1.03 mm, 2.85 mm and 1.89 mm (figures 12 and 13). Comparing the pre-and post-operative measures, we noted that the condyle self-rotated, occupying a new anterior-upper position on the mandibular fossa (table I).
Discussion
In the literature, many areas of the condyle were considered for the study of the positioning on the mandibular fossa during the self-rotation of the mandible after surgery of maxillary impaction. Fish et al. 4 used the top of the condyle as rotation center to pre-surgical prediction. Sperry et al. 11 found that the rotation center of the mandible during impaction of the maxilla is in the mastoid process, noting that two edentulous patients with the Reuleaux method 7,8,13.
Bryan 1 reported a study with 15 individuals, in 1994, concluding that there were no significant differences among the three prediction methods with different centers of mandibular self-rotation 12,13.
Nattestad and Vedtofte 7 noted 10 cases treated by Le Fort I osteotomy without mandibular surgery, to find the center of rotation of the mandibular self-rotation, which was determined later in the analysis of pre- and post-operative lateral cephalograms. The results showed a great individual variation in the centers of rotation of the mandible.
Rekow et al. reported that after the surgery of the maxillary impaction, the mandible self-rotates to a new anterior and superior position towards the original position. In this case report, the CT analysis revealed that the mandible's condyle after self-rotation occupied a new anterior and superior position. The patient remained asymptomatic during the pre-and postoperative treatment, indicating that the new position of the mandible's condyle was not compressing the articular disc, innervated structures and was positioned in the mandibular fossa.
In some cases, after the upper maxillary repositioning, it is necessary to perform the maxillary advancement when the mandibular self-rotation is not sufficient for the fitting of Angle Class I malocclusion 6. If the mandible is slightly retroposed, the mandibular self-rotation is favorable 5. In the present case, the planning of maxilla impaction associated with the mandible self-rotation resulted in a stable Class I canine and molar relationship.
Conclusion
After Le Fort I osteotomy and mandibular self-rotation, the condyle remained stable occupying a new anterior-superior position in mandibular fossa. At 9-month postoperative follow-up, the patient remained asymptomatic with respect to TMJ and the tooth occlusion remained stable.
References
1. Bryan DC. An investigation into the accuracy and validity of three points used in the assessment of autorotation in orthognathic surgery. Br J Oral Maxillofac Surg. 1994 Dec;32(6):363-72. [ Links ]
2. Cardoso MA, Bertoz FA, Capelozza Filho L. Características cefalométricas do padrão face longa. R Dental Press Ortodon Ortop Facial. 2005 Mar/Apr;10(2):29-43.
3. Cherackal GJ, Thomas E, Prathap A. Combined orthodontic and surgical approach in the correction of a class III skeletal malocclusion with mandibular prognathism and vertical maxillary excess using bimaxillary osteotomy. Case Rep Dent. 2013;2013:797846.
4. Fish LC, Wolford LM, Epker BN. Surgical-orthodontic correction of vertical maxillary excess. Am J Orthod. 1978 Mar;73(3):241-57.
5. Jamilian A, Showkatbakhsh A, Gholami D, Kamali Z. The relation between pogonion advancement and posterior maxillary impaction. J Craniofac Surg. 2009 May;20(3):841-3..
6. Laureano Filho JR, Silva EDO, Vasconcellos RJH, Silva LCF, Rocha NS. Alterações estéticas em discrepâncias ântero-posteriores na cirurgia ortognática. Rev Cir Traumatol Buco-Maxilo-Fac 2005 Jan/Mar;5(1):45-52.
7. Nattestad A, Vedtofte P. Mandibular autorotation in orthognathic surgery: a new method of locating the centre of mandibular rotation and determining its consequence in orthognathic surgery. J Craniomaxillofac Surg. 1992 May/Jun;20(4):163-70.
8. Rekow ED, Speidel TM, Koenig RA. Location of the mandibular center of autorotation in maxillary impaction surgery. Am J Orthod Dentofacial Orthop. 1993 Jun;103(6):530-6.
9. Schendel SA, Eisenfeld J, Bell WH, Epker BN, Mishelevich DJ. The long face syndrome: vertical maxillary excess. Am J Orthod. 1976 Oct;70(4):398-408.
10. Schendel SA, Carlotti Jr. AE. Variations of total vertical maxillary excess. J Oral Maxillofac Surg. 1985 Aug;43(8):590-6.
11. Sperry TP, Steinberg MJ, Gans BJ. Mandibular movement during autorotation as a result of maxillary impaction surgery. Am J Orthod. 1982 Feb;81(2):116-23.
12. Steinhäuser S, Richter U, Richter F, Bill J, Rudzki-Janson I. Profile changes following maxillary impaction and autorotation of the mandible. J Orofac Orthop. 2008 Jan;69(1):31-41.
13. Wang YC, Ko EW, Huang CS, Chen YR. The inter-relationship between mandibular autorotation and maxillary LeFort I impaction osteotomies. J Craniofac Surg. 2006 Sep;17(5):898-904.
14. Zarrinkelk HM, Throckmorton GS, Ellis E 3rd. Functional and morphologic alterations secondary to superior repositioning of the maxilla. J Oral Maxillofac Surg. 1995 Nov;53(11):1258-67.
 Corresponding author:
Corresponding author:
Michelle Nascimento
Meger Rua Maranhão, 2146, apto. 301 – Portão
CEP 80610-001 – Curitiba
Paraná – Brasil
E-mail: michellemeger@hotmail.com
Received for publication: January 22, 2017
Accepted for publication: February 13, 2017